Anesth Pain Med.
2021 Jul;16(3):258-265. 10.17085/apm.21021.
A retrospective comparison for prediction of optimal length of right subclavian vein catheterization in infants: landmark-based estimation vs. linear regression model
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Chungnam National University Hospital, Daejeon, Korea
- 2Department of Anesthesiology and Pain Medicine, College of Medicine, Chungnam National University, Daejeon, Korea
- 3Department of Pediatrics, Chungnam National University Hospital, Daejeon, Korea
- KMID: 2519054
- DOI: http://doi.org/10.17085/apm.21021
Abstract
- Background
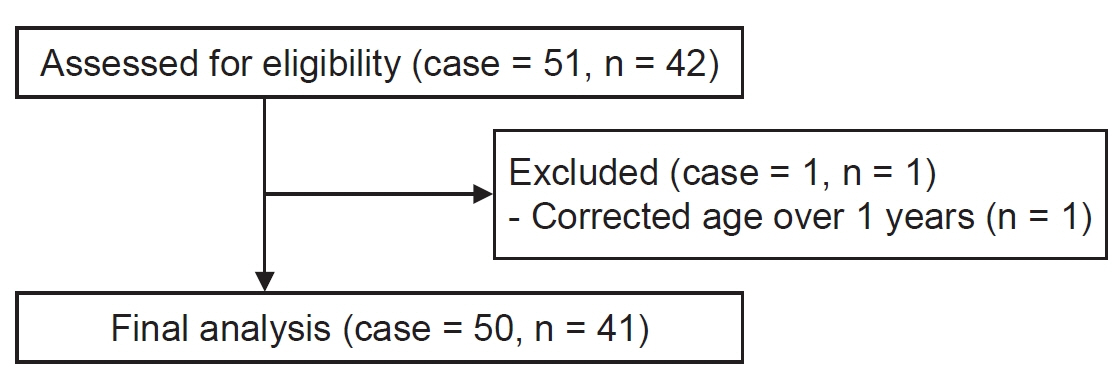
The optimal insertion length for right subclavian vein catheterization in infants has not been determined. This study retrospectively compared landmark-based and linear regression model-based estimation of optimal insertion length for right subclavian vein catheterization in pediatric patients of corrected age < 1 year.
Methods
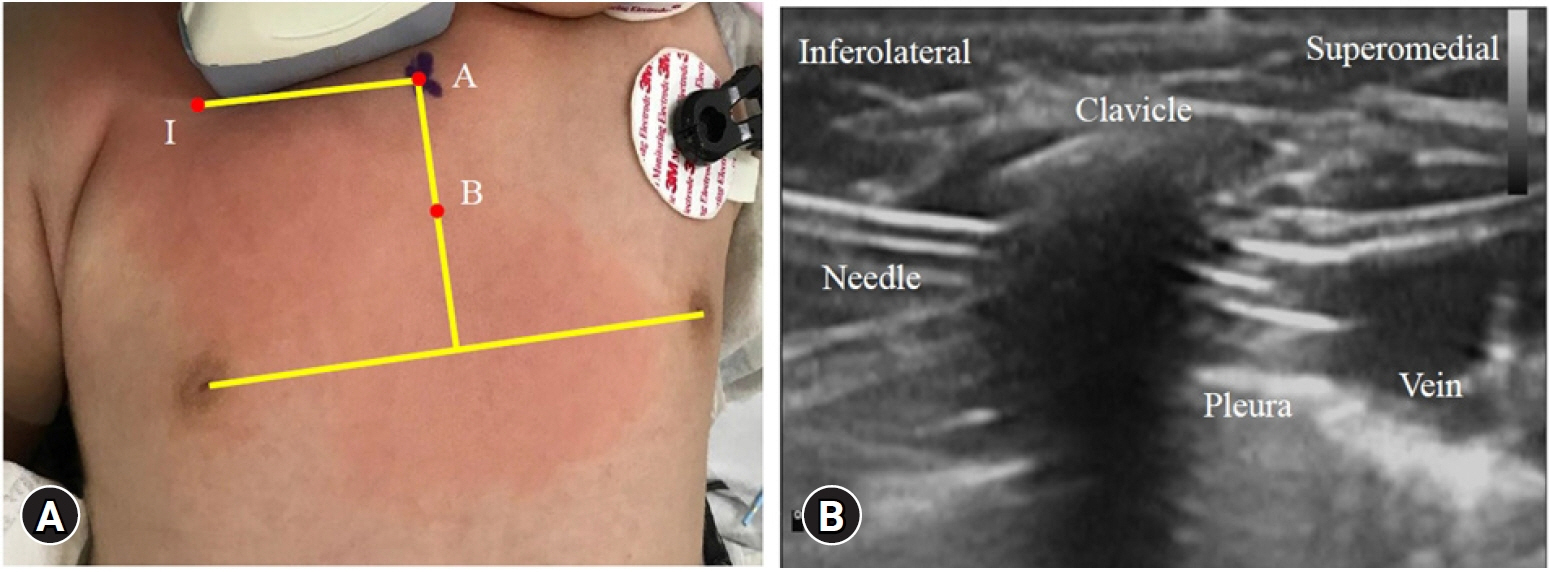
Fifty catheterizations of the right subclavian vein were analyzed. The landmark related distances were: from the needle insertion point (I) to the tip of the sternal head of the right clavicle (A) and from A to the midpoint (B) of the perpendicular line drawn from the sternal head of the right clavicle to the line connecting the nipples. The optimal length of insertion was retrospectively determined by reviewing post-procedural chest radiographs. Estimates using a landmark-based equation (IA + AB – intercept) and a linear regression model were compared with the optimal length of insertion.
Results
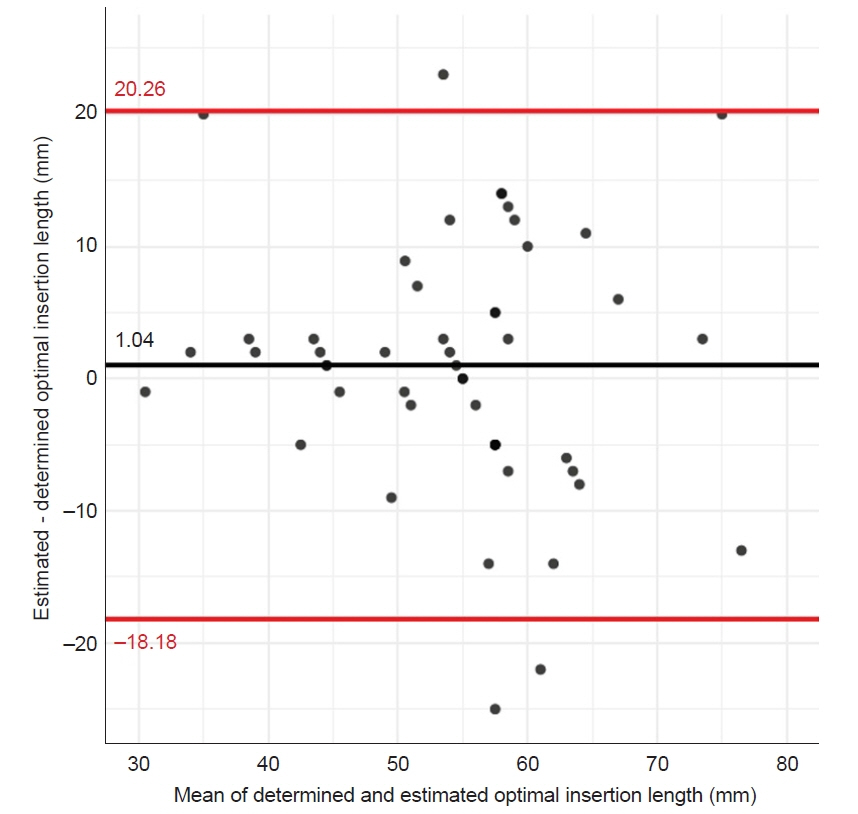
A landmark-based equation was determined as IA + AB – 5. The mean difference between the landmark-based estimate and the optimal insertion length was 1.0 mm (95% limits of agreement –18.2 to 20.3 mm). The mean difference between the linear regression model (26.681 – 4.014 × weight + 0.576 × IA + 0.537 × AB – 0.482 × postmenstrual age) and the optimal insertion length was 0 mm (95% limits of agreement –16.7 to 16.7 mm). The difference between the estimates using these two methods was not significant.
Conclusion
A simple landmark-based equation may be useful for estimating optimal insertion length in pediatric patients of corrected age < 1 year undergoing right subclavian vein catheterization.
Figure
Reference
-
1. Ares G, Hunter CJ. Central venous access in children: indications, devices, and risks. Curr Opin Pediatr. 2017; 29:340–6.2. Citak A, Karaböcüoğlu M, Uçsel R, Uzel N. Central venous catheters in pediatric patients – subclavian venous approach as the first choice. Pediatr Int. 2002; 44:83–6.3. Brass P, Hellmich M, Kolodziej L, Schick G, Smith AF. Ultrasound guidance versus anatomical landmarks for subclavian or femoral vein catheterization. Cochrane Database Syst Rev. 2015; 1:CD011447.4. Pirotte T, Veyckemans F. Ultrasound-guided subclavian vein cannulation in infants and children: a novel approach. Br J Anaesth. 2007; 98:509–14.5. Park SI, Kim YH, So SY, Kim MJ, Kim HJ, Kim JK. Ultrasound-guided subclavian catheterization in pediatric patients with a linear probe: a case series. Korean J Anesthesiol. 2013; 64:541–4.6. Kim KO, Jo JO, Kim HS, Kim CS. Positioning internal jugular venous catheters using the right third intercostal space in children. Acta Anaesthesiol Scand. 2003; 47:1284–6.7. Andropoulos DB, Bent ST, Skjonsby B, Stayer SA. The optimal length of insertion of central venous catheters for pediatric patients. Anesth Analg. 2001; 93:883–6.8. Na HS, Kim JT, Kim HS, Bahk JH, Kim CS, Kim SD. Practical anatomic landmarks for determining the insertion depth of central venous catheter in paediatric patients. Br J Anaesth. 2009; 102:820–3.9. Choi YJ, Hahm KD, Kwon K, Lee EH, Ro YJ, Yang HS. [Bedside prediction of right subclavian venous catheter insertion length]. Rev Bras Anestesiol. 2014; 64:419–24. Portuguese.10. Yoon SZ, Shin JH, Hahn S, Oh AY, Kim HS, Kim SD, et al. Usefulness of the carina as a radiographic landmark for central venous catheter placement in paediatric patients. Br J Anaesth. 2005; 95:514–7.11. Engle WA; American Academy of Pediatrics Committee on Fetus and Newborn. Age terminology during the perinatal period. Pediatrics. 2004; 114:1362–4.12. Giavarina D. Understanding Bland Altman analysis. Biochem Med (Zagreb). 2015; 25:141–51.13. Kang SS, Shin YS, Lee SY, Kim H. Simplified equation for determining proper depth of peripherally inserted central catheter in relation to anatomical landmarks. Korean J Anesthesiol. 2018; 71:300–4.14. Yoon SZ, Shin TJ, Kim HS, Lee J, Kim CS, Kim SD, et al. Depth of a central venous catheter tip: length of insertion guideline for pediatric patients. Acta Anaesthesiol Scand. 2006; 50:355–7.15. Kim H, Jeong CH, Byon HJ, Shin HK, Yun TJ, Lee JH, et al. Predicting the optimal depth of left-sided central venous catheters in children. Anaesthesia. 2013; 68:1033–7.16. Bannon MP, Heller SF, Rivera M. Anatomic considerations for central venous cannulation. Risk Manag Healthc Policy. 2011; 4:27–39.17. Vesely TM. Central venous catheter tip position: a continuing controversy. J Vasc Interv Radiol. 2003; 14:527–34.18. III. NKF-K/DOQI clinical practice guidelines for vascular access: update 2000. Am J Kidney Dis. 2001; 37(1 Suppl 1):S137–8.19. Booth SA, Norton B, Mulvey DA. Central venous catheterization and fatal cardiac tamponade. Br J Anaesth. 2001; 87:298–302.20. Sasaki TM, Panke TW, Dorethy JF, Lindberg RB, Pruitt BA. The relationship of central venous and pulmonary artery catheter position to acute right-sided endocarditis in severe thermal injury. J Trauma. 1979; 19:740–3.21. Huang YC, Huang JC, Chen SC, Chang JM, Chen HC. Lethal cardiac arrhythmia during central venous catheterization in a uremic patient: a case report and review of the literature. Hemodial Int. 2013; 17:644–8.22. Dwivedi S, Siddiqui F, Patel M, Cardozo S. Guide wire induced cardiac tamponade: the soft J tip is not so benign. Case Rep Crit Care. 2016; 2016:1436924.23. Cavatorta F, Campisi S, Fiorini F. Fatal pericardial tamponade by a guide wire during jugular catheter insertion. Nephron. 1998; 79:352.24. Dube SK, Chaturvedi A. A simple technique to avoid difficulty in guide wire insertion during pediatric central venous cannulation. Saudi J Anaesth. 2014; 8:141–2.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Optimal Length of Central Venous Catheterization Using 3-Dimensional Multi-Detector Row Computed Tomography
- Which Position is Ideal for Subclavian Venous Catheterization?
- Ultrasound-Guided Subclavian Vein Catheterization
- Subclavian vein occlusion and massive upper extremity edema : A complication of subclavian vein catheterization
- Incidental ipsilateral subclavian vein catheterization via right internal jugular venous route: A case report