Neurointervention.
2021 Jul;16(2):185-189. 10.5469/neuroint.2021.00080.
Vertebral Artery Dissecting Aneurysm Causing Central Tapia’s Syndrome: A Case Report
- Affiliations
-
- 1Department of Neurosurgery, Busan Paik Hospital, Inje University College of Medicine, Busan, Korea
- 2Department of Neurosurgery, Kosin University Gospel Hospital, Kosin University College of Medicine, Busan, Korea
- 3Department of Diagnostic Radiology, Busan Paik Hospital, Inje University College of Medicine, Busan, Korea
- 4Department of Neurosurgery, Haeundae Paik Hospital, Inje University College of Medicine, Busan, Korea
- 5Department of Endocrinology, Haeundae Paik Hospital, Inje University College of Medicine, Busan, Korea
- KMID: 2517746
- DOI: http://doi.org/10.5469/neuroint.2021.00080
Abstract
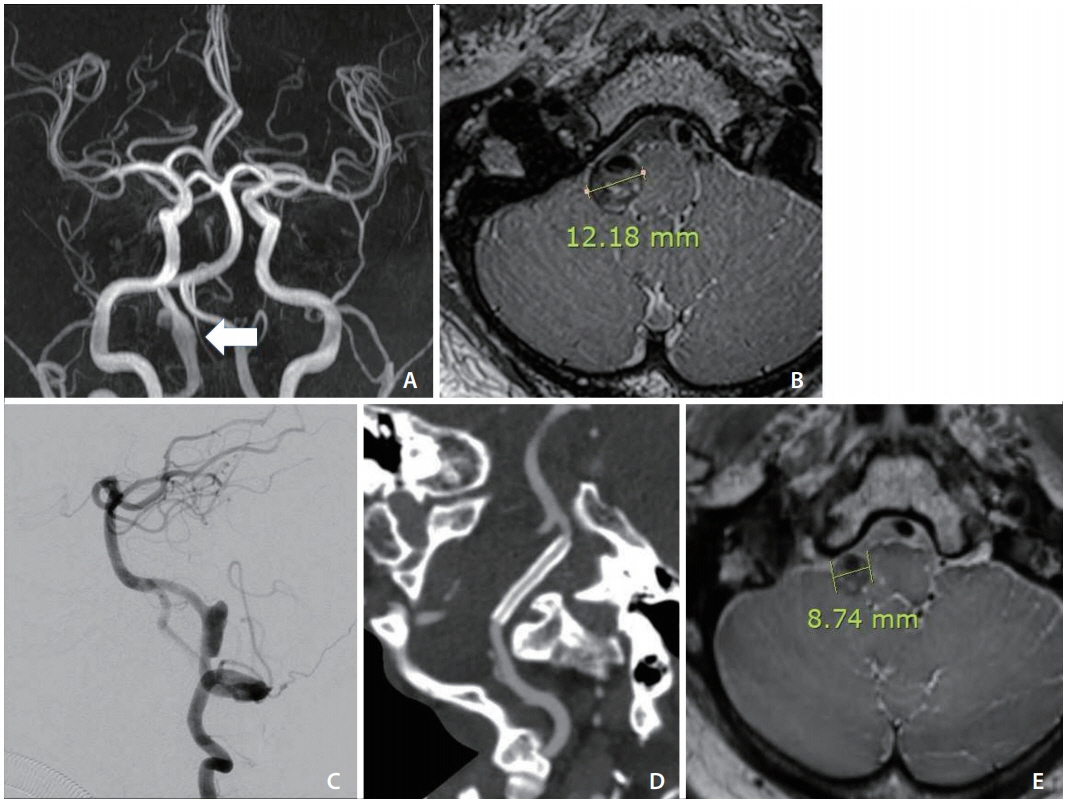
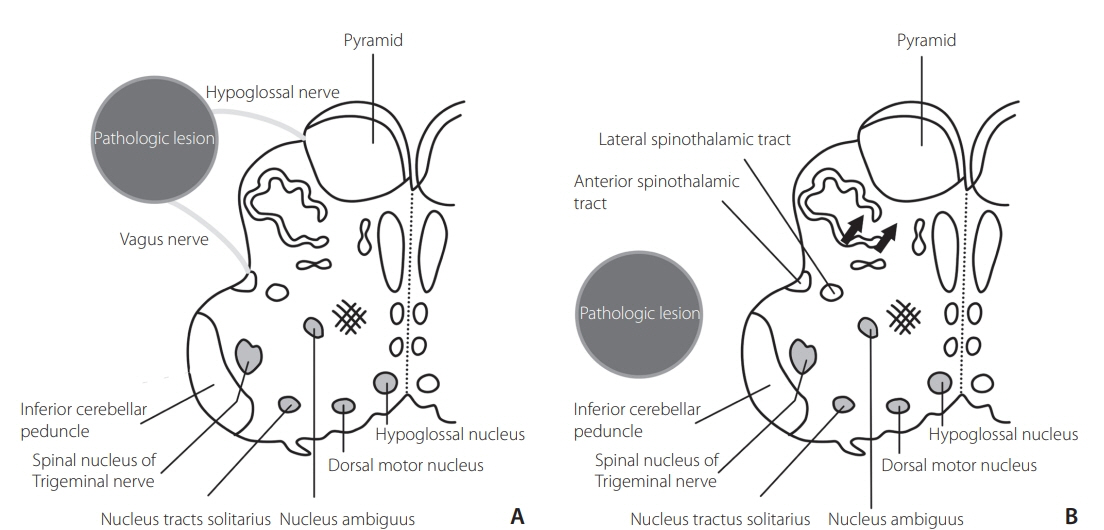
- The central type of Tapia’s syndrome is an extremely rare presentation, characterized by unilateral paralysis of the vagal and hypoglossal nerves, contralateral hemiparesis, or hemihypesthesia. This report describes a case of a middle-aged patient who developed central Tapia’s syndrome due to a right vertebral artery dissecting aneurysm (VADA). The patient complained about swallowing difficulty and odynophagia. Right vocal cord paralysis, mild tongue deviation to the right side, left hypesthesia, and decreased temperature sensation with left hemiparesis were observed in neurologic exams. A right VADA and compression of the medulla oblongata due to the VADA were diagnosed on magnetic resonance imaging. Endovascular flow diversion of the right VADA was performed. After 1 year, all neurological symptoms and vocal cord paralysis were nearly resolved, but left hypesthesia remained with decreased nociception. We present and discuss how a VADA caused those symptoms and propose endovascular flow diversion as a treatment option.
Keyword
Figure
Reference
-
1. Tapia AG. [A new syndrome; few cases of hemiplegia larynx and language with or without sterone-crypto-palsy. Mastoid and trapeze]. Arch Int Laryngol Otol Rhinol. 1906; 22:780–785. French.2. Al-Sihan M Jr, Schumacher M, Löhle E. Tapia syndrome caused by a vertebral artery dissection. Ear Nose Throat J. 2011; 90:313–314.
Article3. Andrioli G, Rigobello L, Mingrino S, Toso V. Tapia’s syndrome caused by a neurofibroma of the hypoglossal and vagus nerves: case report. J Neurosurg. 1980; 52:730–732.4. de Freitas MR, Nascimento OJ, Chimelli L. Tapia’s syndrome caused by Paracoccidioidis brasiliensis. J Neurol Sci. 1991; 103:179–181.
Article5. Shimohata T, Nakano R, Sato S, Tsuji S. [A patient with aneurysm of extracranial internal carotid artery presenting lower cranial polyneuropathy similar to Tapia’s syndrome]. Rinsho Shinkeigaku. 1994; 34:707–711. Japanese.6. Boisseau N, Rabarijaona H, Grimaud D, Raucoules-Aimé M. Tapia’s syndrome following shoulder surgery. Br J Anaesth. 2002; 88:869–870.
Article7. Krasnianski M, Neudecker S, Schlüter A, Krause U, Winterholler M. Central Tapia’s syndrome (“matador’s disease”) caused by metastatic hemangiosarcoma. Neurology. 2003; 61:868–869.
Article8. Sotiriou K, Balanika M, Anagnostopoulou S, Gomatos C, Karakitsos D, Saranteas T. Postoperative airway obstruction due to Tapia’s syndrome after coronary bypass grafting surgery. Eur J Anaesthesiol. 2007; 24:378–379.
Article9. Tesei F, Poveda LM, Strali W, Tosi L, Magnani G, Farneti G. Unilateral laryngeal and hypoglossal paralysis (Tapia’s syndrome) following rhinoplasty in general anaesthesia: case report and review of the literature. Acta Otorhinolaryngol Ital. 2006; 26:219–221.10. Chun DH, Kim ST, Jeong YG, Jeong HW. High-resolution magnetic resonance imaging of intracranial vertebral artery dissecting aneurysm for planning of endovascular treatment. J Korean Neurosurg Soc. 2015; 58:155–158.
Article11. O’kelly CJ, Krings T, Fiorella D, Marotta TR. A novel grading scale for the angiographic assessment of intracranial aneurysms treated using flow diverting stents. Interv Neuroradiol. 2010; 16:133–137.
Article12. Kai Y, Nishi T, Watanabe M, Morioka M, Hirano T, Yano S, et al. Strategy for treating unruptured vertebral artery dissecting aneurysms. Neurosurgery. 2011; 69:1085–1091; discussion 1091-1092.
Article13. Kobayashi N, Murayama Y, Yuki I, Ishibashi T, Ebara M, Arakawa H, et al. Natural course of dissecting vertebrobasilar artery aneurysms without stroke. AJNR Am J Neuroradiol. 2014; 35:1371–1375.
Article14. Kassis SZ, Jouanneau E, Tahon FB, Salkine F, Perrin G, Turjman F. Recovery of third nerve palsy after endovascular treatment of posterior communicating artery aneurysms. World Neurosurg. 2010; 73:11–16; discussion e2.
Article15. Ko JH, Kim YJ. Oculomotor nerve palsy caused by posterior communicating artery aneurysm: evaluation of symptoms after endovascular treatment. Interv Neuroradiol. 2011; 17:415–419.
Article16. Cho DY, Kim BS, Choi JH, Park YK, Shin YS. The fate of unruptured intracranial vertebrobasilar dissecting aneurysm with brain stem compression according to different treatment modalities. AJNR Am J Neuroradiol. 2019; 40:1924–1931.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Dissecting Aneurysm of the Intracranial Vertbral Artery: Case Report
- Two Cases of Intracranial Vertebral Artery Dissecting Aneurysm Improved by Antiplatelets Therapy
- Treatment of Ruptured Dissecting Aneurysm Associated with Fenestration of Vertebral Artery: A Case Report
- Dissecting Aneurysm of Intracranial Vertebral Artery: A Case Report
- Spontaneous Resolution of Dissecting Aneurysm of the Vertebral Artery