Ann Rehabil Med.
2021 Jun;45(3):178-185. 10.5535/arm.20241.
Should We Delay Urodynamic Study When Patients With Spinal Cord Injury Have Asymptomatic Pyuria?
- Affiliations
-
- 1Department of Physical Medicine and Rehabilitation, National Rehabilitation Center, Seoul, Korea
- 2Department of Nursing, National Rehabilitation Center, Seoul, Korea
- KMID: 2517595
- DOI: http://doi.org/10.5535/arm.20241
Abstract
Objective
To assess the incidence of urinary tract infection (UTI) with post-urodynamic study (post-UDS) in patients with spinal cord injury (SCI) and study its relationship with pre-UDS pyuria.
Methods
Patients with SCI who were hospitalized and underwent UDS during a 4-year period were reviewed. Patients with pre-test lower urinary tract symptoms were excluded. Urinalysis and urine culture were performed before and 24 hours after UDS. Prophylactic antibiotics were administered for 5 days starting from the morning of the UDS. UTI was defined as bacteriuria with accompanying symptoms.
Results
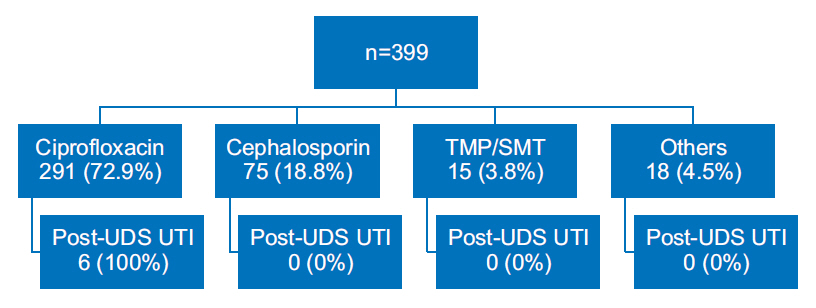
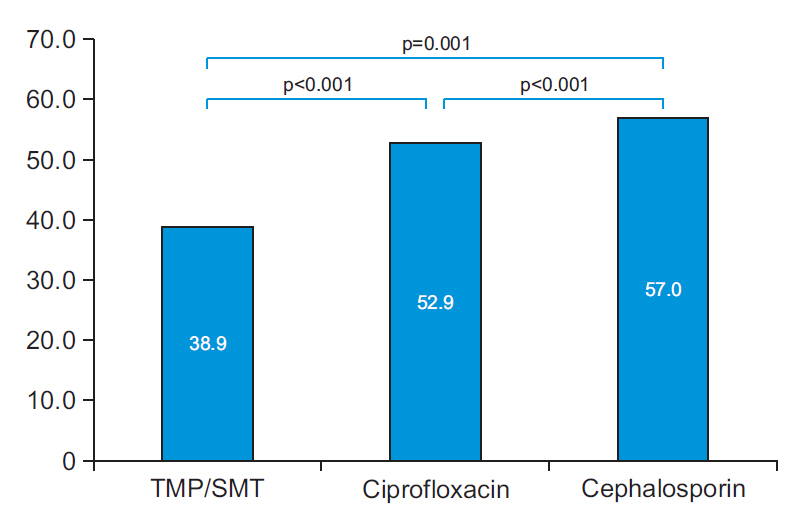
Of 399 patients reviewed, 209 (52.4%) had pyuria in pre-UDS urinalysis, and 257 (64.4%) had bacteriuria in pre-UDS culture. Post-UDS UTI occurred in 6 (1.5%) individuals who all complained of fever: 5 (2.4%) of the post-UDS UTI cases occurred in patients with pre-UDS pyuria, and 1 (0.5%) in a person without. The differences between groups were not statistically significant (p=0.218). Of 221 patients with bacteriuria (gram-negative isolates) on pre-UDS culture, resistance to ciprofloxacin, cephalosporin, and trimethoprim/sulfamethoxazole (TMP/SMT) was noted in 52.9% (117 cases), 57.0% (126 cases), and 38.9% (86 cases), respectively.
Conclusion
No difference was found in the prevalence of post-UDS UTI based on the presence of pyuria in pre-UDS urinalysis. UDS may be performed even in SCI cases of pre-UDS pyuria without increasing the prevalence of post-UDS UTI if prophylactic antibiotics are administered. TMP/SMT could be used as a first-line antibiotic for the prevention of post-UDS UTI in Korea.
Keyword
Figure
Reference
-
1. Albayrak I, Caliskan A Levendoglu F, Ozerbil OM, Dagi HT. Characteristics of urinary tract infections in patients with spinal cord injuries hospitalized at a rehabilitation centre. Cyprus J Med Sci. 2016; 1:17–21.
Article2. Whiteneck GG, Charlifue SW, Frankel HL, Fraser MH, Gardner BP, Gerhart KA, et al. Mortality, morbidity, and psychosocial outcomes of persons spinal cord injured more than 20 years ago. Paraplegia. 1992; 30:617–30.
Article3. Edokpolo LU, Stavris KB, Foster HE Jr. Intermittent catheterization and recurrent urinary tract infection in spinal cord injury. Top Spinal Cord Inj Rehabil. 2012; 18:187–92.
Article4. Khanna R, Sandhu AS, Doddamani D. Urodynamic management of neurogenic bladder in spinal cord injury. Med J Armed Forces India. 2009; 65:300–4.
Article5. Tsai SW, Kung FT, Chuang FC, Ou YC, Wu CJ, Huang KH. Evaluation of the relationship between urodynamic examination and urinary tract infection based on urinalysis results. Taiwan J Obstet Gynecol. 2013; 52:493–7.
Article6. Bothig R, Fiebag K, Thietje R, Faschingbauer M, Hirschfeld S. Morbidity of urinary tract infection after urodynamic examination of hospitalized SCI patients: the impact of bladder management. Spinal Cord. 2013; 51:70–3.
Article7. Yang SO. Catheter-associated urinary tract infection. Korean J Urogenit Tract Infect Inflamm. 2013; 8:73–82.
Article8. Jameson JL, Fauci AS, Kasper DL, Hauser SL, Longo DL, Loscalzo L. Harrison’s principles of internal medicine. 20th ed. New York, NY: McGraw-Hill;2018.9. Rahimkhani M, Nikfallah A, Saberian M, Mordadi A, Varmazyar S, Tavakoli A. Urinary tract infection in spinal cord injuries. Asian J Phama Clin Res. 2014; 7:178–82.10. Tambyah PA, Maki DG. The relationship between pyuria and infection in patients with indwelling urinary catheters: a prospective study of 761 patients. Arch Intern Med. 2000; 160:673–7.
Article11. Goetz LL, Cardenas DD, Kennelly M, Bonne Lee BS, Linsenmeyer T, Moser C, et al. International spinal cord injury urinary tract infection basic data set. Spinal Cord. 2013; 51:700–4.
Article12. Oh SW, Jung JH, Cho IK, Lee HJ, Kwon SH, Lee BS. Changes in the trend in bladder emptying methods in patients with spinal cord injury: a 20-year single-center retrospective study. Ann Rehabil Med. 2020; 44:228–37.
Article13. Amaral DM, Pereira AM, Rodrigues MR, Gandarez MF, Cunha MR, Torres MS. Urinary tract infection in patients with spinal cord injury after urodynamics under fosfomycin prophylaxis: a retrospective analysis. Porto Biomed J. 2019; 4:e56.
Article14. Massa LM, Hoffman JM, Cardenas DD. Validity, accuracy, and predictive value of urinary tract infection signs and symptoms in individuals with spinal cord injury on intermittent catheterization. J Spinal Cord Med. 2009; 32:568–73.
Article15. Pannek J. Treatment of urinary tract infection in persons with spinal cord injury: guidelines, evidence, and clinical practice: a questionnaire-based survey and review of the literature. J Spinal Cord Med. 2011; 34:11–5.16. Pannek J, Nehiba M. Morbidity of urodynamic testing in patients with spinal cord injury: is antibiotic prophylaxis necessary? Spinal Cord. 2007; 45:771–4.
Article17. Hwang SI, Lee BS, Han ZA, Lee HJ, Han SH, Kim MO. Factors related to the occurrence of urinary tract infection following a urodynamic study in patients with spinal cord injury. Ann Rehabil Med. 2016; 40:718–24.
Article18. Cameron AP, Campeau L, Brucker BM, Clemens JQ, Bales GT, Albo ME, et al. Best practice policy statement on urodynamic antibiotic prophylaxis in the non-index patient. Neurourol Urodyn. 2017; 36:915–26.
Article19. Litza JA, Brill JR. Urinary tract infections. Prim Care. 2010; 37:491–507.
Article20. Wagenlehner FM, Wagenlehner C, Schinzel S, Naber KG; Working Group “Urological Infections” of German Society of Urology. Prospective, randomized, multicentric, open, comparative study on the efficacy of a prophylactic single dose of 500 mg levofloxacin versus 1920 mg trimethoprim/sulfamethoxazole versus a control group in patients undergoing TUR of the prostate. Eur Urol. 2005; 47:549–56.21. Hirakauva EY, Bianchi-Ferraro AM, Zucchi EV, Kajikawa MM, Girao MJ, Sartori MG, et al. Incidence of Bacteriuria after Urodynamic Study with or without Antibiotic Prophylaxis in Women with Urinary Incontinence. Rev Bras Ginecol Obstet. 2017; 39:534–40.
Article22. Ditunno JF, Donovan WH, Oleson CV. History of spinal cord medicine. In : Kirshblum S, Lin VW, editors. Spinal cord medicine. 3rd ed. New York, NY: Demos Medical;2018. p. 2–10.23. da Silva MT, Barboza AL, Pijoan MM, Beraldo PS. Antibiotic prophylaxis prior to urodynamic study in patients with traumatic spinal cord injury: is there an indication? Int Braz J Urol. 2019; 45:347–53.24. Kang MS, Lee BS, Lee HJ, Hwang SW, Han ZA. Prevalence of and risk factors for multidrug-resistant bacteria in urine cultures of spinal cord injury patients. Ann Rehabil Med. 2015; 39:686–95.
Article25. Fitzpatrick MA, Suda KJ, Safdar N, Burns SP, Jones MM, Poggensee L, et al. Changes in bacterial epidemiology and antibiotic resistance among veterans with spinal cord injury/disorder over the past 9 years. J Spinal Cord Med. 2018; 41:199–207.
Article26. Suda KJ, Patel UC, Sabzwari R, Cao L, Ramanathan S, Hill JN, et al. Bacterial susceptibility patterns in patients with spinal cord injury and disorder (SCI/D): an opportunity for customized stewardship tools. Spinal Cord. 2016; 54:1001–9.
Article27. Yoon SB, Lee BS, Lee KD, Hwang SI, Lee HJ, Han ZA. Comparison of bacterial strains and antibiotic susceptibilities in urinary isolates of spinal cord injury patients from the community and hospital. Spinal Cord. 2014; 52:298–301.
Article28. Ramanathan S, Fitzpatrick MA, Suda KJ, Burns SP, Jones MM, LaVela et al. Multidrug-resistant gramnegative organisms and association with 1-year mortality, readmission, and length of stay in Veterans with spinal cord injuries and disorders. Spinal Cord. 2020; 58:596–608.
Article29. Kim HY, Lee SJ, Lee DS, Yoo JM, Choe HS. Microbiological characteristics of unresolved acute uncomplicated cystitis. Microb Drug Resist. 2016; 22:387–91.
Article30. Kitagawa K, Shigemura K, Nomi M, Takami N, Yamada N, Fujisawa M. Use of oral third generation cephalosporins and quinolones and occurrence of antibiotic-resistant strains in the neurogenic bladder (NB) outpatient setting: a retrospective chart audit. Spinal Cord. 2020; 58:705–10.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ice Water Urodynamic Study in Neurogenic Bladder of Spinal Cord Injured Patients
- A Correlation of Bulbocavernosus Reflex Test and Urodynamic Investigation in the Spinal Cord Injury Patients
- Risk Factors of Bladder Stone Formation in Spinal Cord Injuries
- Clinical Characteristics of Acute Pyelonephritis in Spinal Cord Injury Patient
- Delay of Orocecal Transit Time in Patients with Chronic Spinal Cord Injury