J Cerebrovasc Endovasc Neurosurg.
2021 Jun;23(2):145-151. 10.7461/jcen.2021.E2020.11.005.
Proximal basilar artery hemorrhage after submaximal angioplasty for intracranial atherosclerotic disease presenting as a large vessel occlusion treated with pipeline embolization device
- Affiliations
-
- 1Department of Neurosurgery, Carle BroMenn Medical Center, Normal, IL, USA
- 2Department of Neurosurgery, Advocate Christ Medical Center, Oak Lawn, IL, USA
- KMID: 2517028
- DOI: http://doi.org/10.7461/jcen.2021.E2020.11.005
Abstract
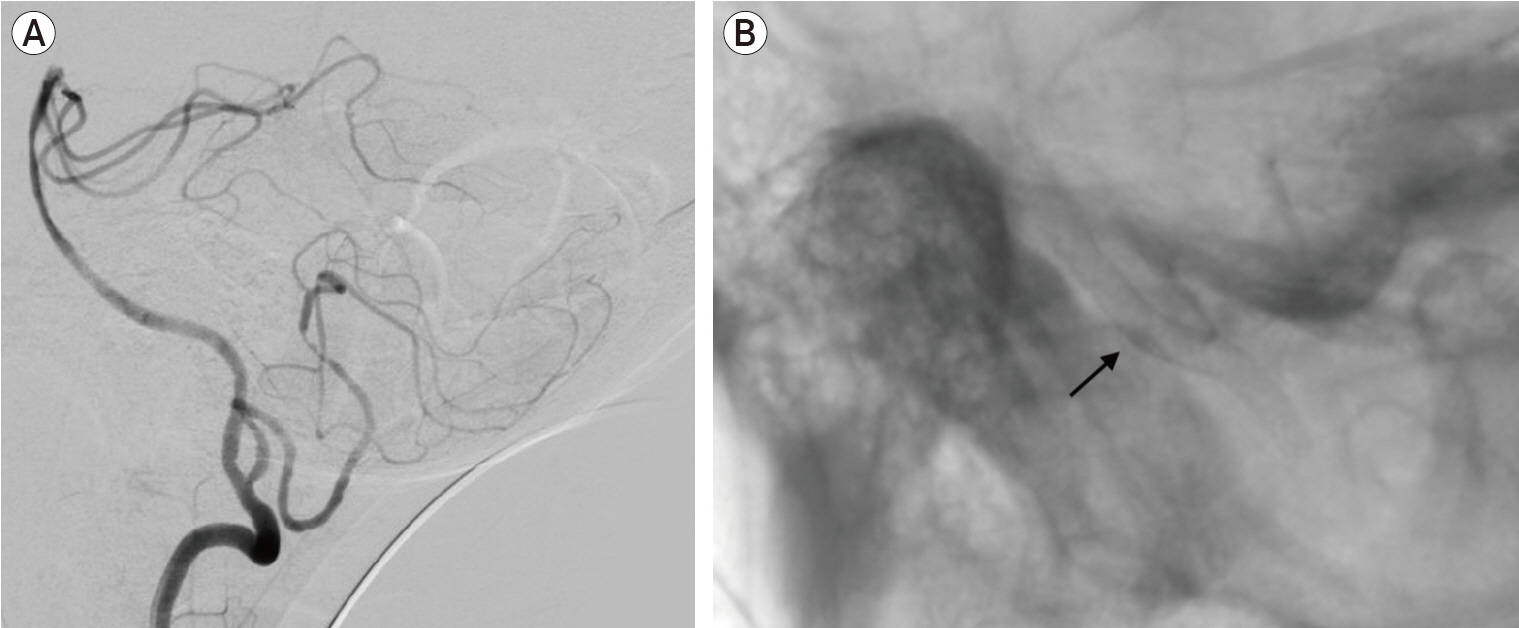
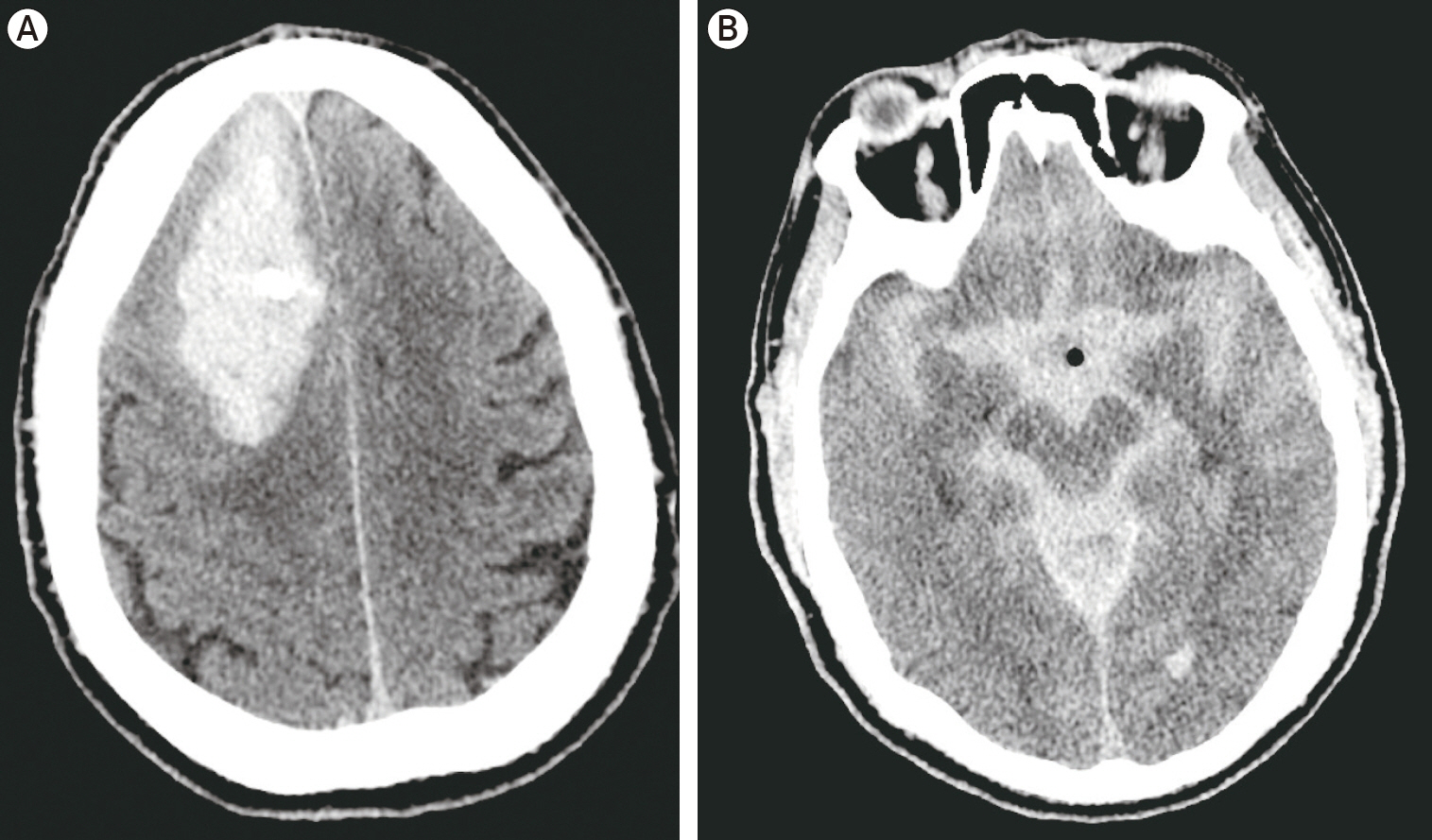
- Iatrogenic vessel perforation from endovascular intervention is a devastating complication that commonly is treated with vessel sacrifice. We present a unique case of an iatrogenic proximal basilar artery perforation after submaximal angioplasty in a 67-year-old male presenting with an acute basilar artery occlusion with underlying intracranial atherosclerotic disease. Telescoping flow-diverting stents were then deployed to reconstruct the vessel wall with resulting active hemorrhage resolution. Our case documents a successful deployment of flow-diverting stents with resolution of active hemorrhage after an iatrogenic basilar artery perforation.
Figure
Reference
-
1. Alexander MD, Rebhun JM, Hetts SW, Amans MR, Settecase F, Darflinger RJ, et al. Technical factors affecting outcomes following endovascular treatment of posterior circulation atherosclerotic lesions. Surg Neurol Int. 2017; Nov. 8:284.
Article2. Ambekar S, Sharma M, Smith D, Cuellar H. Successful treatment of iatrogenic vertebral pseudoaneurysm using pipeline embolization device. Case Rep Vasc Med. 2014; 2014:341748.
Article3. Amenta PS, Starke RM, Jabbour PM, Tjoumakaris SI, Gonzalez LF, Rosenwasser RH, et al. Successful treatment of a traumatic carotid pseudoaneurysm with the Pipeline stent: Case report and review of the literature. Surg Neurol Int. 2012; 3:160.
Article4. Baek JH, Kim BM, Heo JH, Kim DJ, Nam HS, Kim YD. Endovascular and clinical outcomes of vertebrobasilar intracranial atherosclerosis-related large vessel occlusion. Front Neurol. 2019; Mar. 10:215.
Article5. Chimowitz MI, Lynn MJ, Derdeyn CP, Turan TN, Fiorella D, Lane BF, et al. Stenting versus aggressive medical therapy for intracranial arterial stenosis. N Engl J Med. 2011; Sep. 365(11):993–1003.6. Dolati P, Eichberg DG, Thomas A, Ogilvy CS. Application of pipeline embolization device for iatrogenic pseudoaneurysms of the extracranial vertebral artery: A case report and systematic review of the literature. Cureus. 2015; Oct. 7(10):e356.
Article7. Dumont TM, Sonig A, Mokin M, Eller JL, Sorkin GC, Snyder KV, et al. Submaximal angioplasty for symptomatic intracranial atherosclerosis: a prospective Phase I study. J Neurosurg. 2016; Oct. 125(4):964–71.
Article8. Griauzde J, Gemmete JJ, Pandey AS, McKean EL, Sullivan SE, Chaudhary N. Emergency reconstructive endovascular management of intraoperative complications involving the internal carotid artery from trans-sphenoidal surgery. J Neurointerv Surg. 2015; Jan. 7(1):67–71.
Article9. Griauzde J, Ravindra VM, Chaudhary N, Gemmete JJ, Mazur MD, Roark CD, et al. Use of the Pipeline embolization device in the treatment of iatrogenic intracranial vascular injuries: a bi-institutional experience. Neurosurg Focus. 2017; Jun. 42(6):E9.
Article10. Lee JS, Hong JM, Lee KS, Suh HI, Demchuk AM, Hwang YH, et al. Endovascular therapy of cerebral arterial occlusions: Intracranial atherosclerosis versus embolism. J Stroke Cerebrovasc Dis. 2015; Sep. 24(9):2074–80.
Article11. Lee YY, Yoon W, Kim SK, Baek BH, Kim GS, Kim JT, et al. Acute basilar artery occlusion: Differences in characteristics and outcomes after endovascular therapy between patients with and without underlying severe atherosclerotic stenosis. AJNR Am J Neuroradiol. 2017; Aug. 38(8):1600–4.
Article12. Seyedsaadat SM, Yolcu YU, Neuhaus A, Rizvi A, Alzuabi M, Murad MH, et al. Submaximal angioplasty in the treatment of patients with symptomatic ICAD: a systematic review and meta-analysis. J Neurointerv Surg. 2020; Apr. 12(4):380–5.
Article13. Zaidat OO, Fitzsimmons BF, Woodward BK, Wang Z, Killer-Oberpfalzer M, Wakhloo A, et al. Effect of a balloon-expandable intracranial stent vs medical therapy on risk of stroke in patients with symptomatic intracranial stenosis: the VISSIT randomized clinical trial. JAMA. 2015; Mar. 313(12):1240–8.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Persistent Aneurysm Growth Following Pipeline Embolization Device Assisted Coiling of a Fusiform Vertebral Artery Aneurysm: A Word of Caution!
- Endovascular Therapy for Acute Basilar Artery Occlusion: Comparison between Patients with and without Underlying Intracranial Atherosclerotic Stenosis
- Rupture Basilar Artery Dissection: Successful Treatment with Neuroform Stent Placement and Coil Embolization
- Coil Embolization of a Ruptured Basilar Tip Aneurysm Associated with Bilateral Cervical Internal Carotid Artery Occlusion: A Case Report and Literature Review
- The Use of a Pipeline Embolization Device for Treatment of a Ruptured Dissecting Middle Cerebral Artery M3/M4 Aneurysm: Challenges and Technical Considerations