Changes in the Occurrence of Gastrointestinal Infections after COVID-19 in Korea
- Affiliations
-
- 1Department of Pediatrics, Chung-Ang University Hospital, Seoul, Korea
- 2College of Medicine, Chung-Ang University, Seoul, Korea
- 3Department of Preventive Medicine, College of Medicine, Chung-Ang University, Seoul, Korea
- KMID: 2516769
- DOI: http://doi.org/10.3346/jkms.2021.36.e180
Abstract
- Background
After the global epidemic of coronavirus disease 2019 (COVID-19), lifestyle changes to curb the spread of COVID-19 (e.g., wearing a mask, hand washing, and social distancing) have also affected the outbreak of other infectious diseases. However, few studies have been conducted on whether the incidence of gastrointestinal infections has changed over the past year with COVID-19. In this study, we examined how the incidence of gastrointestinal infections has changed since COVID-19 outbreak through open data.
Methods
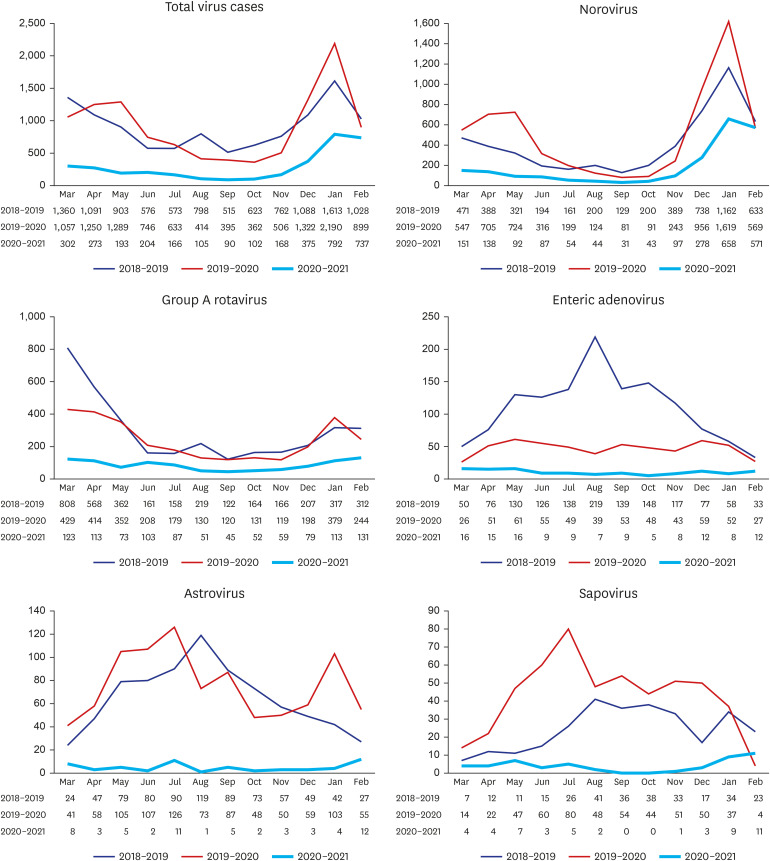
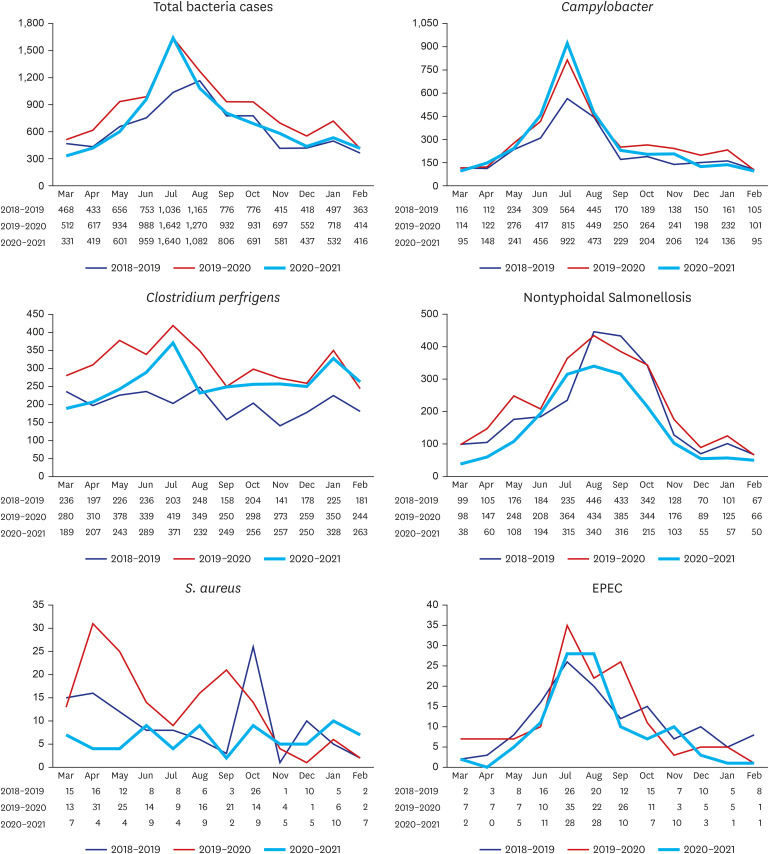
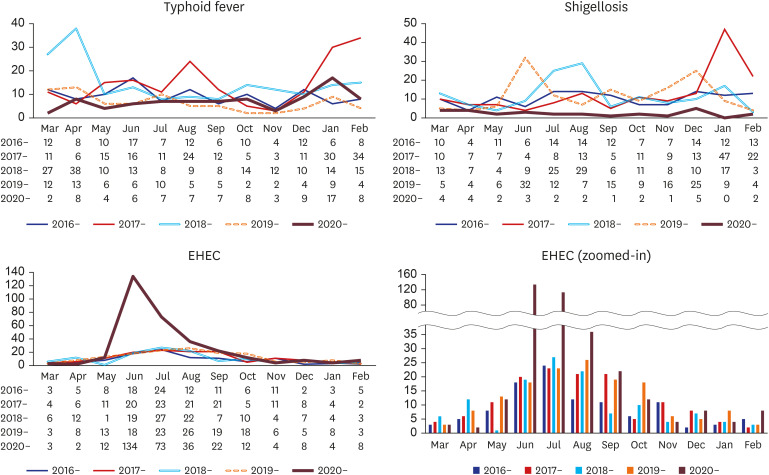
We summarized the data on the several viruses and bacteria that cause gastrointestinal infections from the open data of the Korea Disease Control and Prevention Agency for 3 years from March 2018 to February 2021 (from Spring 2018 to Winter 2020). Moreover, we confirmed three most common legal gastrointestinal infectious pathogens from March 2016.
Results
From March 2020, when the COVID-19 epidemic was in full swing and social distancing and personal hygiene management were heavily emphasized, the incidence of infection from each virus was drastically decreased. The reduction rates compared to the averages of the last 2 years were as follows: total viruses 31.9%, norovirus 40.2%, group A rotavirus 31.8%, enteric adenovirus 13.4%, astrovirus 7.0%, and sapovirus 12.2%. Among bacterial pathogens, the infection rates of Campylobacter and Clostridium perfringens did not decrease but rather increased in some periods when compared to the average of the last two years. The incidence of nontyphoidal Salmonella, Staphylococcus aureus, or enteropathogenic Escherichia coli somewhat decreased but not significantly compared to the previous two years.
Conclusion
The incidence of infection from gastrointestinal viruses, which are mainly caused by the fecal-to-oral route and require direct contact among people, was significantly reduced, whereas the incidence of bacterial pathogens, which have food-mediated transmission as the main cause of infection, did not decrease significantly.
Keyword
Figure
Cited by 4 articles
-
Changes in the Incidence of Intussusception and Infectious Diseases After the COVID-19 Pandemic in Korea
In Hyuk Yoo, Hyun Mi Kang, Dae Chul Jeong
J Korean Med Sci. 2022;37(8):e60. doi: 10.3346/jkms.2022.37.e60.Impact of COVID-19 on Clinicopathological Spectrum of Pityriasis Rosea in Korea
Dai Hyun Kim, Jun Hyuk Cho, Sung Jin Park, Soo Hong Seo, Hyo Hyun Ahn
J Korean Med Sci. 2022;37(24):e190. doi: 10.3346/jkms.2022.37.e190.Epidemiological Trends of Pediatric Inflammatory Bowel Disease in Korea: A Multicenter Study of the Last 3 Years Including the COVID-19 Era
So Yoon Choi, Sujin Choi, Ben Kang, Byung-Ho Choe, Yeoun Joo Lee, Jae Hong Park, Yu Bin Kim, Jae Young Kim, Kunsong Lee, Kyung Jae Lee, Ki Soo Kang, Yoo Min Lee, Hyun Jin Kim, Yunkoo Kang, Hyo-Jeong Jang, Dae Yong Yi, Suk Jin Hong, You Jin Choi, Jeana Hong, Soon Chul Kim
J Korean Med Sci. 2022;37(37):e279. doi: 10.3346/jkms.2022.37.e279.An Outbreak of Campylobacter Jejuni Involving Healthcare Workers Detected by COVID-19 Healthcare Worker Symptom Surveillance
Hye Jin Shi, Jae Baek Lee, Shinhee Hong, Joong Sik Eom, Yoonseon Park
Korean J Healthc Assoc Infect Control Prev. 2023;28(1):172-177. doi: 10.14192/kjicp.2023.28.1.172.
Reference
-
1. Choi JY. COVID-19 in South Korea. Postgrad Med J. 2020; 96(1137):399–402. PMID: 32366457.
Article2. Ha KM. The principle of distance during COVID-19 outbreak in Korea. Int Microbiol. 2020; 23(4):641–643. PMID: 32719983.
Article3. Lu N, Cheng KW, Qamar N, Huang KC, Johnson JA. Weathering COVID-19 storm: Successful control measures of five Asian countries. Am J Infect Control. 2020; 48(7):851–852. PMID: 32360746.
Article4. Wee LE, Conceicao EP, Sim XY, Ko KK, Ling ML, Venkatachalam I. Reduction in healthcare-associated respiratory viral infections during a COVID-19 outbreak. Clin Microbiol Infect. 2020; 26(11):1579–1581. PMID: 32622953.
Article5. Itaya T, Furuse Y, Jindai K. Does COVID-19 infection impact on the trend of seasonal influenza infection? 11 countries and regions, from 2014 to 2020. Int J Infect Dis. 2020; 97:78–80. PMID: 32492532.
Article6. Choi DH, Jung JY, Suh D, Choi JY, Lee SU, Choi YJ, et al. Impact of the COVID-19 outbreak on trends in emergency department utilization in children: a multicenter retrospective observational study in Seoul metropolitan area, Korea. J Korean Med Sci. 2021; 36(5):e44. PMID: 33527786.
Article7. Kim JS, Lee MS, Kim JH. Recent updates on outbreaks of Shiga toxin-producing Escherichia coli and its potential reservoirs. Front Cell Infect Microbiol. 2020; 10:273. PMID: 32582571.
Article8. Bryce J, Boschi-Pinto C, Shibuya K, Black RE. WHO Child Health Epidemiology Reference Group. WHO estimates of the causes of death in children. Lancet. 2005; 365(9465):1147–1152. PMID: 15794969.
Article9. Korea Disease Control and Prevention Agency. Infectious disease portal. Updated 2021. http://www.kdca.go.kr/npt/biz/npp/portal/nppPblctDtaMain.do.10. Ryoo E. Causes of acute gastroenteritis in Korean children between 2004 and 2019. Clin Exp Pediatr. 2021; 64(6):260–268. PMID: 32972055.
Article11. Karg MV, Alber B, Kuhn C, Bohlinger K, Englbrecht M, Dormann H. SARS-CoV-2, influenza and norovirus infection: a direct epidemiologic comparison. Med Klin Intensivmed Notf Med.12. Laszkowska M, Kim J, Faye AS, Joelson AM, Ingram M, Truong H, et al. Prevalence of Clostridioides difficile and other gastrointestinal pathogens in patients with COVID-19. Dig Dis Sci.
Article13. Matsuyama R, Miura F, Nishiura H. The transmissibility of noroviruses: Statistical modeling of outbreak events with known route of transmission in Japan. PLoS One. 2017; 12(3):e0173996. PMID: 28296972.
Article14. Matsuyama R, Miura F, Tsuzuki S, Nishiura H. Household transmission of acute gastroenteritis during the winter season in Japan. J Int Med Res. 2018; 46(7):2866–2874. PMID: 29865912.
Article15. Wen SC, Best E, Nourse C. Non-typhoidal Salmonella infections in children: review of literature and recommendations for management. J Paediatr Child Health. 2017; 53(10):936–941. PMID: 28556448.
Article16. Majowicz SE, Musto J, Scallan E, Angulo FJ, Kirk M, O'Brien SJ, et al. The global burden of nontyphoidal Salmonella gastroenteritis. Clin Infect Dis. 2010; 50(6):882–889. PMID: 20158401.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Trends in gastrointestinal infections before and during non-pharmaceutical interventions in Korea in comparison with the United States
- COVID-19 among infants: key clinical features and remaining controversies
- Gastrointestinal Symptoms in Patients with COVID-19 and Usefulness of Stool Test
- COVID-19 and Fungal Infection
- The Role of COVID-19 Vaccination for Patients With Atherosclerotic Cardiovascular Disease in the Upcoming Endemic Era