J Korean Foot Ankle Soc.
2021 Jun;25(2):89-94. 10.14193/jkfas.2021.25.2.89.
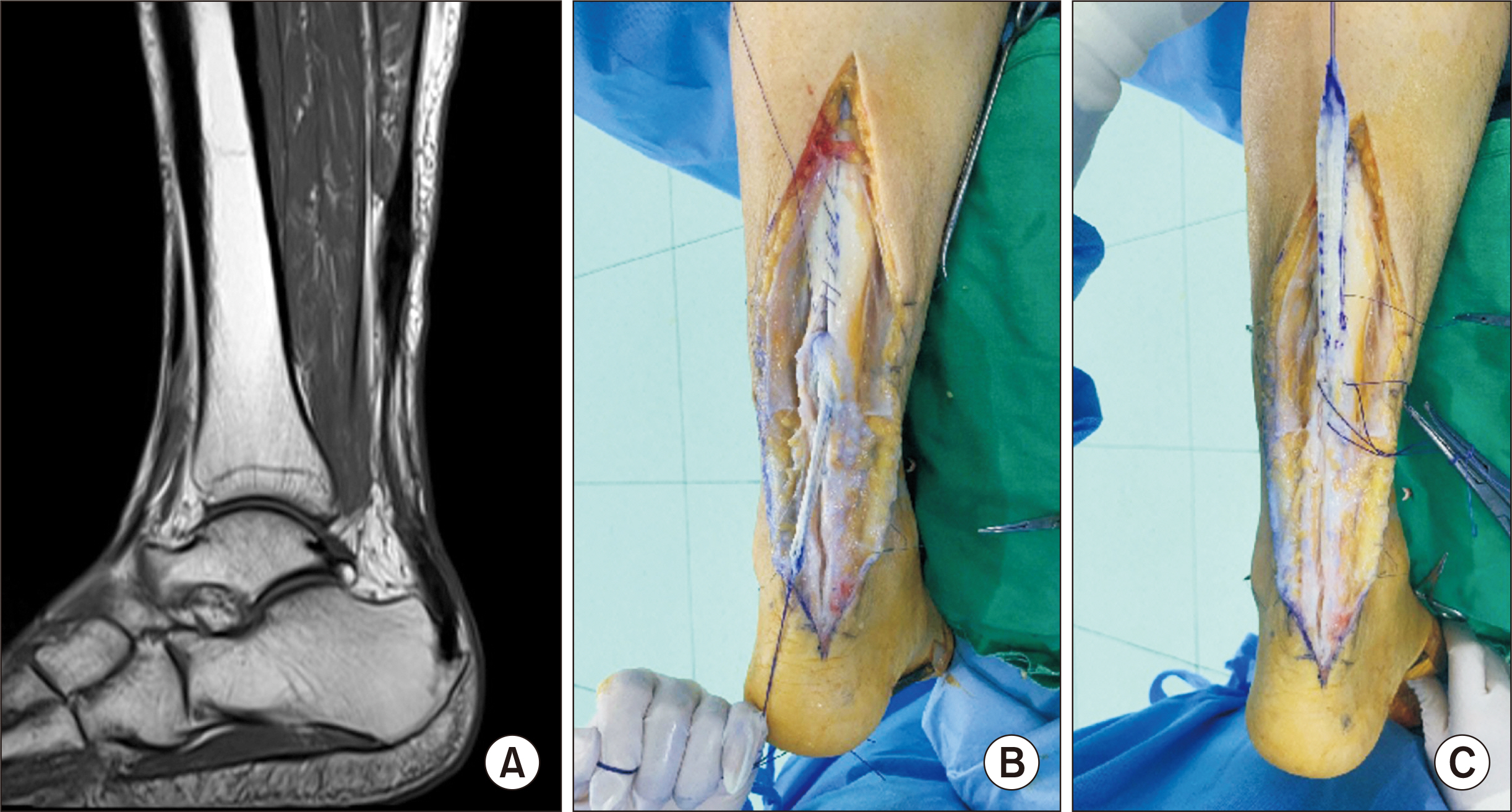
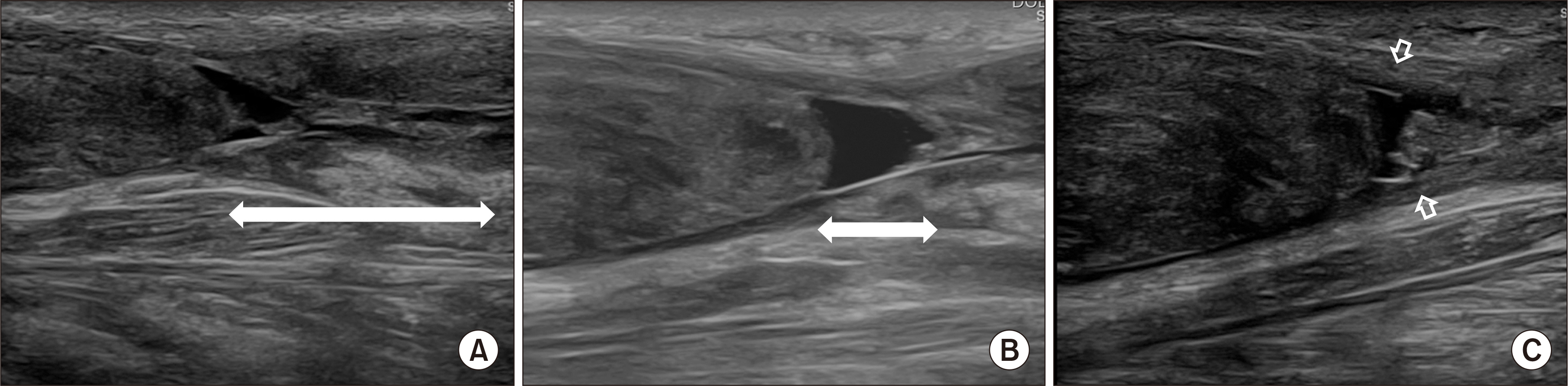
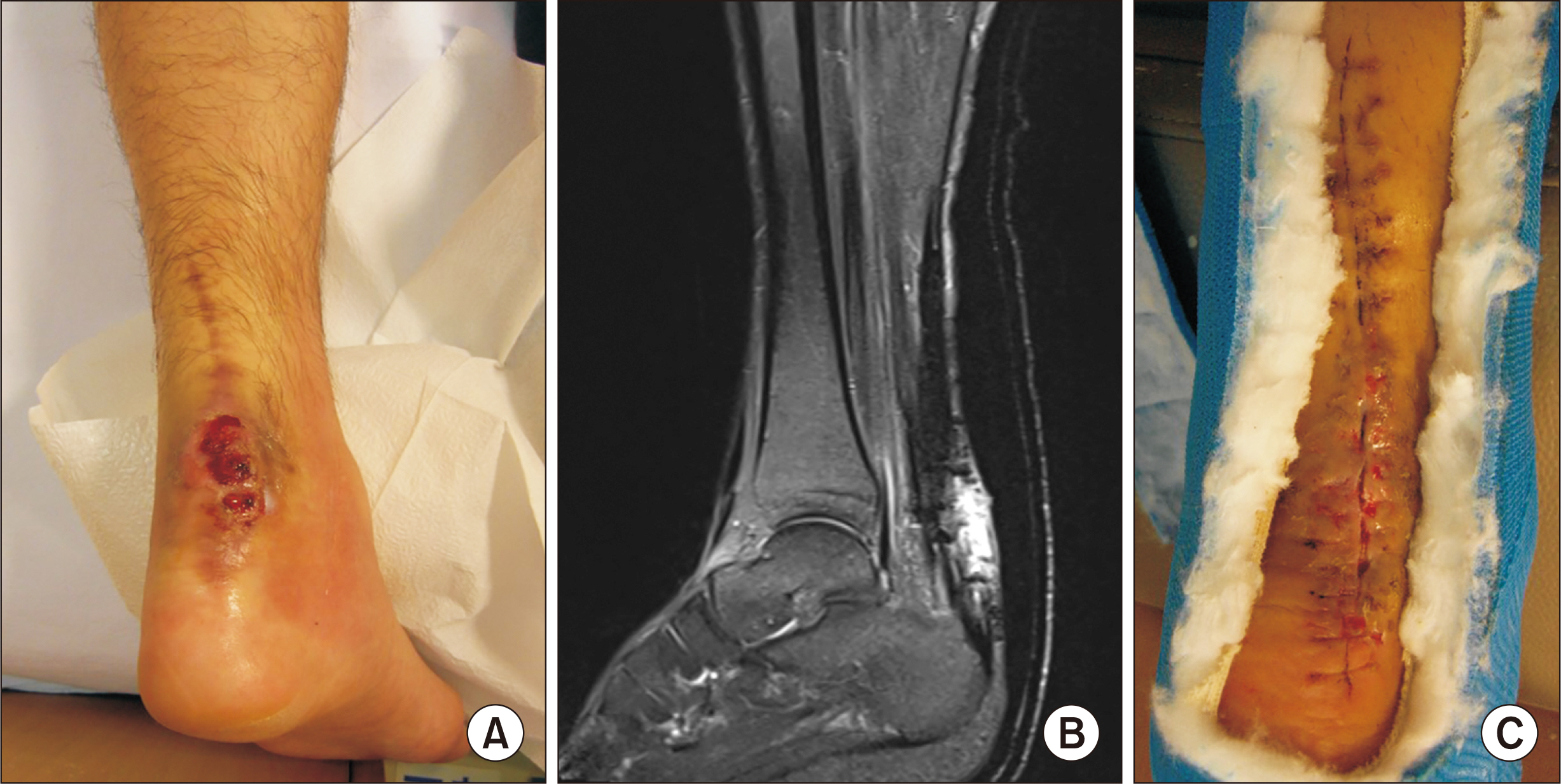
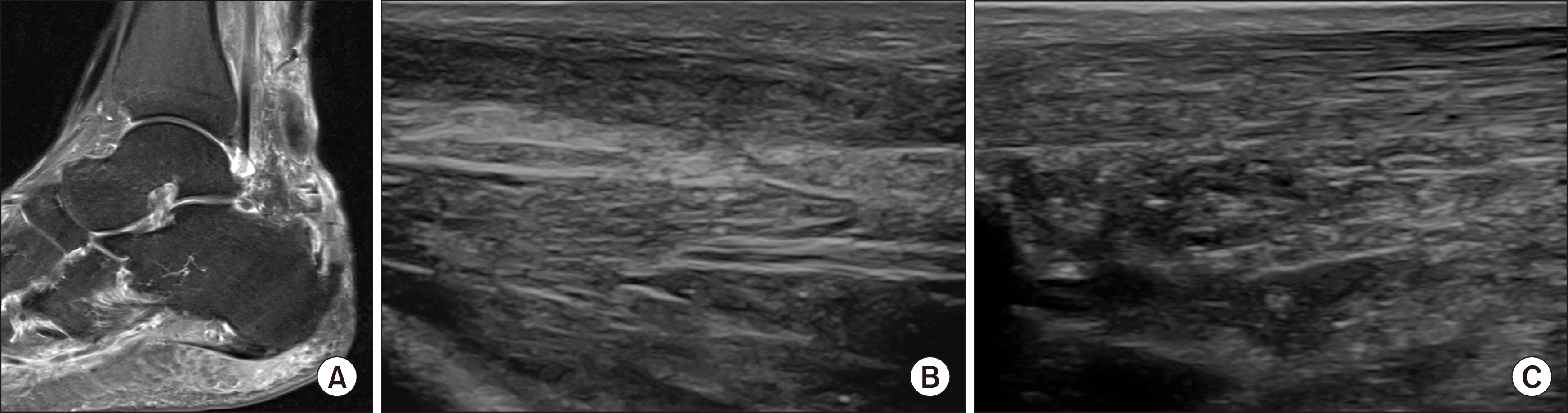
Management of Postoperative Complications Following Surgical Repair of Achilles Tendon Rupture
- Affiliations
-
- 1Department of Orthopedic Surgery, Sanggye Paik Hospital, Inje University College of Medicine, Seoul, Korea
- KMID: 2516646
- DOI: http://doi.org/10.14193/jkfas.2021.25.2.89
Abstract
- The surgical repair of an Achilles tendon acute rupture is a proven, traditional treatment for optimal functional recovery. However, concerns regarding complications such as re-rupture, wound problems and infections are driving new techniques, including minimally invasive approaches and nonoperative treatments. If we understand the characteristics and contemplate treatment strategies for possible complications, the surgical repair of the Achilles tendon is an attractive option and can be expected to yield satisfactory functional recovery.
Keyword
Figure
Reference
-
1. Rensing N, Waterman BR, Frank RM, Heida KA, Orr JD. 2017; Low risk for local and systemic complications after primary repair of 1626 Achilles tendon ruptures. Foot Ankle Spec. 10:216–26. doi: 10.1177/1938640016676340. DOI: 10.1177/1938640016676340. PMID: 27837039.
Article2. Jildeh TR, Okoroha KR, Marshall NE, Abdul-Hak A, Zeni F, Moutzouros V. 2018; Infection and rerupture after surgical repair of Achilles tendons. Orthop J Sports Med. 6:2325967118774300. doi: 10.1177/2325967118774302. DOI: 10.1177/2325967118774302. PMID: 29854862. PMCID: PMC5971389.
Article3. Bruggeman NB, Turner NS, Dahm DL, Voll AE, Hoskin TL, Jacofsky DJ, et al. 2004; Wound complications after open Achilles tendon repair: an analysis of risk factors. Clin Orthop Relat Res. (427):63–6. doi: 10.1097/01.blo.0000144475.05543.e7. DOI: 10.1097/01.blo.0000144475.05543.e7. PMID: 15552138.4. Hussien DG, Villarreal JV, Panchbhavi V, Jupiter DC. 2021; Predisposing factors for 30-day complications following Achilles tendon repair. J Foot Ankle Surg. 60:288–91. doi: 10.1053/j.jfas.2020.08.029. DOI: 10.1053/j.jfas.2020.08.029. PMID: 33461920.
Article5. Wu Y, Mu Y, Yin L, Wang Z, Liu W, Wan H. 2019; Complications in the management of acute Achilles tendon rupture: a systematic review and network meta-analysis of 2060 patients. Am J Sports Med. 47:2251–60. doi: 10.1177/0363546518824601. DOI: 10.1177/0363546518824601. PMID: 30781966.
Article6. Yang B, Liu Y, Kan S, Zhang D, Xu H, Liu F, et al. 2017; Outcomes and complications of percutaneous versus open repair of acute Achilles tendon rupture: a meta-analysis. Int J Surg. 40:178–86. doi: 10.1016/j.ijsu.2017.03.021. DOI: 10.1016/j.ijsu.2017.03.021. PMID: 28288878.
Article7. Stavenuiter XJR, Lubberts B, Prince RM 3rd, Johnson AH, DiGiovanni CW, Guss D. 2019; Postoperative complications following repair of acute Achilles tendon rupture. Foot Ankle Int. 40:679–86. doi: 10.1177/1071100719831371. DOI: 10.1177/1071100719831371. PMID: 30808187.
Article8. Pean CA, Christiano A, Rubenstein WJ, Konda SR, Egol KA. 2018; Risk factors for complications after primary repair of Achilles tendon ruptures. J Orthop. 15:226–9. doi: 10.1016/j.jor.2018.01.017. DOI: 10.1016/j.jor.2018.01.017. PMID: 29657473. PMCID: PMC5895883.
Article9. Barber GR, Miransky J, Brown AE, Coit DG, Lewis FM, Thaler HT, et al. 1995; Direct observations of surgical wound infections at a comprehensive cancer center. Arch Surg. 130:1042–7. doi: 10.1001/archsurg.1995.01430100020005. DOI: 10.1001/archsurg.1995.01430100020005. PMID: 7575114.
Article10. Burrus MT, Werner BC, Park JS, Perumal V, Cooper MT. 2016; Achilles tendon repair in obese patients is associated with increased complication rates. Foot Ankle Spec. 9:208–14. doi: 10.1177/1938640015609983. DOI: 10.1177/1938640015609983. PMID: 26459362.
Article11. Liles J, Adams SB Jr. 2019; Management of complications of Achilles tendon surgery. Foot Ankle Clin. 24:447–57. doi: 10.1016/j.fcl.2019.04.008. DOI: 10.1016/j.fcl.2019.04.008. PMID: 31370996.
Article12. Deng S, Sun Z, Zhang C, Chen G, Li J. 2017; Surgical treatment versus conservative management for acute Achilles tendon rupture: a systematic review and meta-analysis of randomized controlled trials. J Foot Ankle Surg. 56:1236–43. doi: 10.1053/j.jfas.2017.05.036. DOI: 10.1053/j.jfas.2017.05.036. PMID: 29079238.13. Metz R, Verleisdonk EJ, van der Heijden GJ, Clevers GJ, Hammacher ER, Verhofstad MH, et al. 2008; Acute Achilles tendon rupture: minimally invasive surgery versus nonoperative treatment with immediate full weightbearing--a randomized controlled trial. Am J Sports Med. 36:1688–94. doi: 10.1177/0363546508319312. DOI: 10.1177/0363546508319312. PMID: 18645042.14. Westin O, Nilsson Helander K, Grävare Silbernagel K, Samuelsson K, Brorsson A, Karlsson J. 2018; Patients with an Achilles tendon re-rupture have long-term functional deficits and worse patient-reported outcome than primary ruptures. Knee Surg Sports Traumatol Arthrosc. 26:3063–72. doi: 10.1007/s00167-018-4952-0. DOI: 10.1007/s00167-018-4952-0. PMID: 29691618. PMCID: PMC6154022.15. van Maele M, Misselyn D, Metsemakers WJ, Sermon A, Nijs S, Hoekstra H. 2018; Is open acute Achilles tendon rupture repair still justified? A single center experience and critical appraisal of the literature. Injury. 49:1947–52. doi: 10.1016/j.injury.2018.08.012. DOI: 10.1016/j.injury.2018.08.012. PMID: 30144965.
Article16. Jones MP, Khan RJ, Carey Smith RL. 2012; Surgical interventions for treating acute Achilles tendon rupture: key findings from a recent Cochrane review. J Bone Joint Surg Am. 94:e88. doi: 10.2106/JBJS.J.01829. DOI: 10.2106/JBJS.J.01829. PMID: 22717840.
Article17. Majewski M, Rohrbach M, Czaja S, Ochsner P. 2006; Avoiding sural nerve injuries during percutaneous Achilles tendon repair. Am J Sports Med. 34:793–8. doi: 10.1177/0363546505283266. DOI: 10.1177/0363546505283266. PMID: 16627630.
Article18. Barfod KW, Sveen TM, Ganestam A, Ebskov LB, Troelsen A. 2017; Severe functional debilitations after complications associated with acute Achilles tendon rupture with 9 years of follow-up. J Foot Ankle Surg. 56:440–4. doi: 10.1053/j.jfas.2017.01.004. DOI: 10.1053/j.jfas.2017.01.004. PMID: 28216305.19. Pajala A, Kangas J, Ohtonen P, Leppilahti J. 2002; Rerupture and deep infection following treatment of total Achilles tendon rupture. J Bone Joint Surg Am. 84:2016–21. doi: 10.2106/00004623-200211000-00017. DOI: 10.2106/00004623-200211000-00017. PMID: 12429764.
Article20. Bae SH, Lee HS, Seo SG, Kim SW, Gwak HC, Bae SY. 2016; Debridement and functional rehabilitation for Achilles tendon infection following tendon repair. J Bone Joint Surg Am. 98:1161–7. doi: 10.2106/JBJS.15.01117. DOI: 10.2106/JBJS.15.01117. PMID: 27440563.
Article21. Molloy A, Wood EV. 2009; Complications of the treatment of Achilles tendon ruptures. Foot Ankle Clin. 14:745–59. doi: 10.1016/j.fcl.2009.07.004. DOI: 10.1016/j.fcl.2009.07.004. PMID: 19857846.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Deep Vein Thrombosis after Achilles Tendon Repair: A Case Report
- Heterotopic Ossification of a Partially Ruptured Achilles Tendon (A Case Report)
- Minimal Invasive Surgery for Acute Achilles Tendon Rupture
- Percutaneous Repair of Acute Achilles Tendon Ruptures
- Free Semitendinosus Tendon Graft in Re-ruptured Achilles Tendon