Ann Hepatobiliary Pancreat Surg.
2021 May;25(2):167-170. 10.14701/ahbps.2021.25.2.167.
Hepatic artery aneurysms: Endovascular therapeutic techniques
- Affiliations
-
- 1Department of Radiological Area, Interventional Radiology Unit, E.O. Galliera Hospital, Genova, Italy
- 2Department of Radiology and Interventional Radiology, IRCCS San Martino Policlinic University Hospital, Genova, Italy
- KMID: 2516236
- DOI: http://doi.org/10.14701/ahbps.2021.25.2.167
Abstract
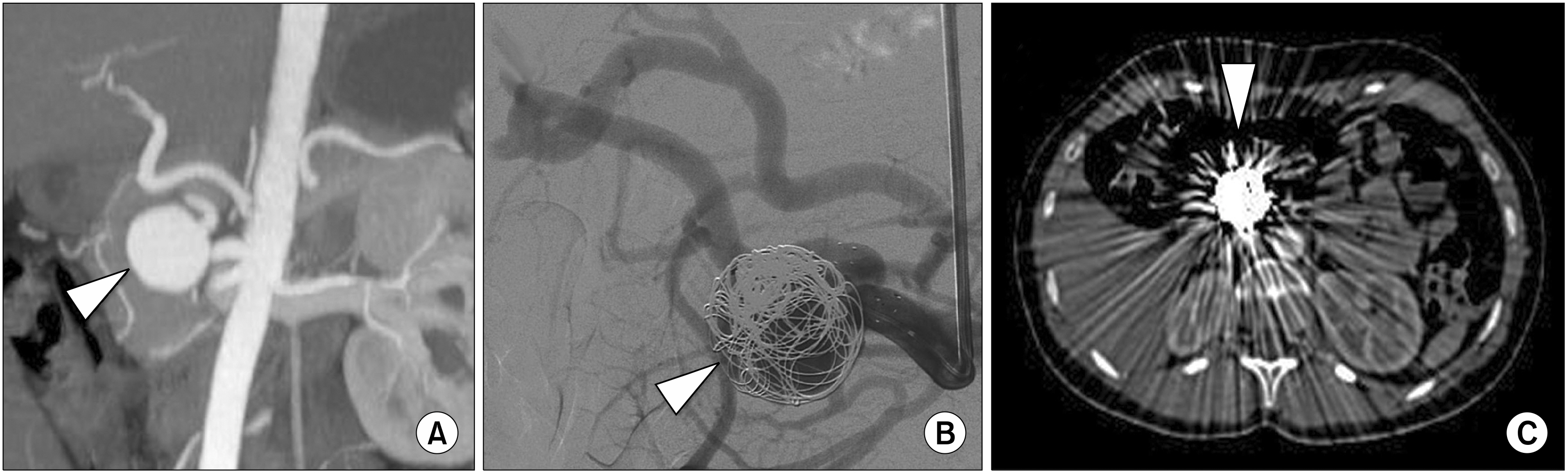
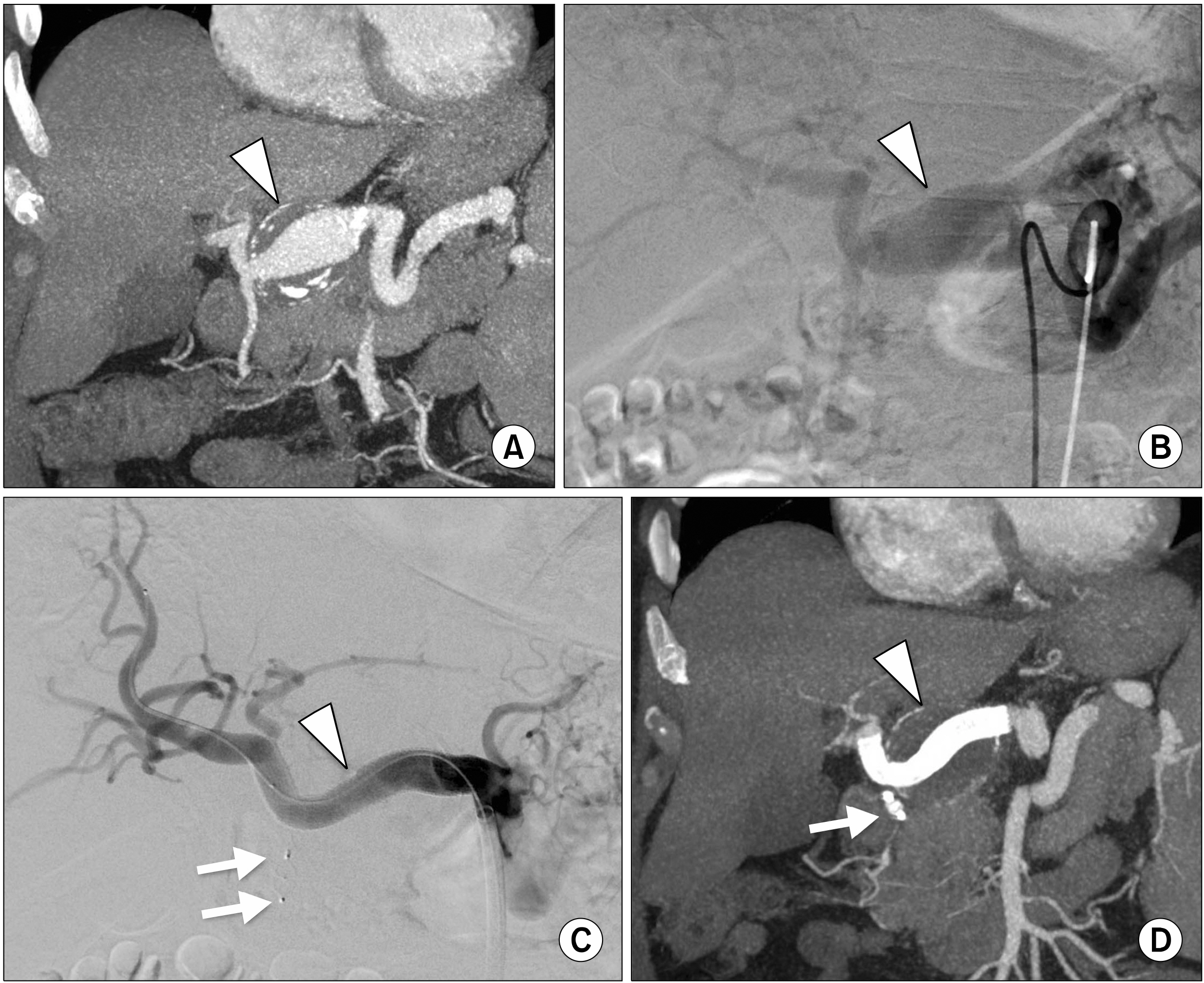
- Hepatic Artery Aneurysm (HAA) is a rare disease, but it can be a life-threatening pathology if it is ruptured. MultiDetector Computed Tomography has to be considered the “gold standard” diagnostic imaging in detecting HAA and it is essential for treatment planning. Treatment for HAA can be surgical or endovascular. Endovascular approaches in HAA, compare to conventional abdominal surgery, benefit in less invasive treatments. The aim of our paper is to emphasize the three possible endovascular therapeutic techniques in HAA: packing embolization, isolation embolization and stenting deployment.
Keyword
Figure
Reference
-
1. Rosenberg A, Trebska-McGowan K, Reichman T, Sharma A, Cotterell A, Strife B, et al. 2020; Management of hepatic artery aneurysm: a case series. Ann Hepatobiliary Pancreat Surg. 24:333–338. DOI: 10.14701/ahbps.2020.24.3.333. PMID: 32843601. PMCID: PMC7452805.
Article2. Obara H, Kentaro M, Inoue M, Kitagawa Y. 2020; Current management strategies for visceral artery aneurysms: an overview. Surg Today. 50:38–49. DOI: 10.1007/s00595-019-01898-3. PMID: 31620866. PMCID: PMC6949316.
Article3. Chiaradia M, Novelli L, Deux JF, Tacher V, Mayer J, You K, et al. 2015; Ruptured visceral artery aneurysms. Diagn Interv Imaging. 96:797–806. DOI: 10.1016/j.diii.2015.03.012. PMID: 26054246.
Article4. Ferro C, Rossi UG, Bovio G, Petrocelli F, Seitun S. 2010; The Amplatzer vascular plug 4: preliminary experience. Cardiovasc Intervent Radiol. 33:844–848. DOI: 10.1007/s00270-009-9749-6. PMID: 19908084.
Article5. Ferro C, Rossi UG, Seitun S, Bovio G, Castellan L, De Paolis M, et al. 2008; Hepatic arterial loop with accessory right hepatic artery aneurysm with celiac atresia: endovascular therapy with a stent and detachable coils. J Vasc Interv Radiol. 19:1236–1240. DOI: 10.1016/j.jvir.2008.05.005. PMID: 18656020.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Right Gastroepiploic Artery Transposition for a Common Hepatic Artery and Proper Hepatic Artery Aneurysm Repair
- Endovascular Management of Hepatic Artery Pseudoaneurysms: A Case Series
- Endovascular Treatment of Multiple Pancreaticoduodenal Artery Aneurysms Associated with Celiac Artery Stenosis: A Case Report
- Kissing Aneurysms at Fenestrated Proximal Basilar Artery: Double-barrel Stent-assisted Coiling Using Dual Closed-cell Stents
- The Clinical Presentation and Treatment of Distal Posterior Inferior Cerebellar artery Aneurysms: Report on 2 cases