Obstet Gynecol Sci.
2021 May;64(3):248-256. 10.5468/ogs.20267.
Detection of small for gestational age in preterm prelabor rupture of membranes by Hadlock versus the Fetal Medicine Foundation growth charts
- Affiliations
-
- 1Department of Obstetrics and Gynecology, University of Tennessee Health Science Center, Memphis, TN, USA
- 2Department of Obstetrics and Gynecology, University of South Florida, Tampa, FL, USA
- 3Labor and Delivery Unit, Tampa General Hospital, Tampa, FL, USA
- 4Department of Obstetrics and Gynecology, University of Missouri at Kansas, Kansas City, MO, USA
- KMID: 2515976
- DOI: http://doi.org/10.5468/ogs.20267
Abstract
Objective
The primary outcome was to compare the diagnostic accuracy of neonatal small for gestational age (SGA) by the Hadlock and Fetal Medicine Foundation (FMF) charts in our cohort, followed by the ability to predict composite severe neonatal outcomes (SNO) in pregnancies with preterm prelabor rupture of membranes (PPROM).
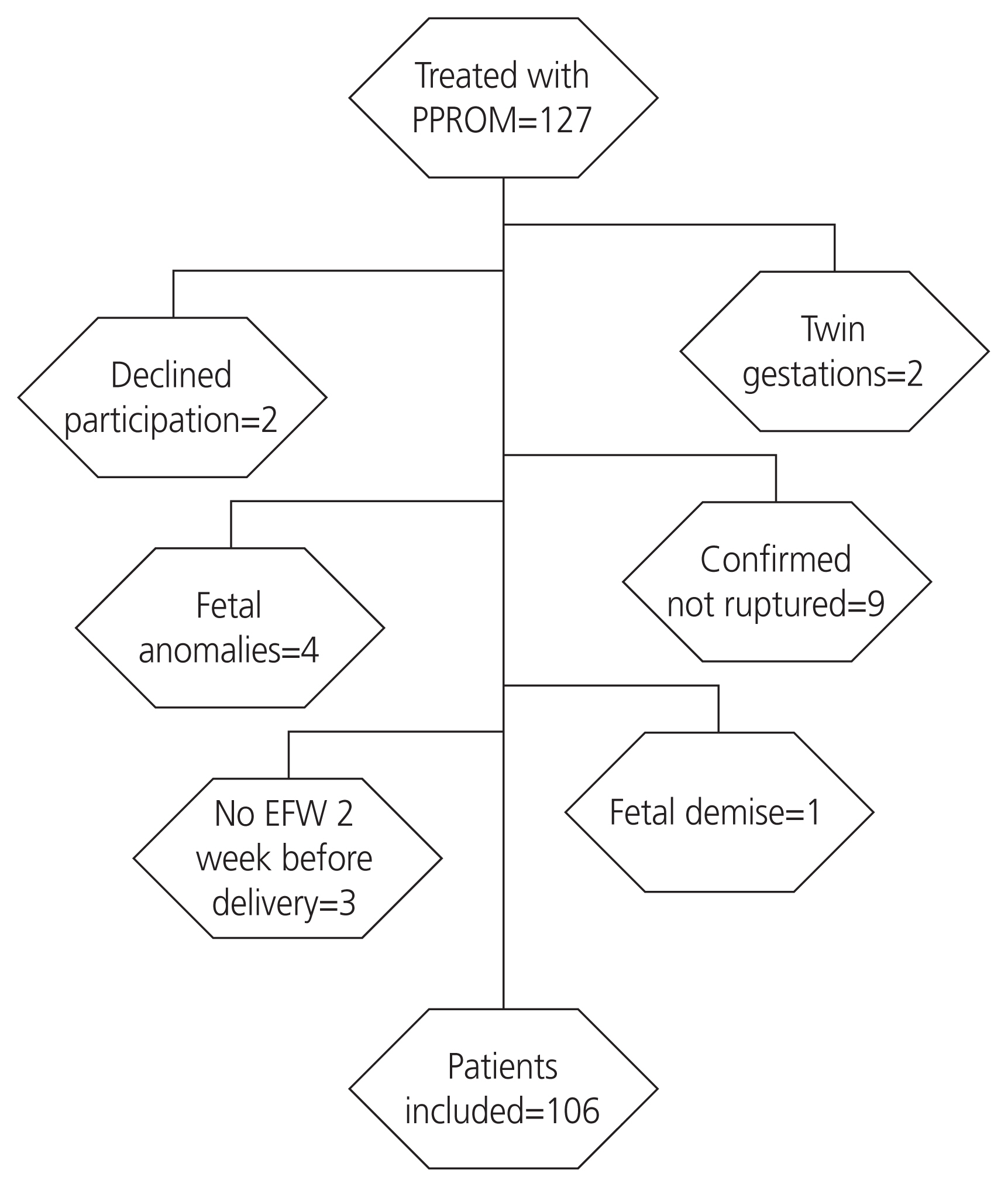
Methods
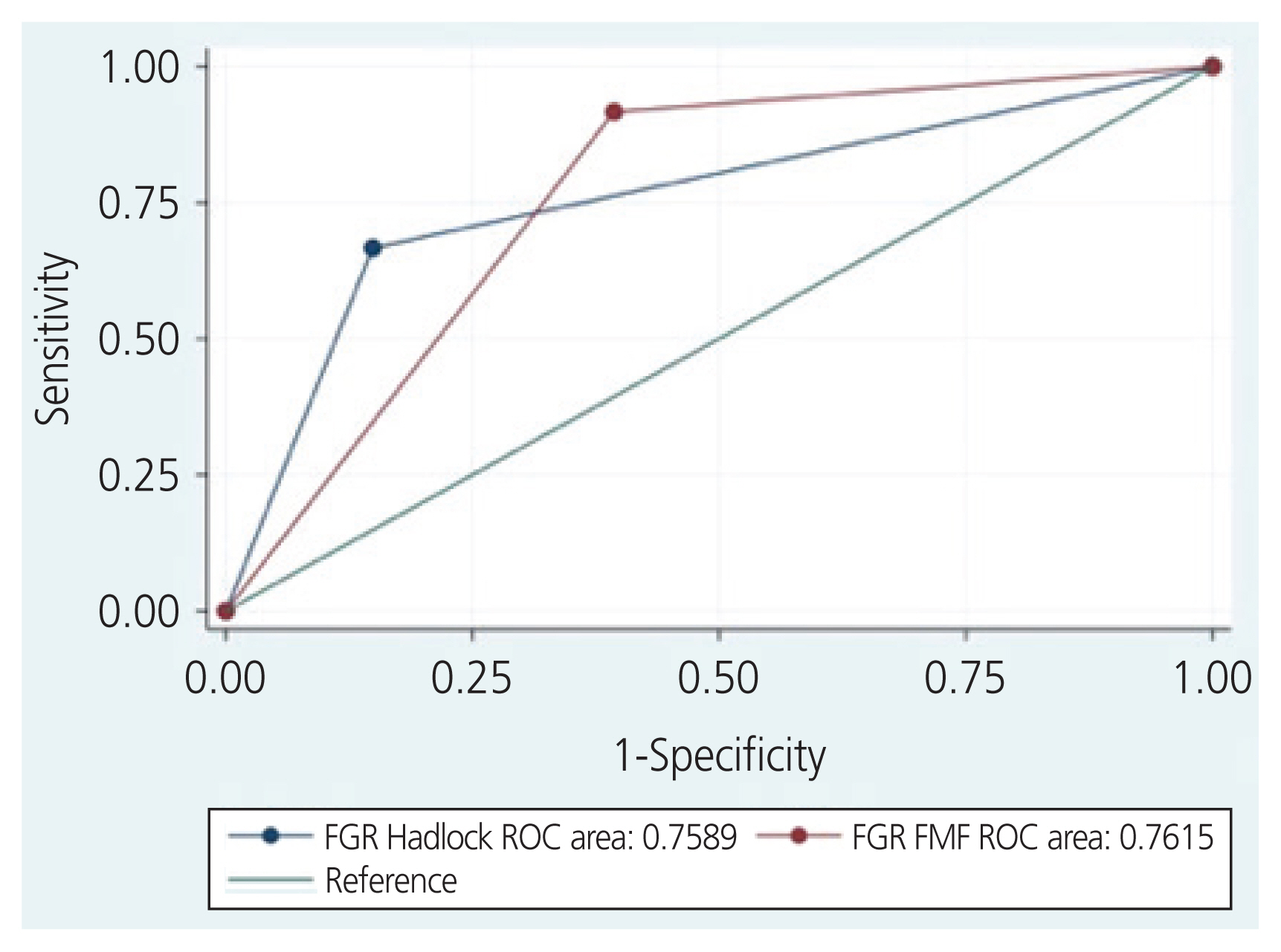
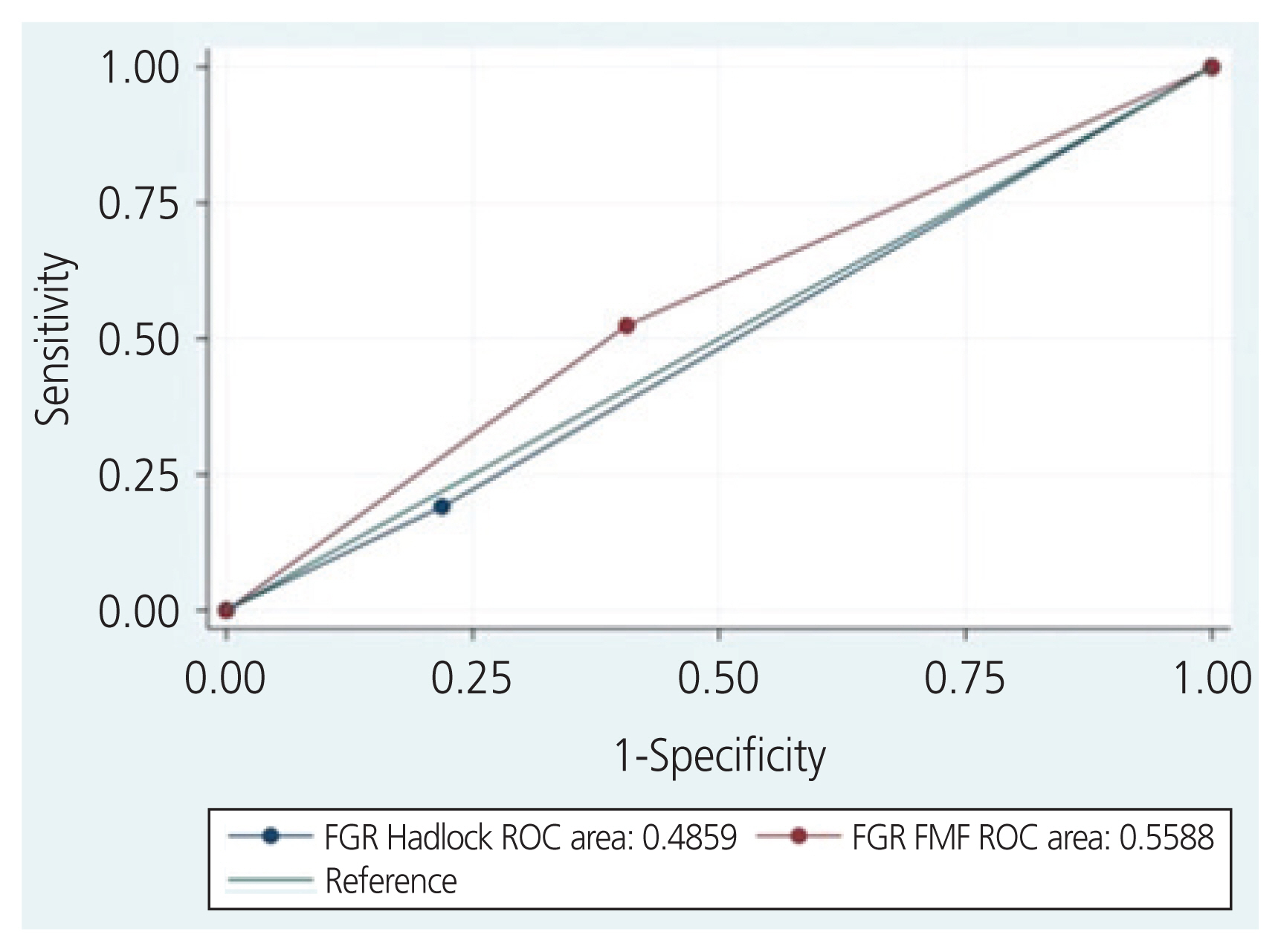
This study was a secondary analysis of a prospective cohort of pregnancies with PPROM from 2015 to 2018, from 23 to 36 completed weeks of gestation. Sensitivity, specificity, and positive and negative predictive values for the primary and secondary outcomes of the Hadlock and FMF fetal charts were calculated. The discriminatory ability of each chart was compared using the area under the receiver’s operating curves of clinical characteristics.
Results
Of the 106 women who met the inclusion criteria, 48 (45%) were screened positive using the FMF fetal growth chart and 22 (21%) were screened positive using the Hadlock chart. SGA was diagnosed in 12 infants (11%). Both fetal growth charts had comparable diagnostic accuracies and were statistically significant predictors of SGA (Hadlock: area under the receiver operating characteristic curves [AUC], 0.76, risk ratio [RR], 7.6, 95% confidence interval [CI], 2.5-23; and FMF: AUC, 0.76 RR, 13.3 95%CI 1.8-99.3). Both growth standards were poor predictors of SNO.
Conclusion
The Hadlock and FMF fetal growth charts have a similar accuracy to predict SGA in pregnancies complicated by PPROM. The FMF fetal growth chart may result in a 2-fold increase in positive screens, potentially increasing fetal surveillance.
Figure
Reference
-
References
1. American College of Obstetricians and Gynecologists’ Committee on Practice Bulletins-Obstetrics and the Society for Maternal-Fetal Medicine. ACOG practice bulletin No. 204: fetal growth restriction. Obstet Gynecol. 2019; 133:e97–109.2. American College of Obstetricians and Gynecologists’ Committee on Practice Bulletins-Obstetrics. Prelabor rupture of membranes: ACOG practice bulletin, number 217. Obstet Gynecol. 2020; 135:e80–97.3. Kim WJ, Han YS, Ko HS, Park IY, Shin JC, Wie JH. Antenatal corticosteroids and outcomes of preterm small-for-gestational-age neonates in a single medical center. Obstet Gynecol Sci. 2018; 61:7–13.
Article4. Kim SY, Kwon HS, Lee J, Sul AR, Ko HS, Yang JI. Questionnaire survey on the management of pregnant women with preterm premature rupture of membranes. Obstet Gynecol Sci. 2020; 63:286–92.
Article5. Hediger ML, Scholl TO, Schall JI, Miller LW, Fischer RL. Fetal growth and the etiology of preterm delivery. Obstet Gynecol. 1995; 85:175–82.
Article6. Monier I, Ancel PY, Ego A, Guellec I, Jarreau PH, Kaminski M, et al. Gestational age at diagnosis of early-onset fetal growth restriction and impact on management and survival: a population-based cohort study. BJOG. 2017; 124:1899–906.
Article7. Selvaratnam RJ, Davey MA, Anil S, McDonald SJ, Farrell T, Wallace EM. Does public reporting of the detection of fetal growth restriction improve clinical outcomes: a retrospective cohort study. BJOG. 2020; 127:581–9.
Article8. Gordijn SJ, Beune IM, Thilaganathan B, Papageorghiou A, Baschat AA, Baker PN, et al. Consensus definition of fetal growth restriction: a Delphi procedure. Ultrasound Obstet Gynecol. 2016; 48:333–9.
Article9. Molina LCG, Odibo L, Zientara S, Običan SG, Rodriguez A, Stout M, et al. Validation of the Delphi procedure consensus criteria for defining fetal growth restriction. Ultrasound Obstet Gynecol. 2020; 56:61–6.10. Hammami A, Mazer Zumaeta A, Syngelaki A, Akolekar R, Nicolaides KH. Ultrasonographic estimation of fetal weight: development of new model and assessment of performance of previous models. Ultrasound Obstet Gynecol. 2018; 52:35–43.
Article11. Kabiri D, Romero R, Gudicha DW, Hernandez-Andrade E, Pacora P, Benshalom-Tirosh N, et al. Prediction of adverse perinatal outcomes by fetal biometry: a comparison of customized and population-based standards. Ultrasound Obstet Gynecol. 2020; 55:177–88.12. Blue NR, Savabi M, Beddow ME, Katukuri VR, Fritts CM, Izquierdo LA, et al. The Hadlock method is superior to newer methods for the prediction of the birth weight percentile. J Ultrasound Med. 2019; 38:587–96.
Article13. Hadlock FP, Harrist RB, Sharman RS, Deter RL, Park SK. Estimation of fetal weight with the use of head, body, and femur measurements--a prospective study. Am J Obstet Gynecol. 1985; 151:333–7.
Article14. Hadlock FP, Harrist RB, Martinez-Poyer J. In utero analysis of fetal growth: a sonographic weight standard. Radiology. 1991; 181:129–33.
Article15. Blue NR, Beddow ME, Savabi M, Katukuri VR, Chao CR. Comparing the Hadlock fetal growth standard to the Eunice Kennedy Shriver National Institute of Child Health and Human Development racial/ethnic standard for the prediction of neonatal morbidity and small for gestational age. Am J Obstet Gynecol. 2018; 219:474.e1–12.
Article16. Nwabuobi C, Odibo L, Camisasca-Lopina H, Leavitt K, Tuuli M, Odibo AO. Comparing INTERGROWTH-21st Century and Hadlock growth standards to predict small for gestational age and short-term neonatal outcomes. J Matern Fetal Neonatal Med. 2020; 33:1906–12.
Article17. Tamura RK, Sabbagha RE, Dooley SL, Vaisrub N, Socol ML, Depp R. Real-time ultrasound estimations of weight in fetuses of diabetic gravid women. Am J Obstet Gynecol. 1985; 153:57–60.
Article18. GRIT Study Group. A randomised trial of timed delivery for the compromised preterm fetus: short term outcomes and Bayesian interpretation. BJOG. 2003; 110:27–32.19. Gardosi JO. Prematurity and fetal growth restriction. Early Hum Dev. 2005; 81:43–9.
Article20. Nicolaides KH, Wright D, Syngelaki A, Wright A, Akolekar R. Fetal Medicine Foundation fetal and neonatal population weight charts. Ultrasound Obstet Gynecol. 2018; 52:44–51.
Article21. Alexander GR, Himes JH, Kaufman RB, Mor J, Kogan M. A United States national reference for fetal growth. Obstet Gynecol. 1996; 87:163–8.
Article22. Bischoff A, Calvo-Garcia MA, Baregamian N, Levitt MA, Lim FY, Hall J, et al. Prenatal counseling for cloaca and cloacal exstrophy-challenges faced by pediatric surgeons. Pediatr Surg Int. 2012; 28:781–8.
Article23. Duncan JR, Tobiasz AM, Dorsett KM, Aziz MM, Thompson RE, Bursac Z, et al. Fetal pulmonary artery acceleration/ejection time prognostic accuracy for respiratory complications in preterm prelabor rupture of membranes. J Matern Fetal Neonatal Med. 2020; 33:2054–8.
Article24. Papile LA, Burstein J, Burstein R, Koffler H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J Pediatr. 1978; 92:529–34.
Article25. Bell MJ, Ternberg JL, Feigin RD, Keating JP, Marshall R, Barton L, et al. Neonatal necrotizing enterocolitis. Therapeutic decisions based upon clinical staging. Ann Surg. 1978; 187:1–7.26. Reddy UM, Abuhamad AZ, Levine D, Saade GR. Fetal Imaging Workshop Invited Participants. Fetal imaging: executive summary of a joint Eunice Kennedy Shriver National Institute of Child Health and Human Development, Society for Maternal-Fetal Medicine, American Institute of Ultrasound in Medicine, American College of Obstetricians and Gynecologists, American College of Radiology, Society for Pediatric Radiology, and Society of Radiologists in Ultrasound Fetal Imaging workshop. Obstet Gynecol. 2014; 123:1070–82.27. Duncan JR, Dorsett KM, Vilchez G, Schenone MH, Mari G. Uterine artery pulsatility index for the prediction of obstetrical complications in preterm prelabor rupture of membranes. J Matern Fetal Neonatal Med. 2019; Dec. 16. [Epub]. http://doi.org/10.1080/14767058.2019.1702961 .
Article28. Morris JM, Roberts CL, Bowen JR, Patterson JA, Bond DM, Algert CS, et al. Immediate delivery compared with expectant management after preterm pre-labour rupture of the membranes close to term (PPROMT trial): a randomised controlled trial. Lancet. 2016; 387:444–52.
Article29. Lorthe E, Ancel PY, Torchin H, Kaminski M, Langer B, Subtil D, et al. Impact of latency duration on the prognosis of preterm infants after preterm premature rupture of membranes at 24 to 32 weeks’ gestation: a national population-based cohort study. J Pediatr. 2017; 182:47–52.e2.
Article30. Spinillo A, Montanari L, Sanpaolo P, Bergante C, Chiara A, Fazzi E. Fetal growth and infant neurodevelopmental outcome after preterm premature rupture of membranes. Obstet Gynecol. 2004; 103:1286–93.
Article31. Parazzini F, Cortinovis I, Bortolus R, Zanardo V. Birth weight of infants born between the 23rd and 42nd gestational week in Italy. Pediatr Med Chir. 1998; 20:93–7.32. Papageorghiou AT, Ohuma EO, Altman DG, Todros T, Cheikh Ismail L, Lambert A, et al. International standards for fetal growth based on serial ultrasound measurements: the Fetal Growth Longitudinal Study of the INTERGROWTH-21st Project. Lancet. 2014; 384:869–79.
Article33. Buck Louis GM, Grewal J, Albert PS, Sciscione A, Wing DA, Grobman WA, et al. Racial/ethnic standards for fetal growth: the NICHD Fetal Growth Studies. Am J Obstet Gynecol. 2015; 213:449.e1–41.
Article34. Gardosi J, Francis A, Turner S, Williams M. Customized growth charts: rationale, validation and clinical benefits. Am J Obstet Gynecol. 2018; 218:S609–18.
Article35. Mercer BM. Preterm premature rupture of the membranes. Obstet Gynecol. 2003; 101:178–93.
Article36. Duncan JR, Schenone C, Dorset KM, Goedecke PJ, Tobiasz AM, Meyer NL, et al. Estimated fetal weight accuracy in pregnancies with preterm prelabor rupture of membranes by the Hadlock method. J Matern Fetal Neonatal Med. 2020. May. 22. [Epub]. http://doi.org/10.1080/14767058.2020.1769593 .
Article37. EXPRESS Group. Fellman V, Hellström-Westas L, Norman M, Westgren M, Källén K, et al. One-year survival of extremely preterm infants after active perinatal care in Sweden. JAMA. 2009; 301:2225–33.
Article38. Grace MR, Dotters-Katz S, Varner MW, Boggess K, Manuck TA. Birthweight extremes and neonatal and childhood outcomes after preterm premature rupture of membranes. Am J Perinatol. 2016; 33:1138–44.39. Ancel PY, Goffinet F, Kuhn P, Langer B, Matis J, et al. EPIPAGE-2 Writing Group. Survival and morbidity of preterm children born at 22 through 34 weeks’ gestation in France in 2011: results of the EPIPAGE-2 cohort study. JAMA Pediatr. 2015; 169:230–8.40. Duncan JR, Dorsett KM, Aziz MM, Bursac Z, Cleves MA, Talati AJ, et al. Estimated fetal weight and severe neonatal outcomes in preterm prelabor rupture of membranes. J Perinat Med. 2020; 48:687–93.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Iatrogenic Prelabor Premature Rupture of Membrane and Preterm Birth: an Experimental Mouse Study
- Current Approach in the Treatment of Preterm Premature Rupture of Membrane
- Measurement of Fetal Fibronectin for Diagnosis of Premature Rupture of Amniotic Membrane
- The Usefulness of Fetal Fibronectin as a Diagnostic Method of Preterm Ruptere of Membrane
- Preterm delivery in a primigravida with uterine adenomyosis