J Korean Neurosurg Soc.
2021 May;64(3):447-459. 10.3340/jkns.2020.0342.
Learning Curve and Complications Experience of Oblique Lateral Interbody Fusion : A Single-Center 143 Consecutive Cases
- Affiliations
-
- 1Department of Neurosurgery, Research Institute for Convergence of Biomedical Science and Technology, Pusan National University Yangsan Hospital, Yangsan, Korea
- 2Deparment of Neurosurgery, School of Medicine, Pusan National University, Yangsan, Korea
- KMID: 2515501
- DOI: http://doi.org/10.3340/jkns.2020.0342
Abstract
Objective
: Oblique lateral interbody fusion (OLIF) is becoming the preferred treatment for degenerative lumbar diseases. As beginners, we performed 143 surgeries over 19 months. In these consecutive cases, we analyzed the learning curve and reviewed the complications in our experience.
Methods
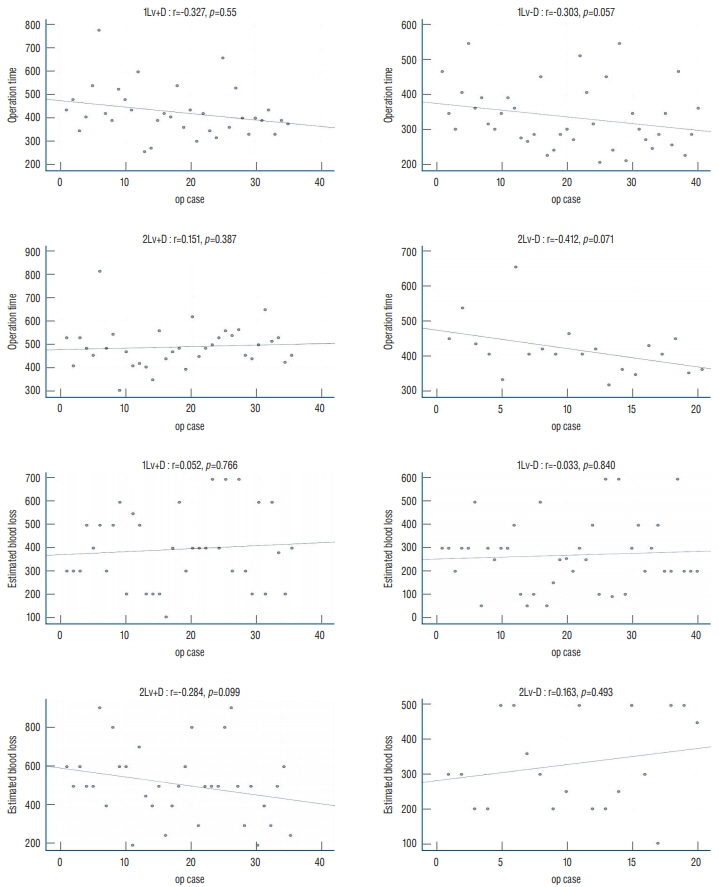
: This was a retrospective study; however, complications that were well known in the previous literature were strictly recorded prospectively. We followed up the changes in estimated blood loss (EBL), operation time, and transient psoas paresis according to case accumulation to analyze the learning curve.
Results
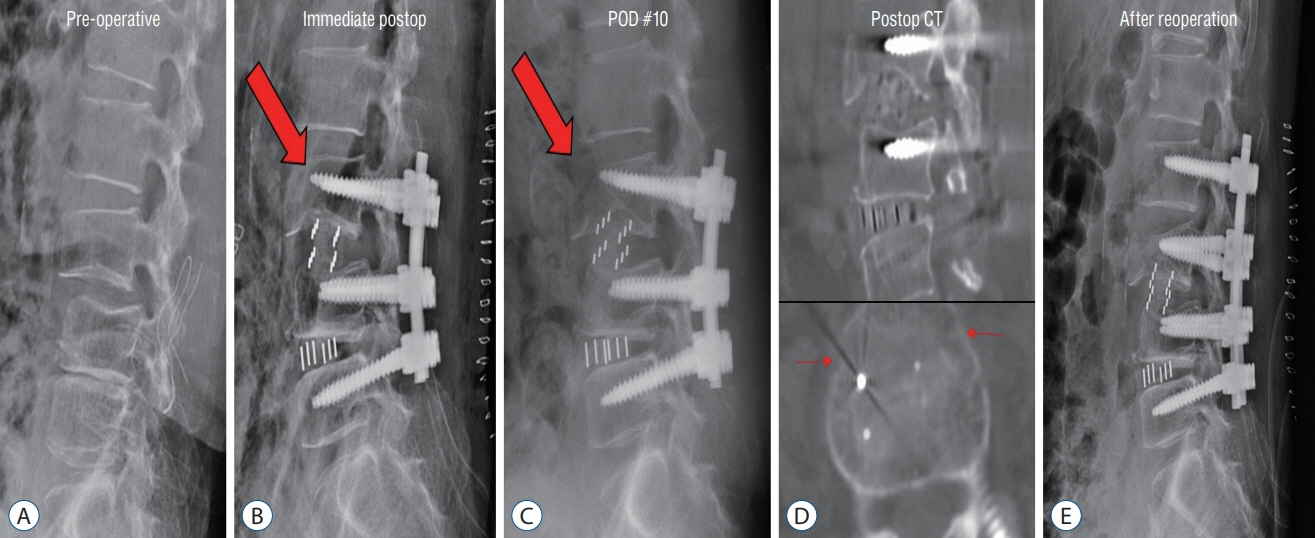
: Complication-free patients accounted for 43.6% (12.9%, early stage 70 patients and 74.3%, late stage 70 patients). The most common complication was transient psoas paresis (n=52). Most of these complications occurred in the early stages of learning. C-reactive protein normalization was delayed in seven patients (4.89%). The operation time showed a decreasing trend with the cases; however, EBL did not show any significant change. Notable operation-induced complications were cage malposition, vertebral body fracture, injury to the ureter, and injury to the lumbar vein.
Conclusion
: According to the learning curve, the operation time and psoas paresis decreased. It is important to select an appropriately sized cage along with clear dissection of the anterior border of the psoas muscle to prevent OLIF-specific complications.
Keyword
Figure
Reference
-
References
1. Abbasi H, Abbasi A. Oblique lateral lumbar interbody fusion (OLLIF): technical notes and early results of a single surgeon comparative study. Cureus. 7:e351. 2015.
Article2. Abbasi H, Miller L, Abbasi A, Orandi V, Khaghany K. Minimally invasive scoliosis surgery with oblique lateral lumbar interbody fusion: single surgeon feasibility study. Cureus. 9:e1389. 2017.
Article3. Abe K, Orita S, Mannoji C, Motegi H, Aramomi M, Ishikawa T, et al. Perioperative complications in 155 patients who underwent oblique lateral interbody fusion surgery: perspectives and indications from a retrospective, multicenter survey. Spine (Phila Pa 1976). 42:55–62. 2017.
Article4. Boghani Z, Steele WI, Barber SM, Lee JJ, Sokunbi O, Blacklock JB, et al. Variability in the size of the retroperitoneal oblique corridor: a magnetic resonance imaging-based analysis. Surg Neurol Int. 11:54. 2020.
Article5. Brier-Jones JE, Palmer DK, Ĭnceoğlu S, Cheng WK. Vertebral body fractures after transpsoas interbody fusion procedures. Spine J. 11:1068–1072. 2011.
Article6. Chung NS, Lee HD, Jeon CH. Accuracy of the lateral cage placement under intraoperative C-arm fluoroscopy in oblique lateral interbody fusion. J Orthop Sci. 23:918–922. 2018.
Article7. DiGiorgio AM, Edwards CS, Virk MS, Mummaneni PV, Chou D. Stereotactic navigation for the prepsoas oblique lateral lumbar interbody fusion: technical note and case series. Neurosurg Focus. 43:E14. 2017.
Article8. Fujibayashi S, Hynes RA, Otsuki B, Kimura H, Takemoto M, Matsuda S. Effect of indirect neural decompression through oblique lateral interbody fusion for degenerative lumbar disease. Spine (Phila Pa 1976). 40:E175–E182. 2015.
Article9. Fujibayashi S, Kawakami N, Asazuma T, Ito M, Mizutani J, Nagashima H, et al. Complications associated with lateral interbody fusion: nation-wide survey of 2998 cases during the first 2 years of its use in Japan. Spine (Phila Pa 1976). 42:1478–1484. 2017.
Article10. Fujibayashi S, Otsuki B, Kimura H, Tanida S, Masamoto K, Matsuda S. Preoperative assessment of the ureter with dual-phase contrast-enhanced computed tomography for lateral lumbar interbody fusion procedures. J Orthop Sci. 22:420–424. 2017.
Article11. Heo DH, Kim JS. Clinical and radiological outcomes of spinal endoscopic discectomy-assisted oblique lumbar interbody fusion: preliminary results. Neurosurg Focus. 43:E13. 2017.
Article12. Huang C, Xu Z, Li F, Chen Q. Does the access angle change the risk of approach-related complications in minimally invasive lateral lumbar interbody fusion? An MRI study. J Korean Neurosurg Soc. 61:707–715. 2018.
Article13. Hwang JU, Son DW, Kang KT, Lee SH, Lee JS, Song GS, et al. Importance of hemoglobin A1c levels for the detection of post-surgical infection following single-level lumbar posterior fusion in patients with diabetes. Korean J Neurotrauma. 15:150–158. 2019.
Article14. Jin C, Jaiswal MS, Jeun SS, Ryu KS, Hur JW, Kim JS. Outcomes of oblique lateral interbody fusion for degenerative lumbar disease in patients under or over 65 years of age. J Orthop Surg Res. 13:38. 2018.15. Jin J, Ryu KS, Hur JW, Seong JH, Kim JS, Cho HJ. Comparative study of the difference of perioperative complication and radiologic results: MISDLIF (minimally invasive direct lateral lumbar interbody fusion) versus MIS-OLIF (minimally invasive oblique lateral lumbar interbody fusion). Clin Spine Surg. 31:31–36. 2018.
Article16. Kang KT, Son DW, Lee SH, Song GS, Sung SK, Lee SW. Variation of Creactive protein and white blood cell counts in spinal operation: primary fusion surgery versus revision fusion surgery. Korean J Spine. 14:66–70. 2017.
Article17. Kim SB, Won YG, Lee JS, Ahn JS, Kang C, Lee GS. Vertebral body fracture after oblique lumbar interbody fusion in 2 patients: a case report. J Korean Soc Spine Surg. 25:35–39. 2018.
Article18. Kraiwattanapong C, Arnuntasupakul V, Kantawan R, Keorochana G, Lertudomphonwanit T, Sirijaturaporn P, et al. Malposition of cage in minimally invasive oblique lumbar interbody fusion. Case Rep Orthop. 2018:9142074. 2018.
Article19. Li HM, Zhang RJ, Shen CL. Differences in radiographic and clinical outcomes of oblique lateral interbody fusion and lateral lumbar interbody fusion for degenerative lumbar disease: a meta-analysis. BMC Musculoskelet Disord. 20:582. 2019.
Article20. Li J, Wang X, Sun Y, Zhang F, Gao Y, Li Z, et al. Safety analysis of two anterior lateral lumbar interbody fusions at the initial stage of learning curve. World Neurosurg. 127:e901–e909. 2019.
Article21. Miscusi M, Ramieri A, Forcato S, Giuffrè M, Trungu S, Cimatti M, et al. Comparison of pure lateral and oblique lateral inter-body fusion for treatment of lumbar degenerative disk disease: a multicentric cohort study. Eur Spine J. 27(Suppl 2):222–228. 2018.
Article22. Ohtori S, Orita S, Yamauchi K, Eguchi Y, Ochiai N, Kishida S, et al. Miniopen anterior retroperitoneal lumbar interbody fusion: oblique lateral interbody fusion for lumbar spinal degeneration disease. Yonsei Med J. 56:1051–1059. 2015.
Article23. Quillo-Olvera J, Lin GX, Jo HJ, Kim JS. Complications on minimally invasive oblique lumbar interbody fusion at L2-L5 levels: a review of the literature and surgical strategies. Ann Transl Med. 6:101. 2018.
Article24. Sato J, Ohtori S, Orita S, Yamauchi K, Eguchi Y, Ochiai N, et al. Radiographic evaluation of indirect decompression of mini-open anterior retroperitoneal lumbar interbody fusion: oblique lateral interbody fusion for degenerated lumbar spondylolisthesis. Eur Spine J. 26:671–678. 2017.
Article25. Silvestre C, Mac-Thiong JM, Hilmi R, Roussouly P. Complications and morbidities of mini-open anterior retroperitoneal lumbar interbody fusion: oblique lumbar interbody fusion in 179 patients. Asian Spine J. 6:89–97. 2012.
Article26. Suri P, Rainville J, Kalichman L, Katz JN. Does this older adult with lower extremity pain have the clinical syndrome of lumbar spinal stenosis? JAMA. 304:2628–2636. 2010.
Article27. Woods K, Fonseca A, Miller LE. Two-year outcomes from a single surgeon’s learning curve experience of oblique lateral interbody fusion without intraoperative neuromonitoring. Cureus. 9:e1980. 2017.28. Woods KR, Billys JB, Hynes RA. Technical description of oblique lateral interbody fusion at L1-L5 (OLIF25) and at L5-S1 (OLIF51) and evaluation of complication and fusion rates. Spine J. 17:545–553. 2017.
Article29. Xu DS, Walker CT, Godzik J, Turner JD, Smith W, Uribe JS. Minimally invasive anterior, lateral, and oblique lumbar interbody fusion: a literature review. Ann Transl Med. 6:104. 2018.
Article30. Zeng ZY, Xu ZW, He DW, Zhao X, Ma WH, Ni WF, et al. Complications and prevention strategies of oblique lateral interbody fusion technique. Orthop Surg. 10:98–106. 2018.
Article31. Zhu G, Hao Y, Yu L, Cai Y, Yang X. Comparing stand-alone oblique lumbar interbody fusion with posterior lumbar interbody fusion for revision of rostral adjacent segment disease: a STROBE-compliant study. Medicine (Baltimore). 97:e12680. 2018.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Minimally Invasive Lateral Lumbar Interbody Fusion: Indications, Outcomes and Complications
- Laparoscopy Assisted Miniopen Lateral Approach for Anterior Lumbar Interbody Fusion
- Morphometric Analysis of the Ureter with Respect to Lateral Lumbar Interbody Fusion Using Contrast-Enhanced Computed Tomography
- Pearls and Pitfalls of Oblique Lateral Interbody Fusion: A Comprehensive Narrative Review
- Oblique Posterior Interbody Fusion with Bone Plugs by Unilateral Approach for Treatment of Lumbar Instability: Technical Note