Brain Tumor Res Treat.
2021 Apr;9(1):26-30. 10.14791/btrt.2021.9.e4.
Surgical Experience of Posterior Fossa Meningioma in a Jehovah’s Witnesses Patient
- Affiliations
-
- 1Department of Neurosurgery, Wonkwang University School of Medicine, Iksan, Korea
- KMID: 2515079
- DOI: http://doi.org/10.14791/btrt.2021.9.e4
Abstract
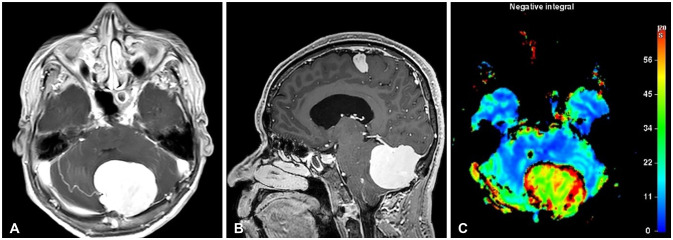
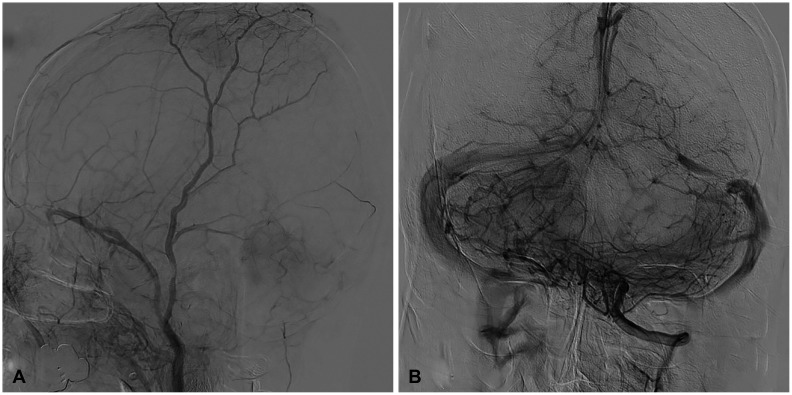
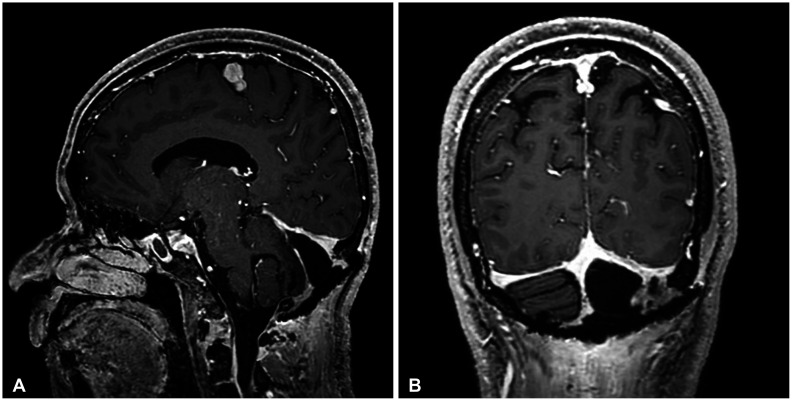
- Unexpected bleeding is a common complication that can occur during surgery. This unexpected bleeding can be managed by checking the patients’ preoperative hemodynamic state or by autologous transfusion of an appropriate volume during surgery depending on the amount of blood loss and hemodynamic condition. However, patients like Jehovah’s Witnesses, who refuse autologous transfusions for religious reasons even in life-threatening situations, present a predicament for treating physicians. The author reports on a large meningioma on the posterior fossa of a Jehovah’s Witness patient who underwent surgery without autologous blood transfusion. There were no major problems other than the fear of unexpected massive bleeding. The surgeon’s attention and efforts to minimize bleeding during surgery seemed to be the most important factors for success.
Keyword
Figure
Reference
-
1. Goodnough LT, Brecher ME. Autologous blood transfusion. Intern Med. 1998; 37:238–245. PMID: 9617857.2. Suess S, Suess O, Brock M. Neurosurgical procedures in Jehovah's Witnesses: an increased risk? Neurosurgery. 2001; 49:266–272. discussion 272-3. PMID: 11504102.3. Watch Tower Bible and Tract Society of Pennsylvania. Hospital Liaison Committees for Jehovah's Witnesses. New York, NY: Watch Tower Bible and Tract Society of Pennsylvania;2012. Accessed October 21, 2020. at https://www.jw.org/en/medical-library/strategies-downloads/hospital-liaison-committees-jehovahs-witnesses/.4. American Society of Anesthesiologists Task Force on Perioperative Blood Management. Practice guidelines for perioperative blood management: an updated report by the American Society of Anesthesiologists Task Force on Perioperative Blood Management. Anesthesiology. 2015; 122:241–275. PMID: 25545654.5. Spence RK. Surgical red blood cell transfusion practice policies. Am J Surg. 1995; 170(6 Suppl 1):S3–S15.6. Carson JL. Morbidity risk assessment in the surgically anemic patient. Am J Surg. 1995; 170(6 Suppl 1):S32–S36.7. Supreme Court of Korea. Jehovah's Witnesses Death During Bloodless Surgery. Seoul: Supreme Court of Korea;2014. Accessed September 9, 2020. at https://www.scourt.go.kr/portal/news/NewsViewAction.work?seqnum=4557&gubun=4&searchOption=&searchWord=.8. Lindstrom E, Johnstone R. Acute normovolemic hemodilution in a Jehovah's Witness patient: a case report. AANA J. 2010; 78:326–330. PMID: 20879634.9. Yang SA, Park SW, Kim KS. Acute normovolemic hemodilution in Jehovah's Witness. J Kyung Hee Univ Med Cent. 2015; 30:74–77.10. Lin S, McKenna SJ, Yao CF, Chen YR, Chen C. Effects of hypotensive anesthesia on reducing intraoperative blood loss, duration of operation, and quality of surgical field during orthognathic surgery: a systematic review and meta-analysis of randomized controlled trials. J Oral Maxillofac Surg. 2017; 75:73–86. PMID: 27542543.11. Michelson AD, MacGregor H, Barnard MR, Kestin AS, Rohrer MJ, Valeri CR. Reversible inhibition of human platelet activation by hypothermia in vivo and in vitro. Thromb Haemost. 1994; 71:633–640. PMID: 7522354.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Biomedical Ethics for Jehovah’s Witnesses and Patient Blood Management
- Hip Joint Surgery without Transfusion in Patients Who Were Jehovah's Witnesses: A Report of Two Cases
- Experience of a Bloodless Two-Jaw Surgery and Care in Jehovah's Witnesses with Anemia
- Anesthesia for a Jehovah's Witness Patient Experiencing Unexpected Perioperative Hemorrhage: A Case Report
- Liver transplantation in Jehovah's Witnesses: two cases report