Anat Cell Biol.
2021 Mar;54(1):124-127. 10.5115/acb.20.237.
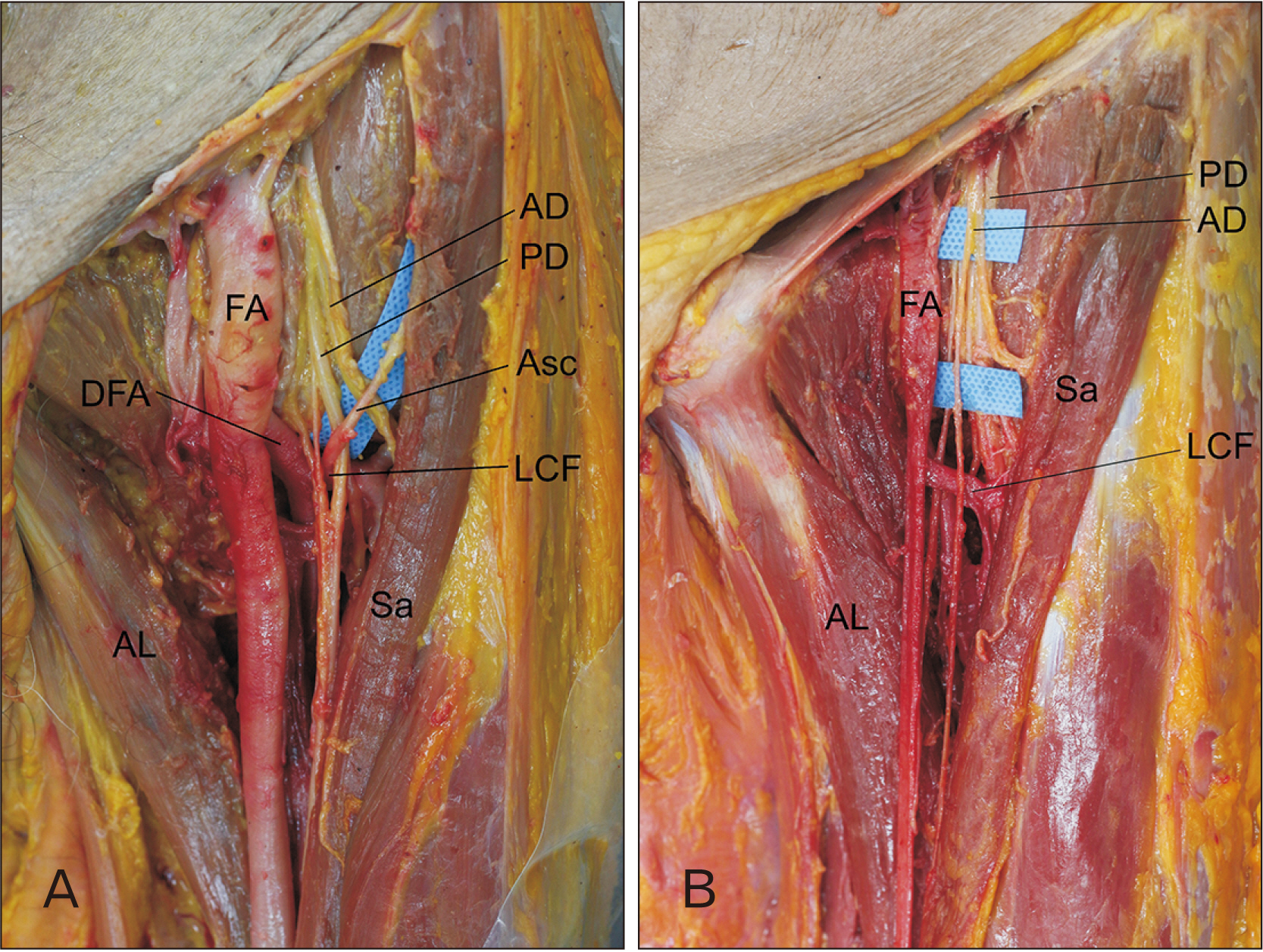
The ascending branch of the lateral circumflex femoral artery penetrating the posterior division of the femoral nerve
- Affiliations
-
- 1Department of Anatomy, College of Medicine, The Catholic University of Korea, Seoul,
- 2The Catholic Institute for Applied Anatomy, College of Medicine, The Catholic University of Korea, Seoul, Korea
- KMID: 2514592
- DOI: http://doi.org/10.5115/acb.20.237
Abstract
- Understanding anatomic variations in neurovascular structure inside the femoral triangle is crucial for regional anesthesiologists performing femoral nerve block. During routine dissection of a cadaver, an ascending branch of the lateral circumflex femoral artery with an anomalous course passing through the femoral nerve, specifically the posterior division, was identified inside the femoral triangle on the left thigh. The novel variation identified in this study occurred in an early stage of prenatal development. Recognition of this anatomic variation will be helpful for reducing unexpected complications during the femoral nerve block and the tensor fascia latae flap. Penetration of the posterior division of the femoral nerve by the arterial branch might cause pain or paresthesia of the medial aspect of the leg in the distribution of the saphenous nerve.
Figure
Reference
-
References
1. Standring S, Gray H. 2016. Gray's anatomy: the anatomical basis of clinical practice. 41st ed. Elsevier;Philadelphia:2. Ishiguro S, Yokochi A, Yoshioka K, Asano N, Deguchi A, Iwasaki Y, Sudo A, Maruyama K. 2012; Technical communication: anatomy and clinical implications of ultrasound-guided selective femoral nerve block. Anesth Analg. 115:1467–70. DOI: 10.1213/ANE.0b013e31826af956. PMID: 22886842.3. Anloague PA, Huijbregts P. 2009; Anatomical variations of the lumbar plexus: a descriptive anatomy study with proposed clinical implications. J Man Manip Ther. 17:e107–14. DOI: 10.1179/106698109791352201. PMID: 20140146. PMCID: PMC2813498.
Article4. Unat F, Sirinturk S, Cagimni P, Pinar Y, Govsa F, Nteli Chatzioglou G. 2018; Macroscopic observations of muscular bundles of accessory iliopsoas muscle as the cause of femoral nerve compression. J Orthop. 16:64–8. DOI: 10.1016/j.jor.2018.12.009. PMID: 30662241. PMCID: PMC6324757.
Article5. Wong TL, Kikuta S, Iwanaga J, Tubbs RS. 2019; A multiply split femoral nerve and psoas quartus muscle. Anat Cell Biol. 52:208–10. DOI: 10.5115/acb.2019.52.2.208. PMID: 31338239. PMCID: PMC6624330.
Article6. Saadeh FA, Haikal FA, Abdel-Hamid FA. 1998; Blood supply of the tensor fasciae latae muscle. Clin Anat. 11:236–8. DOI: 10.1002/(SICI)1098-2353(1998)11:4<236::AID-CA2>3.0.CO;2-P. PMID: 9652537.
Article7. Keen JA. 1961; A study of the arterial variations in the limbs, with special reference to symmetry of vascular patterns. Am J Anat. 108:245–61. DOI: 10.1002/aja.1001080303. PMID: 14454801.
Article8. Senior HD. 1925; An interpretation of the recorded arterial anomalies of the human pelvis and thigh. Am J Anat. 36:1–46. DOI: 10.1002/aja.1000360102.
Article9. Ciftcioğlu E, Kale A, Kopuz C, Edizer M, Aydin E, Demir MT. 2009; Medial circumflex femoral artery with different origin and course: a case report and review of the literature. Folia Morphol (Warsz). 68:188–91. PMID: 19722165.10. Patrick BS. 2005; Unusual nerve-artery relationship in microvascular exploration for tic douloureux. Neurosurgery. 56:E629. DOI: 10.1227/01.NEU.0000155083.39755.53. PMID: 18235264.
Article11. Helbig GM, Callahan JD, Cohen-Gadol AA. 2009; Variant intraneural vein-trigeminal nerve relationships: an observation during microvascular decompression surgery for trigeminal neuralgia. Neurosurgery. 65:958–61. discussion 961DOI: 10.1227/01.NEU.0000351757.29658.C0. PMID: 19834410.12. Zheng X, Feng B, Hong W, Zhang W, Yang M, Tang Y, Zhong J, Hua X, Li S. 2012; Management of intraneural vessels during microvascular decompression surgery for trigeminal neuralgia. World Neurosurg. 77:771–4. DOI: 10.1016/j.wneu.2011.08.031. PMID: 22120295.
Article13. Feng BH, Zheng XS, Wang XH, Ying TT, Yang M, Tang YD, Li ST. 2015; Management of vessels passing through the facial nerve in the treatment of hemifacial spasm. Acta Neurochir (Wien). 157:1935–40. discussion 1940DOI: 10.1007/s00701-015-2562-x. PMID: 26329733.
Article14. Oh CH, Shim YS, Park H, Kim EY. 2015; A case of hemifacial spasm caused by an artery passing through the facial nerve. J Korean Neurosurg Soc. 57:221–4. DOI: 10.3340/jkns.2015.57.3.221. PMID: 25810866. PMCID: PMC4373055.
Article15. Muhly WT, Orebaugh SL. 2011; Ultrasound evaluation of the anatomy of the vessels in relation to the femoral nerve at the femoral crease. Surg Radiol Anat. 33:491–4. DOI: 10.1007/s00276-010-0755-9. PMID: 21132494.
Article16. Lechner G, Jantsch H, Waneck R, Kretschmer G. 1988; The relationship between the common femoral artery, the inguinal crease, and the inguinal ligament: a guide to accurate angiographic puncture. Cardiovasc Intervent Radiol. 11:165–9. DOI: 10.1007/BF02577111. PMID: 3139299.
Article17. Jeng CL, Torrillo TM, Rosenblatt MA. 2010; Complications of peripheral nerve blocks. Br J Anaesth. 105 Suppl 1:i97–107. DOI: 10.1093/bja/aeq273. PMID: 21148659.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Origin of Main Branches of the Femoral Artery in Korean Adults
- Reconstruction of Trochanteric Pressure Sores using Perforator-based Flap from the Ascending Branch of Lateral Circumflex Femoral Artery
- Anatomic Analysis of Rectus Femoris Functional Flap in Korean
- Injury of the Ascending Branch of the Lateral Femoral Circumflex Artery Caused by a Spike of the Displaced Lesser Trochanter in an Intertrochanteric Femoral Fracture - A Case Report -
- Anatomical and Radiological Study of the Vascular Distribution and Skin Territory for the Tensor Fasciae Latae Free Flap