J Liver Cancer.
2021 Mar;21(1):92-96. 10.17998/jlc.21.1.92.
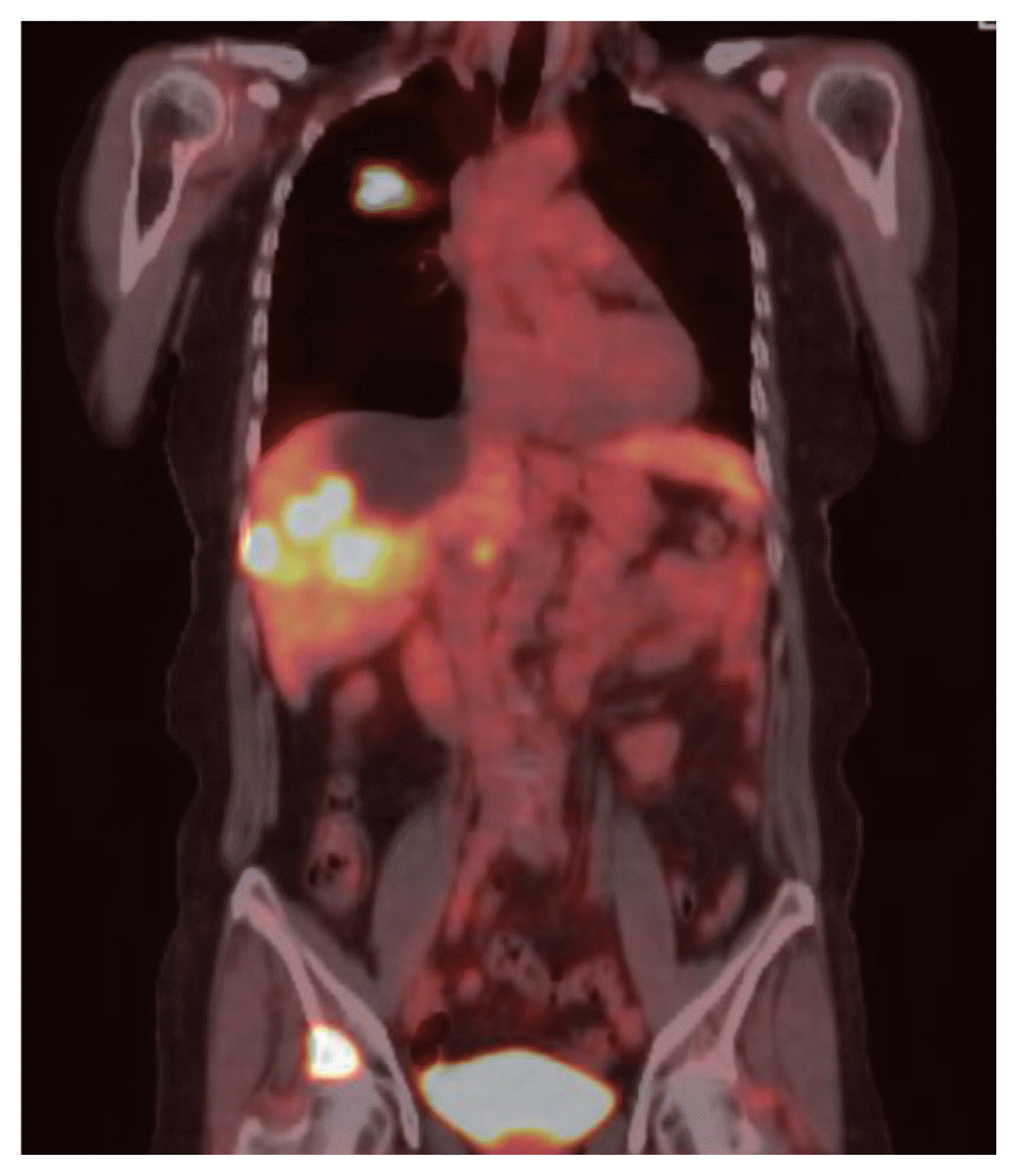
A Case of Metastatic Melanoma in the Liver Mimicking Hepatocellular Carcinoma
- Affiliations
-
- 1Department of Internal Medicine, Chonnam National University Medical School, Gwangju, Korea
- KMID: 2514240
- DOI: http://doi.org/10.17998/jlc.21.1.92
Abstract
- The liver is one of the most common sites of metastasis. Although most metastatic liver cancers are hypovascular, some hypervascular metastases, such as those from melanoma, need to be differentiated from hepatocellular carcinoma (HCC) because they may show similar radiologic findings due to their hypervascularity. We encountered a case of multinodular liver masses with hyperenhancement during the arterial phase and washout during the portal venous and delayed phases, which were consistent with imaging hallmarks of HCC. The patient had a history of malignant melanoma and had undergone curative resection 11 years earlier. We performed a liver biopsy for pathologic confirmation, which revealed a metastatic melanoma of the liver. Metastatic liver cancer should be considered if a patient without chronic liver disease has a history of other primary malignancies, and caution should be exercised with hypervascular cancers that may mimic HCC.
Figure
Reference
-
1. Korean Liver Cancer Association; National Cancer Center. 2018 Korean Liver Cancer Association-National Cancer Center Korea Practice Guidelines for the Management of Hepatocellular Carcinoma. Gut Liver. 2019; 13:227–299.2. Ros PR, Erturk SM. Malignant tumors of the liver. Gore RM, Levine MS, editors. Textbook of gastrointestinal radiology. 2:4th ed. Philadephia: Saunders;2015. p. 1561–1607.3. Matos AP, Velloni F, Ramalho M, AlObaidy M, Rajapaksha A, Semelka RC. Focal liver lesions: practical magnetic resonance imaging approach. World J Hepatol. 2015; 7:1987–2008.4. Kim YY, Park MS, Aljoqiman KS, Choi JY, Kim MJ. Gadoxetic acid-enhanced magnetic resonance imaging: Hepatocellular carcinoma and mimickers. Clin Mol Hepatol. 2019; 25:223–233.5. Chou R, Cuevas C, Fu R, Devine B, Wasson N, Ginsburg A, et al. Imaging techniques for the diagnosis of hepatocellular carcinoma: a systematic review and meta-analysis. Ann Intern Med. 2015; 162:697–711.6. Lee YJ, Lee JM, Lee JS, Lee HY, Park BH, Kim YH, et al. Hepatocellular carcinoma: diagnostic performance of multidetector CT and MR imaging-a systematic review and meta-analysis. Radiology. 2015; 275:97–109.7. Wang S, Feng Y, Swinnen J, Oyen R, Li Y, Ni Y. Incidence and prognosis of liver metastasis at diagnosis: a pan-cancer population-based study. Am J Cancer Res. 2020; 10:1477–1517.8. Oh CM, Cho H, Won YJ, Kong HJ, Roh YH, Jeong KH, et al. Nationwide trends in the incidence of melanoma and non-melanoma skin cancers from 1999 to 2014 in South Korea. Cancer Res Treat. 2018; 50:729–737.9. Patel JK, Didolkar MS, Pickren JW, Moore RH. Metastatic pattern of malignant melanoma. A study of 216 autopsy cases. Am J Surg. 1978; 135:807–810.10. Barth A, Wanek LA, Morton DL. Prognostic factors in 1,521 melanoma patients with distant metastases. J Am Coll Surg. 1995; 181:193–201.11. NCCN clinical practice guidelines in oncolology. Melanoma: Cutaneous (version 1.2021) [Internet]. Plymouth Meeting, PA: National Comprehensive Cancer Network;[cited 2020 Nov 25]. Available from: https://www.nccn.org/professionals/physician_gls/pdf/cutaneous_melanoma.pdf.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Metastatic Omental Hepatocellular Carcinoma: Two Cases Report
- A Case of Metastatic Conjunctival Tumor
- Cytologic Diagnosis of Metastatic Hepatocellular Carcinoma by Aspiration Cytology of Sacrum
- A Case of Metastatic Malignant Melanoma of the Liver Resulting from Choroidal Melanoma
- Cell proliferation index and the expression of p53 and Bcl-2 in tumorous and non-tumorous lesions of hepatocellular carcinoma and metastatic liver cancer