J Korean Med Sci.
2021 Mar;36(11):e76. 10.3346/jkms.2021.36.e76.
Hand Grip and Leg Muscle Strength in Hemodialysis Patients and Its Determinants
- Affiliations
-
- 1Department of Internal Medicine, National Medical Center, Seoul, Korea
- KMID: 2514052
- DOI: http://doi.org/10.3346/jkms.2021.36.e76
Abstract
- Background
Chronic kidney disease is associated with chronic inflammation and progressive loss of peripheral muscle strength and the ability to exercise, and these changes are highly pronounced in patients receiving hemodialysis (HD). We evaluated hand grip strength (HGS) and leg muscle strength (LMS) in patients receiving HD and attempted to identify factors associated with muscle strength.
Methods
We screened HGS (opposite the fistula side) and LMS (both sides) in HD patients at a single center (n = 112) by using digital hand and leg dynamometers (T.K.K. 5401 and 5710e/5715, Takei Scientific Instruments Co. Ltd., Niigata, Japan).
Results
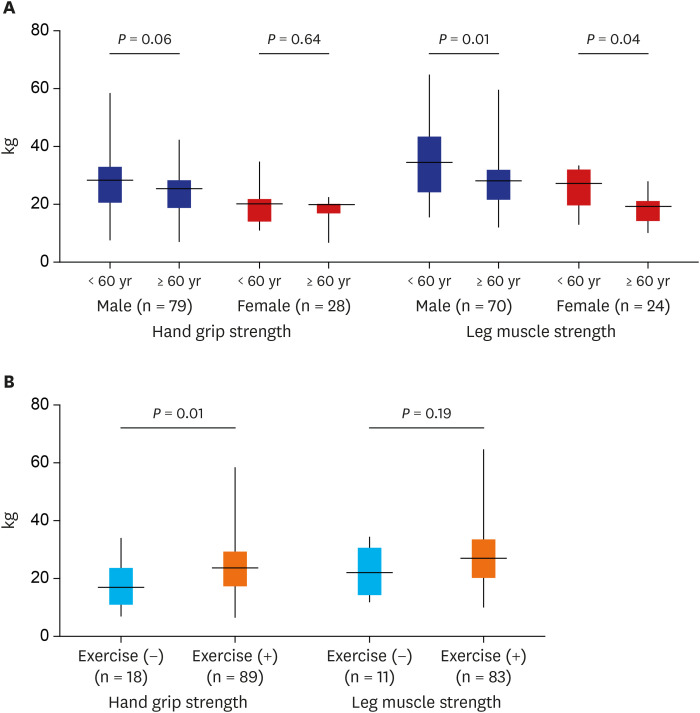
The mean age of patients was 62.6 years, and 73.2% of the patients were male. Diabetes was the cause of kidney failure in 50% of the patients, and the median HD vintage was 34 months. A total of 77.7% of patients reported that they participated in regular home-based exercise, and 29.5% of patients regularly participated in hospital-based resistance exercise. HGS and LMS showed good correlation (r = 0.715, P < 0.001). HGS (25.1 vs. 17.0 kg) and LMS (30.1 vs. 20.4 kg) were greater in males (P < 0.001 and P < 0.001, respectively) than in females. Older patients (≥ 60 years) showed less LMS than younger patients in both males and females (P = 0.012 and P = 0.037, respectively), but HGS did not differ according to age. Patients performing regular home- or hospital-based exercise showed higher HGS than those who did not exercise (24.2 vs. 18.6 kg, P = 0.011), but LMS was not significantly different (29.3 vs. 23.6 kg, P = 0.185). Multiple linear regression analysis proved that male sex, younger age, and any type of exercise were factors associated with improved HGS and LMS. Groups of older age (≥ 60 years), male sex, and shorter duration of HD (< median) benefitted more from exercise.
Conclusion
Sex, age, and exercise were the most important determinants of muscle strength in HD patients. We need to encourage patients to engage in regular home or group exercise from the beginning of dialysis and introduce new feasible forms of exercise for HD patients.
Figure
Reference
-
1. Fouque D, Kalantar-Zadeh K, Kopple J, Cano N, Chauveau P, Cuppari L, et al. A proposed nomenclature and diagnostic criteria for protein-energy wasting in acute and chronic kidney disease. Kidney Int. 2008; 73(4):391–398. PMID: 18094682.
Article2. Hanna RM, Ghobry L, Wassef O, Rhee CM, Kalantar-Zadeh K. A practical approach to nutrition, protein-energy wasting, sarcopenia, and cachexia in patients with chronic kidney disease. Blood Purif. 2020; 49(1-2):202–211. PMID: 31851983.
Article3. Moon SJ, Kim TH, Yoon SY, Chung JH, Hwang HJ. Relationship between stage of chronic kidney disease and sarcopenia in Korean aged 40 years and older using the Korea National Health and Nutrition Examination Surveys (KNHANES IV-2, 3, and V-1, 2), 2008–2011. PLoS One. 2015; 10(6):e0130740. PMID: 26083479.
Article4. Goisser S, Kemmler W, Porzel S, Volkert D, Sieber CC, Bollheimer LC, et al. Sarcopenic obesity and complex interventions with nutrition and exercise in community-dwelling older persons--a narrative review. Clin Interv Aging. 2015; 10:1267–1282. PMID: 26346071.5. Fahal IH. Uraemic sarcopenia: aetiology and implications. Nephrol Dial Transplant. 2014; 29(9):1655–1665. PMID: 23625972.
Article6. Stenvinkel P, Larsson TE. Chronic kidney disease: a clinical model of premature aging. Am J Kidney Dis. 2013; 62(2):339–351. PMID: 23357108.
Article7. Anand S, Johansen KL, Kurella Tamura M. Aging and chronic kidney disease: the impact on physical function and cognition. J Gerontol A Biol Sci Med Sci. 2014; 69(3):315–322. PMID: 23913934.
Article8. Domański M, Ciechanowski K. Sarcopenia: a major challenge in elderly patients with end-stage renal disease. J Aging Res. 2012; 2012:754739. PMID: 22536505.
Article9. Foley RN, Wang C, Ishani A, Collins AJ, Murray AM. Kidney function and sarcopenia in the United States general population: NHANES III. Am J Nephrol. 2007; 27(3):279–286. PMID: 17440263.
Article10. Fried LF, Boudreau R, Lee JS, Chertow G, Kurella-Tamura M, Shlipak MG, et al. Kidney function as a predictor of loss of lean mass in older adults: health, aging and body composition study. J Am Geriatr Soc. 2007; 55(10):1578–1584. PMID: 17908060.
Article11. Workeneh BT, Mitch WE. Review of muscle wasting associated with chronic kidney disease. Am J Clin Nutr. 2010; 91(4):1128S–32S. PMID: 20181807.
Article12. Wang XH, Mitch WE. Muscle wasting from kidney failure-a model for catabolic conditions. Int J Biochem Cell Biol. 2013; 45(10):2230–2238. PMID: 23872437.
Article13. Stenvinkel P, Carrero JJ, von Walden F, Ikizler TA, Nader GA. Muscle wasting in end-stage renal disease promulgates premature death: established, emerging and potential novel treatment strategies. Nephrol Dial Transplant. 2016; 31(7):1070–1077. PMID: 25910496.
Article14. Jhamb M, Weisbord SD, Steel JL, Unruh M. Fatigue in patients receiving maintenance dialysis: a review of definitions, measures, and contributing factors. Am J Kidney Dis. 2008; 52(2):353–365. PMID: 18572290.
Article15. Lenk K, Schuler G, Adams V. Skeletal muscle wasting in cachexia and sarcopenia: molecular pathophysiology and impact of exercise training. J Cachexia Sarcopenia Muscle. 2010; 1(1):9–21. PMID: 21475693.
Article16. Koppe L, Fouque D, Kalantar-Zadeh K. Kidney cachexia or protein-energy wasting in chronic kidney disease: facts and numbers. J Cachexia Sarcopenia Muscle. 2019; 10(3):479–484. PMID: 30977979.
Article17. Clyne N. Physical working capacity in uremic patients. Scand J Urol Nephrol. 1996; 30(4):247–252. PMID: 8908642.
Article18. Obi Y, Qader H, Kovesdy CP, Kalantar-Zadeh K. Latest consensus and update on protein-energy wasting in chronic kidney disease. Curr Opin Clin Nutr Metab Care. 2015; 18(3):254–262. PMID: 25807354.
Article19. Rogan A, McCarthy K, McGregor G, Hamborg T, Evans G, Hewins S, et al. Quality of life measures predict cardiovascular health and physical performance in chronic renal failure patients. PLoS One. 2017; 12(9):e0183926. PMID: 28910330.
Article20. McGregor G, Ennis S, Powell R, Hamborg T, Raymond NT, Owen W, et al. Feasibility and effects of intra-dialytic low-frequency electrical muscle stimulation and cycle training: a pilot randomized controlled trial. PLoS One. 2018; 13(7):e0200354. PMID: 29995947.
Article21. Bohannon RW. Hand-grip dynamometry predicts future outcomes in aging adults. J Geriatr Phys Ther. 2008; 31(1):3–10. PMID: 18489802.
Article22. Norman K, Stobäus N, Gonzalez MC, Schulzke JD, Pirlich M. Hand grip strength: outcome predictor and marker of nutritional status. Clin Nutr. 2011; 30(2):135–142. PMID: 21035927.
Article23. Kittiskulnam P, Chertow GM, Carrero JJ, Delgado C, Kaysen GA, Johansen KL. Sarcopenia and its individual criteria are associated, in part, with mortality among patients on hemodialysis. Kidney Int. 2017; 92(1):238–247. PMID: 28318630.24. Vogt BP, Borges MC, Goés CR, Caramori JC. Handgrip strength is an independent predictor of all-cause mortality in maintenance dialysis patients. Clin Nutr. 2016; 35(6):1429–1433. PMID: 27083497.
Article25. Hwang SH, Lee DH, Min J, Jeon JY. Handgrip Strength as a Predictor of all-cause mortality in patients with chronic kidney disease undergoing dialysis: a meta-analysis of prospective cohort studies. J Ren Nutr. 2019; 29(6):471–479. PMID: 30827839.
Article26. Matsuzawa R, Kamitani T, Roshanravan B, Fukuma S, Joki N, Fukagawa M. Decline in the functional status and mortality in patients on hemodialysis: results from the Japan Dialysis Outcome and Practice Patterns Study. J Ren Nutr. 2019; 29(6):504–510. PMID: 30591357.
Article27. Yoo JI, Choi H, Ha YC. Mean hand grip strength and cut-off value for sarcopenia in Korean adults using KNHANES VI. J Korean Med Sci. 2017; 32(5):868–872. PMID: 28378563.
Article28. Hyun YY, Lee KB, Han SH, Kim YH, Kim YS, Lee SW, et al. Nutritional status in adults with predialysis chronic kidney disease: KNOW-CKD Study. J Korean Med Sci. 2017; 32(2):257–263. PMID: 28049236.
Article29. Carrero JJ, Stenvinkel P, Cuppari L, Ikizler TA, Kalantar-Zadeh K, Kaysen G, et al. Etiology of the protein-energy wasting syndrome in chronic kidney disease: a consensus statement from the International Society of Renal Nutrition and Metabolism (ISRNM). J Ren Nutr. 2013; 23(2):77–90. PMID: 23428357.
Article30. Kaizu Y, Ohkawa S, Odamaki M, Ikegaya N, Hibi I, Miyaji K, et al. Association between inflammatory mediators and muscle mass in long-term hemodialysis patients. Am J Kidney Dis. 2003; 42(2):295–302. PMID: 12900811.
Article31. Yamada S, Tokumoto M, Tatsumoto N, Taniguchi M, Noguchi H, Nakano T, et al. Phosphate overload directly induces systemic inflammation and malnutrition as well as vascular calcification in uremia. Am J Physiol Renal Physiol. 2014; 306(12):F1418–28. PMID: 24808541.
Article32. Kalantar-Zadeh K, Mehrotra R, Fouque D, Kopple JD. Metabolic acidosis and malnutrition-inflammation complex syndrome in chronic renal failure. Semin Dial. 2004; 17(6):455–465. PMID: 15660576.33. Kalantar-Zadeh K, Fouque D. Nutritional management of chronic kidney disease. N Engl J Med. 2017; 377(18):1765–1776. PMID: 29091561.
Article34. Bailey JL, Zheng B, Hu Z, Price SR, Mitch WE. Chronic kidney disease causes defects in signaling through the insulin receptor substrate/phosphatidylinositol 3-kinase/Akt pathway: implications for muscle atrophy. J Am Soc Nephrol. 2006; 17(5):1388–1394. PMID: 16611720.
Article35. de Brito-Ashurst I, Varagunam M, Raftery MJ, Yaqoob MM. Bicarbonate supplementation slows progression of CKD and improves nutritional status. J Am Soc Nephrol. 2009; 20(9):2075–2084. PMID: 19608703.
Article36. Kittiskulnam P, Srijaruneruang S, Chulakadabba A, Thokanit NS, Praditpornsilpa K, Tungsanga K, et al. Impact of serum bicarbonate levels on muscle mass and kidney function in pre-dialysis chronic kidney disease patients. Am J Nephrol. 2020; 51(1):24–34. PMID: 31752000.
Article37. Abramowitz MK, Melamed ML, Bauer C, Raff AC, Hostetter TH. Effects of oral sodium bicarbonate in patients with CKD. Clin J Am Soc Nephrol. 2013; 8(5):714–720. PMID: 23393105.
Article38. Toyoda K, Kuragano T, Kawada H, Taniguchi T, Nakanishi T. Effect of progression in malnutrition and inflammatory conditions on adverse events and mortality in patients on maintenance hemodialysis. Blood Purif. 2019; 47(Suppl 2):3–11. PMID: 30943483.
Article39. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Chapter 3: management of progression and complications of CKD. Kidney Int Suppl. 2013; 3(1):73–90.40. Bauer J, Biolo G, Cederholm T, Cesari M, Cruz-Jentoft AJ, Morley JE, et al. Evidence-based recommendations for optimal dietary protein intake in older people: a position paper from the PROT-AGE Study Group. J Am Med Dir Assoc. 2013; 14(8):542–559. PMID: 23867520.
Article41. Ziolkowski SL, Long J, Baker JF, Chertow GM, Leonard MB. Chronic kidney disease and the adiposity paradox: valid or confounded? J Ren Nutr. 2019; 29(6):521–528. PMID: 30709713.
Article42. Ku E, Kopple JD, Johansen KL, McCulloch CE, Go AS, Xie D, et al. Longitudinal weight change during CKD progression and its association with subsequent mortality. Am J Kidney Dis. 2018; 71(5):657–665. PMID: 29217305.
Article43. Patel SS, Molnar MZ, Tayek JA, Ix JH, Noori N, Benner D, et al. Serum creatinine as a marker of muscle mass in chronic kidney disease: results of a cross-sectional study and review of literature. J Cachexia Sarcopenia Muscle. 2013; 4(1):19–29. PMID: 22777757.
Article44. Canaud B, Granger Vallée A, Molinari N, Chenine L, Leray-Moragues H, Rodriguez A, et al. Creatinine index as a surrogate of lean body mass derived from urea Kt/V, pre-dialysis serum levels and anthropometric characteristics of haemodialysis patients. PLoS One. 2014; 9(3):e93286. PMID: 24671212.
Article45. Park J, Jin DC, Molnar MZ, Dukkipati R, Kim YL, Jing J, et al. Mortality predictability of body size and muscle mass surrogates in Asian vs white and African American hemodialysis patients. Mayo Clin Proc. 2013; 88(5):479–486. PMID: 23562348.
Article46. Moreau-Gaudry X, Jean G, Genet L, Lataillade D, Legrand E, Kuentz F, et al. A simple protein-energy wasting score predicts survival in maintenance hemodialysis patients. J Ren Nutr. 2014; 24(6):395–400. PMID: 25194620.
Article47. Cupisti A, D'Alessandro C, Fumagalli G, Vigo V, Meola M, Cianchi C, et al. Nutrition and physical activity in CKD patients. Kidney Blood Press Res. 2014; 39(2-3):107–113. PMID: 25117648.
Article48. Jung HW, Kim SW, Kim IY, Lim JY, Park HS, Song W, et al. Protein intake recommendation for Korean older adults to prevent sarcopenia: Expert consensus by the Korean Geriatric Society and the Korean Nutrition Society. Ann Geriatr Med Res. 2018; 22(4):167–175. PMID: 32743269.
Article49. Frey S, Mir AR, Lucas M. Visceral protein status and caloric intake in exercising versus nonexercising individuals with end-stage renal disease. J Ren Nutr. 1999; 9(2):71–77. PMID: 10089262.
Article50. Majchrzak KM, Pupim LB, Flakoll PJ, Ikizler TA. Resistance exercise augments the acute anabolic effects of intradialytic oral nutritional supplementation. Nephrol Dial Transplant. 2008; 23(4):1362–1369. PMID: 18065829.
Article51. Heiwe S, Jacobson SH. Exercise training in adults with CKD: a systematic review and meta-analysis. Am J Kidney Dis. 2014; 64(3):383–393. PMID: 24913219.
Article52. Johansen KL, Painter P. Exercise in individuals with CKD. Am J Kidney Dis. 2012; 59(1):126–134. PMID: 22113127.
Article53. Koh KP, Fassett RG, Sharman JE, Coombes JS, Williams AD. Effect of intradialytic versus home-based aerobic exercise training on physical function and vascular parameters in hemodialysis patients: a randomized pilot study. Am J Kidney Dis. 2010; 55(1):88–99. PMID: 19932545.
Article54. Ashor AW, Lara J, Siervo M, Celis-Morales C, Oggioni C, Jakovljevic DG, et al. Exercise modalities and endothelial function: a systematic review and dose-response meta-analysis of randomized controlled trials. Sports Med. 2015; 45(2):279–296. PMID: 25281334.
Article55. Kirkman DL, Mullins P, Junglee NA, Kumwenda M, Jibani MM, Macdonald JH. Anabolic exercise in haemodialysis patients: a randomised controlled pilot study. J Cachexia Sarcopenia Muscle. 2014; 5(3):199–207. PMID: 24710697.
Article56. Moraes C, Marinho SM, da Nobrega AC, de Oliveira Bessa B, Jacobson LV, Stockler-Pinto MB, et al. Resistance exercise: a strategy to attenuate inflammation and protein-energy wasting in hemodialysis patients? Int Urol Nephrol. 2014; 46(8):1655–1662. PMID: 24729104.
Article57. Salhab N, Karavetian M, Kooman J, Fiaccadori E, El Khoury CF. Effects of intradialytic aerobic exercise on hemodialysis patients: a systematic review and meta-analysis. J Nephrol. 2019; 32(4):549–566. PMID: 30659520.
Article58. Rhee SY, Song JK, Hong SC, Choi JW, Jeon HJ, Shin DH, et al. Intradialytic exercise improves physical function and reduces intradialytic hypotension and depression in hemodialysis patients. Korean J Intern Med. 2019; 34(3):588–598. PMID: 28838226.
Article59. Fotbolcu H, Duman D, Ecder SA, Oduncu V, Cevik C, Tigen K, et al. Attenuated cardiovascular response to sympathetic system activation during exercise in patients with dialysis-induced hypotension. Am J Nephrol. 2011; 33(6):491–498. PMID: 21546765.
Article60. Flythe JE, Xue H, Lynch KE, Curhan GC, Brunelli SM. Association of mortality risk with various definitions of intradialytic hypotension. J Am Soc Nephrol. 2015; 26(3):724–734. PMID: 25270068.
Article61. Kirkman DL, Edwards DG, Lennon-Edwards S. Exercise as an Adjunct therapy in chronic kidney disease. Renal Nutr Forum. 2014; 33(4):1–8. PMID: 26069463.62. Johansen KL, Chertow GM, Ng AV, Mulligan K, Carey S, Schoenfeld PY, et al. Physical activity levels in patients on hemodialysis and healthy sedentary controls. Kidney Int. 2000; 57(6):2564–2570. PMID: 10844626.
Article63. K/DOQI Workgroup. K/DOQI clinical practice guidelines for cardiovascular disease in dialysis patients. Am J Kidney Dis. 2005; 45(4):Suppl 3. S1–S153.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Cervicobrachial Disorders of Female International Telephone Operators III. Grip Strenghth
- Relationship Between Cigarette Smoking and Muscle Strength in Japanese Men
- Comparison of lower leg muscle strength and grip strength for diagnosing slower gait speed in the elderly
- Association between Muscle Strength and Anemia in the Rural Middle Age and Older Adults
- Association between Sleep Duration and Hand Grip Strength in Korean Elderly