Obstet Gynecol Sci.
2021 Mar;64(2):143-155. 10.5468/ogs.20264.
Social determinants of mental health of women living in slum: a systematic review
- Affiliations
-
- 1Social Determinants of Health Research Center, Alborz University of Medical Sciences, Karaj, Iran
- 2Student Research Committee, Nursing and Midwifery Faculty, Shahid Beheshti University of Medical Sciences, Tehran, Iran
- 3Department of Community Medicine, Faculty of Medicine, Tehran Medical Sciences, Islamic Azad University, Tehran, Iran
- 4Master Student of Clinical Psychology, Department of Psychology, Islamic Azad University, Tehran, Iran
- KMID: 2513945
- DOI: http://doi.org/10.5468/ogs.20264
Abstract
Objective
With the rise of urbanization globally, the problem of living in slums has become a problem for the civil society. As a vulnerable segment, women make up half of the population in these regions; therefore, women’s mental health has always been a concern. The purpose of this study was to review the social determinants of mental health in women living in slum areas.
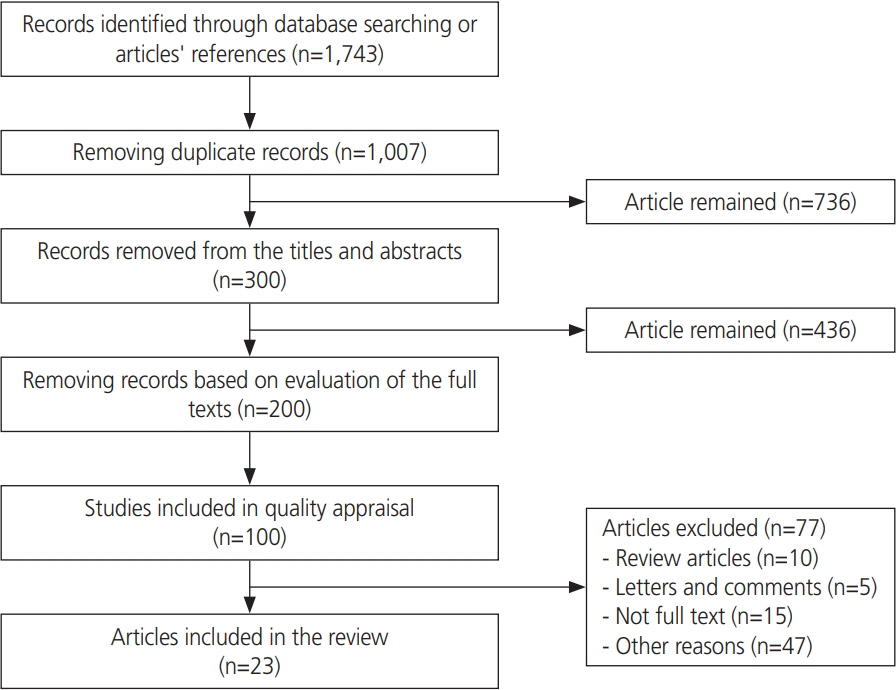
Methods
We systematically reviewed articles published between 2009 and 2019 on the social determinants of women’s mental health in SID, Magiran, Google scholar, PubMed, Scopus, Science Direct, Embase, MEDLINE, PsychINFO, and PsychARTICLES databases using MeSH keywords according to PRISMA guidelines. The quality of the studies was assessed depending on the type of study using Ottawa Newcastle” scale and Joanna Briggs Institute quality assessment tools. Finally, 23 studies were analyzed.
Results
Different social determinants influenced the mental health of women living in slum areas. Among the structural determinants, the socioeconomic level had the highest frequency, and gender was in the second rank with the highest correlation with poorer women’s mental health status. Among the intermediate determinants, living conditions, food insecurity, social capital, and social support were most frequently associated with mental health status.
Conclusion
Women living in slum areas are prone to developing mental disorders and poorer mental health; therefore, supporting these women and creating job opportunities to raise their incomes and, subsequently, improve their social, economic, and living conditions should be taken into consideration. In addition, this requires careful planning and comprehensive social support.
Figure
Reference
-
References
1. Begum S, Donta B, Nair S, Prakasam CP. Socio-demographic factors associated with domestic violence in urban slums, Mumbai, Maharashtra, India. Indian J Med Res. 2015; 141:783–8.
Article2. Lotfi H, Mirzaei M, Edalatkhah F, Vazirpour S. The crisis of slumminess in metropolises management and global approaches. J Hum Geogr. 2010; 2:135–45.3. Qishlaqi A, Moore F, Forghani G. Impact of untreated wastewater irrigation on soils and crops in Shiraz suburban area, SW Iran. Environ Monit Assess. 2008; 141:257–73.
Article4. Jamshidi A, Jamini D, Jamshidi M, Cheraghi R. Informal settlement, prioritizing current challenges case study: Jafar Abad District in Kermanshah City. Hum Geogr Res Q. 2014; 45:221–42.5. Riahi V, Gadermarzi H, Hamidi MS. Analysis of inequalities spatial in rural settlements Saqqez County. Geography. 2015; 13:47–72.6. Ruger JP. Health and social justice. Lancet. 2004; 364:1075–80.
Article7. Razzani B, Atashzadeh-Shoorideh F, Jamshidi T, Barkhordari-Sharifabad M, Lotfi Z, Skerrett V. The effect of education around ethical principles on nurses’ perception to patient safety culture in an Iranian mental health inpatient unit: a pilot study. BMC Nurs. 2020; 19:10.
Article8. Nazari H, Farhadi A, Jariayani M, Hosseinabadi R, Asgari S, Majidimehr M. Mental health of pregnant women referred to Khorramabad Health Centers. Yafteh. 2014; 16:40–8.9. Banaian SH, Parvin N, Kazemian A. The investigation of the relationship between mental health condition and marital satisfaction. J Hamadan Nurs Midwifery Fac. 2006; 14:52–8.10. Abdi F, Daryani NE, Khorvash F, Yousefi Z. Experiences of individuals with liver cirrhosis. Gastroenterol Nurs. 2015; 38:252–7.
Article11. Vahidi R, Kousha A, Kalantari H, Tabrizi J. Social determinants of health and their related organizations in East Azerbaijan. J Health. 2013; 3:20–8.12. Abdi F, Ozgoli G, Rahnemaie FS. A systematic review of the role of vitamin D and calcium in premenstrual syndrome. Obstet Gynecol Sci. 2019; 62:73–86.
Article13. Abdi F, Mobedi H, Bayat F, Mosaffa N, Dolatian M, Tehrani FR. The effects of transdermal estrogen delivery on bone mineral density in postmenopausal women: a meta-analysis. Iran J Pharm Res. 2017; 16:380–9.14. Rahnemaei FA, Fashami MA, Abdi F, Abbasi M. Factors effective in the prevention of preeclampsia: a systematic review. Taiwan J Obstet Gynecol. 2020; 59:173–82.15. World Health Organization. A conceptual framework for action on the social determinants of health. Geneva: World Health Organization;2010.16. Chauhan SK, Dhar M. Prevalence and predictors of mental health disorder among the adolescent living in the slums of Lucknow, India: a cross-sectional study. Community Ment Health J. 2020; 56:383–92.
Article17. Ashe S, Routray D. Prevalence, associated risk factors of depression and mental health needs among geriatric population of an urban slum, Cuttack, Odisha. Int J Geriatr Psychiatry. 2019; 34:1799–807.
Article18. Mathias K, Pandey A, Armstrong G, Diksha P, Kermode M. Outcomes of a brief mental health and resilience pilot intervention for young women in an urban slum in Dehradun, North India: a quasi-experimental study. Int J Ment Health Syst. 2018; 12:47.
Article19. Mutiso VN, Musyimi CW, Tomita A, Loeffen L, Burns JK, Ndetei DM. Epidemiological patterns of mental disorders and stigma in a community household survey in urban slum and rural settings in Kenya. Int J Soc Psychiatry. 2018; 64:120–9.
Article20. Rani D, Singh JK, Acharya D, Paudel R, Lee K, Singh SP. Household food insecurity and mental health among teenage girls living in urban slums in Varanasi, India: a cross-sectional study. Int J Environ Res Public Health. 2018; 15:1585.
Article21. Khan AM, Flora MS. Maternal common mental disorders and associated factors: a cross-sectional study in an urban slum area of Dhaka, Bangladesh. Int J Ment Health Syst. 2017; 11:23.
Article22. Khayat S, Dolatian M, Navidian A, Mahmoodi Z, Kasaeian A. Association between physical and sexual violence and mental health in suburban women of Zahedan: a cross-sectional study. J Clin Diagn Res. 2017; 11:IC01–5.
Article23. Panigrahi A, Panigrahi M, Padhy AP, Das SC. Common mental disorder and its socio-demographic correlates among married women residing in slum areas of Bhubaneswar, India. Women Health. 2017; 57:521–33.
Article24. Jacobs MB, Harville EW. Long-term mental health among low-income, minority women following exposure to multiple natural disasters in early and late adolescence compared to adulthood. Child Youth Care Forum. 2015; 44:511–25.
Article25. Khopkar SA, Virtanen SM, Kulathinal S. Mental health, anthropometry and blood pressure among adolescents living in slums of Nashik, India. Tanzan J Health Res. 2015; 17:6.26. Kiran MB, Srinivasan K, Niharika B, Priya S. A cross-sectional study of potential mental health problem in adult women living in urban slums of hyderabad. J Evol Med Dent Sci. 2015; 4:8561–9.27. Gupta S. Mental health and housing structure: a slum based study. Indian J Health Wellbeing. 2015; 6:734–6.28. Gilan NR, Ghasemi SR, Reshadat S, Zanganeh A, Saeidi S. Health-related quality of life of women in marginal areas of Kermanshah and some related factors. J Kermanshah Univ Med Sci. 2014; 18:e74023.29. Hiremath R, Debaje SP. Assessment of prevalence of domestic violence and mental health profile of adolescents exposed to domestic violence in an urban slum in Mumbai. Int J Res Med Sci. 2014; 2:290–2.
Article30. Subbaraman R, Nolan L, Shitole T, Sawant K, Shitole S, Sood K, et al. The psychological toll of slum living in Mumbai, India: a mixed methods study. Soc Sci Med. 2014; 119:155–69.
Article31. Haghighatian M, Jafari E. The relationship of bonding social capital with mental health among slum dwellers. Soc Welf. 2013; 13:129–47.32. Nahar JS, Haque M, Chowdhury NF, Qusar MS, Rahman W, Chowdhury HR, et al. Psychiatric morbidity among rural and slum female population: a comparative study. Bangabandhu Sheikh Mujib Med Univ J. 2013; 6:146–50.
Article33. Dasgupta A, Battala M, Saggurti N, Nair S, Naik DD, Silverman JG, et al. Local social support mitigates depression among women contending with spousal violence and husband’s risky drinking in Mumbai slum communities. J Affect Disord. 2013; 145:126–9.
Article34. Gruebner O, Khan MM, Lautenbach S, Müller D, Krämer A, Lakes T, et al. Mental health in the slums of Dhaka - a geoepidemiological study. BMC Public Health. 2012; 12:177.
Article35. Gruebner O, Khan MM, Lautenbach S, Müller D, Kraemer A, Lakes T, et al. A spatial epidemiological analysis of self-rated mental health in the slums of Dhaka. Int J Health Geogr. 2011; 10:36.
Article36. Rabbani R, Haghighatian M, Nazari J, Ghasemi M. A sociological study of marginalization and its impact on mental health of marginalized people (case study of Merzhan and Darak) Zeinabieh Isfahan. Shooshtar Soc Sci. 2011; 14:95.37. Elsey H, Manandah S, Sah D, Khanal S, MacGuire F, King R, et al. Public health risks in urban slums: findings of the qualitative ‘Healthy Kitchens Healthy Cities’ study in Kathmandu, Nepal. PLoS One. 2016; 11:e0163798.
Article38. Travasso SM, Rajaraman D, Heymann SJ. A qualitative study of factors affecting mental health amongst low-income working mothers in Bangalore, India. BMC Womens Health. 2014; 14:22.
Article39. Zare E, Roozbeh N, Akbari PA, Teshnizi SH, Ghazanfarpour M, Abdi F. HPV and its high-risk genotypes in Middle Eastern countries: a meta-analysis. Future Virol. 2020; 15:595–607.40. Weinberg D, Stevens GW, Duinhof EL, Finkenauer C. Adolescent Socioeconomic Status and Mental Health Inequalities in the Netherlands, 2001–2017. Int J Environ Res Public Health. 2019; 16:E3605.
Article41. Sweeney S, Air T, Zannettino L, Galletly C. Psychosis, socioeconomic disadvantage, and health service use in South Australia: findings from the second Australian National Survey of Psychosis. Front Public Health. 2015; 3:259.
Article42. Carter SE, Walker RL, Cutrona CE, Simons RL, Beach SR. Anxiety mediates perceived discrimination and health in African-American women. Am J Health Behav. 2016; 40:697–704.
Article43. Naghdi A, Zare S. The study of social and cultural factors affecting on women fertility living in slums. Sociol Women. 2013; 4:31–54.44. Nwameme AU, Phillips JF, Adongo PB. Compliance with emergency obstetric care referrals among pregnant women in an urban informal settlement of Accra, Ghana. Matern Child Health J. 2014; 18:1403–12.
Article45. Gitay MN, Fatima S, Arshad S, Arshad B, Ehtesham A, Baig MA, et al. Correction to: gender differences and prevalence of mental health problems in students of healthcare units. Community Ment Health J. 2019; 55:854.
Article46. Khayat S, Dolatian M, Navidian A, Kasaeian A, Mahmoodi Z. Association between style of living and general health in suburban women: a cross-sectional study in South East of Iran. J Clin Diagn Res. 2017; 11:LC09–13.47. Khayat S, Dolatian M, Navidian A, Kasaeian A, Mahmoodi Z. Association between style of living and general health in suburban women: a cross-sectional study in South East of Iran. J Clin Diagn Res. 2017; 11:LC09–13.48. Yadegari L, Dolatian M, Mahmoodi Z, Shahsavari S, Sharifi N. The relationship between socioeconomic factors and food security in pregnant women. Shiraz E Med J. 2017; 18:e41483.
Article49. Nieminen T, Martelin T, Koskinen S, Aro H, Alanen E, Hyyppä MT. Social capital as a determinant of self-rated health and psychological well-being. Int J Public Health. 2010; 55:531–42.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Most Important Social Determinants of Slum Dwellers’ Health: A Scoping Review
- Physician Utilization and its Determinants in Rural and Urban Slun Areas
- Contextual and Individual Determinants of Mental Health: A Cross-sectional Multilevel Study in Tehran, Iran
- Social Determinants of Health in Diabetes Patient Care
- Malnutrition Risk in Community-Dwelling Older Adults with Dual Sensory Declines: Focusing on Social Determinants of Health