Neonatal Med.
2021 Feb;28(1):53-58. 10.5385/nm.2021.28.1.53.
A Case of Midgut Volvulus with Gastric Perforation and Periveintricular Leukomalacia in a Term Infant
- Affiliations
-
- 1Department of Pediatrics, Inje University Ilsan Paik Hospital, Inje University College of Medicine, Goyang, Korea
- KMID: 2513360
- DOI: http://doi.org/10.5385/nm.2021.28.1.53
Abstract
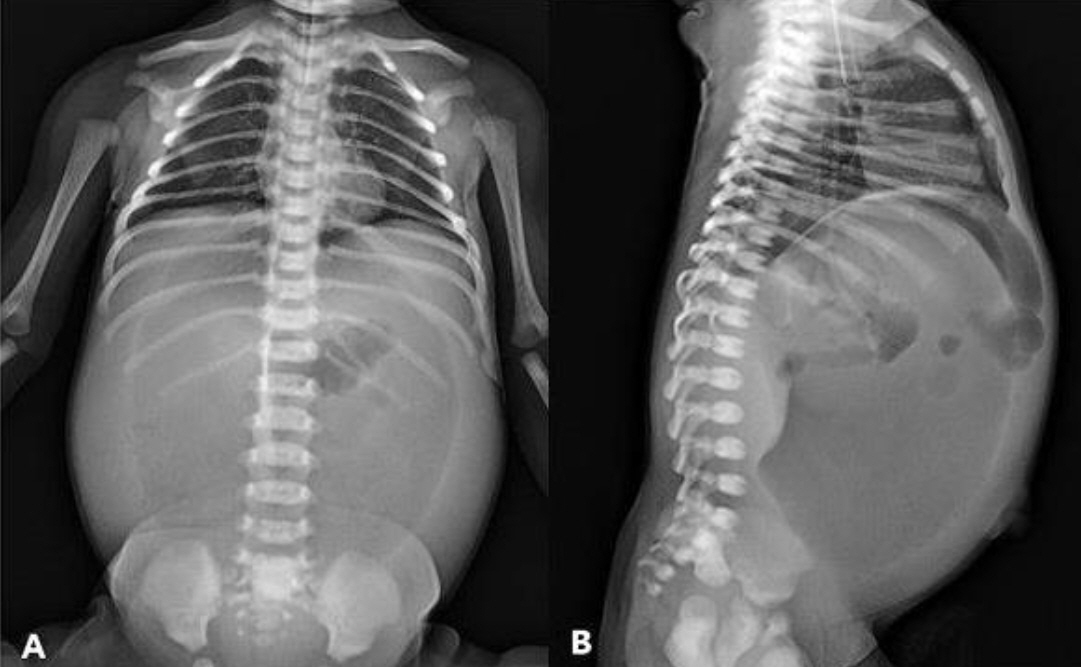
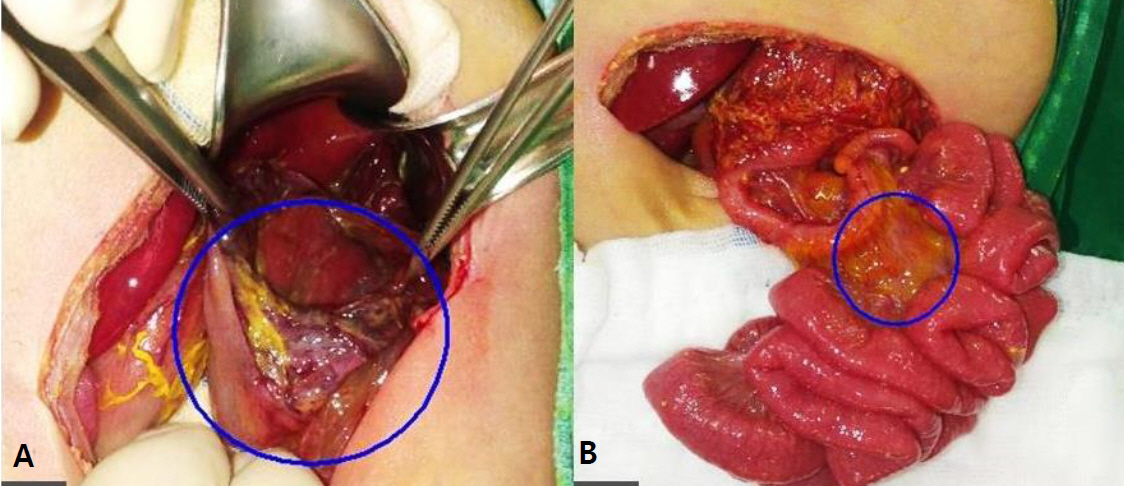
- Intestinal malrotation with midgut volvulus (MV) is a life-threatening surgical emergency. Most events of MV occur in the neonatal period with bilious vomiting, abdominal distension, feeding intolerance, and bloody stools. Neonatal gastric perforation (GP) is a rare and life-threatening condition associated with high mortality. It occurs either in an idiopathic form or in association with gastrointestinal anomalies such as duodenal atresia and MV. The pathogenesis of both MV and GP is related to ischemic change and inflammatory response. MV and GP can lead to morbidities such as sepsis, intestinal ischemia, and organ failure, but not neurologic problems. We herein report the case of a term infant at 5 days after birth, with MV accompanied by GP, who developed periventricular leukomalacia.
Figure
Reference
-
1. Lin JN, Lou CC, Wang KL. Intestinal malrotation and midgut volvulus: a 15-year review. J Formos Med Assoc. 1995; 94:178–81.2. Langer JC. Intestinal rotation abnormalities and midgut volvulus. Surg Clin North Am. 2017; 97:147–59.3. Linkner LM, Benson CD. Spontaneous perforation of the stomach in the newborn; analysis of thirteen cases. Ann Surg. 1959; 149:525–33.4. Nafatalewa DK, Misenga JB, Musapudi EM, Yebalaya PM, Mujinga DT, Ilunga GN. Spontaneous neonatal gastric perforation: about a case. Pan Afr Med J. 2018; 30:72.5. Kara CS, Ilce Z, Celayir S, Sarimurat N, Erdogan E, Yeker D. Neonatal gastric perforation: review of 23 years' experience. Surg Today. 2004; 34:243–5.6. Ohshiro K, Yamataka A, Kobayashi H, Hirai S, Miyahara K, Sueyoshi N, et al. Idiopathic gastric perforation in neonates and abnormal distribution of intestinal pacemaker cells. J Pediatr Surg. 2000; 35:673–6.7. Terui K, Iwai J, Yamada S, Takenouchi A, Nakata M, Komatsu S, et al. Etiology of neonatal gastric perforation: a review of 20 years' experience. Pediatr Surg Int. 2012; 28:9–14.8. Yang T, Huang Y, Li J, Zhong W, Tan T, Yu J, et al. Neonatal gastric perforation: case series and literature review. World J Surg. 2018; 42:2668–73.9. Amadeo JH, Ashmore HW, Aponte GE. Neonatal gastric perforation caused by congenital defects of the gastric musculature. Surgery. 1960; 47:1010–7.10. Tan CE, Kiely EM, Agrawal M, Brereton RJ, Spitz L. Neonatal gastrointestinal perforation. J Pediatr Surg. 1989; 24:888–92.11. Duran R, Inan M, Vatansever U, Aladag N, Acunas B. Etiology of neonatal gastric perforations: review of 10 years' experience. Pediatr Int. 2007; 49:626–30.12. Jawad AJ, Al-Rabie A, Hadi A, Al-Sowailem A, Al-Rawaf A, Abu-Touk B, et al. Spontaneous neonatal gastric perforation. Pediatr Surg Int. 2002; 18:396–9.13. Durham MM, Ricketts RR. Neonatal gastric perforation and necrosis with Hunt-Lawrence pouch reconstruction. J Pediatr Surg. 1999; 34:649–51.14. Herzog M, Cerar LK, Srsen TP, Verdenik I, Lucovnik M. Impact of risk factors other than prematurity on periventricular leukomalacia: a population-based matched case control study. Eur J Obstet Gynecol Reprod Biol. 2015; 187:57–9.15. Park HA, Hwang JH. The risk factors of periventricular leukomalacia among very low birth weight infants. Neonatal Med. 2020; 27:51–56.16. Jeican II, Ichim G, Gheban D. Intestinal ischemia in neonates and children. Clujul Med. 2016; 89:347–51.17. Chen Y, Chang KT, Lian DW, Lu H, Roy S, Laksmi NK, et al. The role of ischemia in necrotizing enterocolitis. J Pediatr Surg. 2016; 51:1255–61.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case of premature born with bowel perforation and gangrene due to intrauterine midgut volvulus caused by meconium ileus
- Sonographic Findings of Mesenteroaxial Gastric Volvulus in a Young Infant: A Case Report
- Midgut Volvulus of Infant Simulating Intussusception Diagnosis with Color Doppler Ultrasonography
- Intrauterine Midgut Volvulus with Malrotation in a Preterm Infant: A Case Report
- A Case of a Preterm Infant with Prenatally Diagnosed Intrauterine Midgut Volvulus