Arch Hand Microsurg.
2021 Mar;26(1):43-49. 10.12790/ahm.20.0046.
Subunit Principle: Key Element for Plantar Reconstruction with Free Sensate Flaps
- Affiliations
-
- 1Hospital Central Sur de Alta Especialidad De Petróleos Mexicanos, Mexico City, Mexico
- KMID: 2513205
- DOI: http://doi.org/10.12790/ahm.20.0046
Abstract
- Purpose
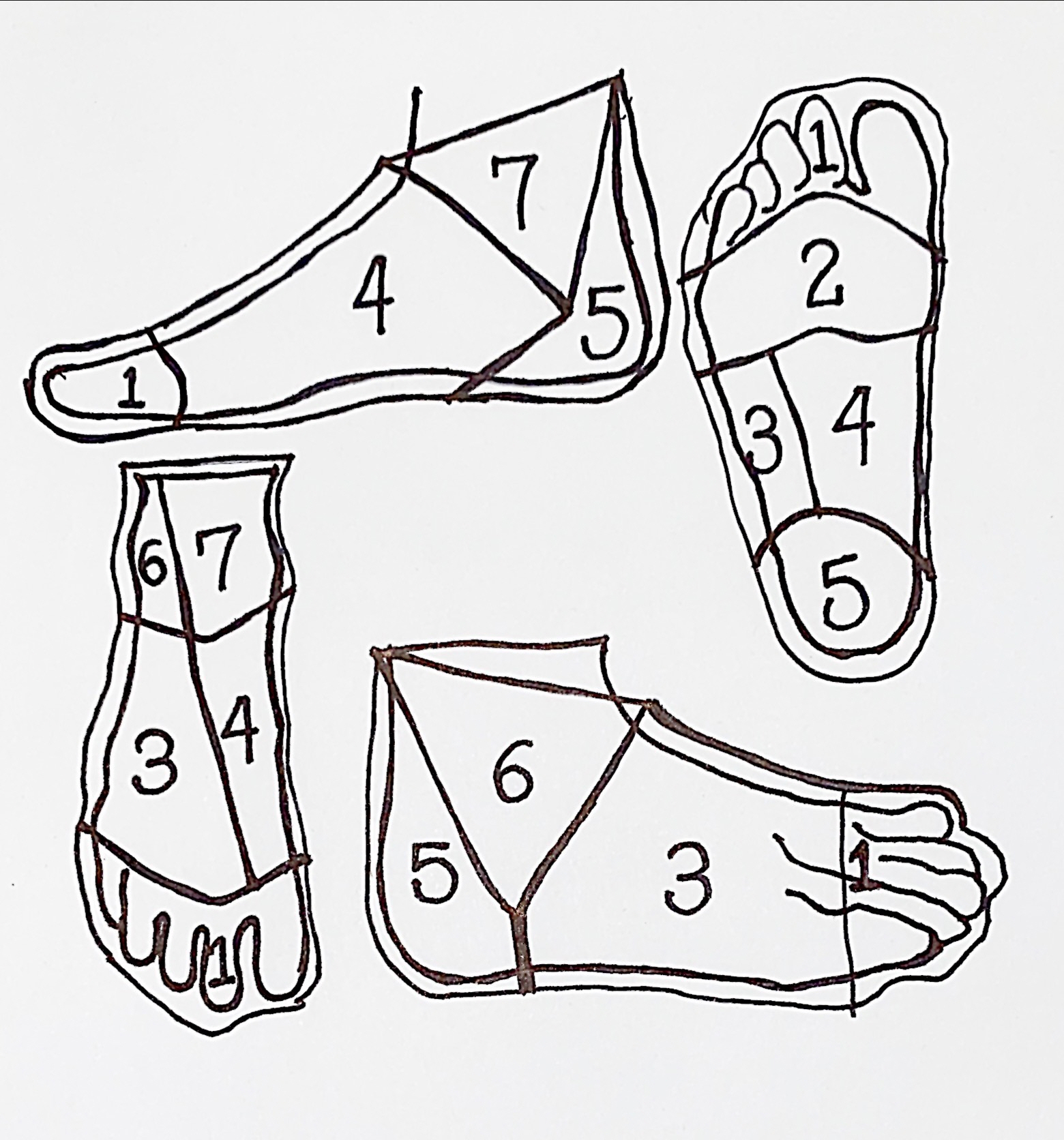
Plantar wounds represent a frequent practice of the plastic and reconstructive surgeon. The uniqueness and high complexity of the microarchitecture and biomechanics of the plantar region explain the complex challenge of its reconstruction. With the advances in microsurgery, including the plantar subunit principle, both applied in the restoration of plantar defects through the use of sensorineural free flaps have allowed an optimal reconstruction.
Methods
A descriptive, retrospective study was carried out in a period of time established between January 2016 and January 2019, obtaining a total of 18 patients with plantar defects, reconstructed using sensory free flaps. Tissue stability, recovery of protective sensitivity, early ambulation, and correct use of footwear were evaluated.
Results
The most frequent etiology was secondary to oncological resections due to melanoma (n = 12, 66.7%), followed by gunshot wounds (n = 4, 22.2%). Subunit 3 was the most frequently involved in 38.9% (n = 7). In the 88.8% of the cases, was used an anterolateral thigh flap (n = 16) and the lateral antebrachial flap in 22.2% (n = 2). The free flap survival rate was 100%. An average of seven points was obtained at 6 months based on the Semmes-Weinstein test. The mean for the return to their daily activities was 2.5 months. The patients of 94.4% (n = 17) recovered ambulation and could footwear.
Conclusion
The reconstruction of plantar defects must have a systematic approached, taking the subunit principle as a central point. The treatment of plantar defects with sensorineural free flaps represent an unprecedented option for optimal reconstruction.
Keyword
Figure
Cited by 1 articles
-
Comparison of fasciocutaneous and fascial anterolateral thigh free flaps in foot reconstruction
Si Young Roh, Chan Ju Park, Sung Hoon Koh, Jin Soo Kim, Dong Chul Lee, Kyung Jin Lee
Arch Hand Microsurg. 2023;28(2):97-105. doi: 10.12790/ahm.23.0004.
Reference
-
1. Soltanian H, Garcia RM, Hollenbeck ST. Current concepts in lower extremity reconstruction. Plast Reconstr Surg. 2015; 136:815e–829e.
Article2. Godina M. Early microsurgical reconstruction of complex trauma of the extremities. Plast Reconstr Surg. 1986; 78:285–92.
Article3. Hinchliffe RJ, Forsythe RO, Apelqvist J, et al. Guidelines on diagnosis, prognosis, and management of peripheral artery disease in patients with foot ulcers and diabetes (IWGDF 2019 update). Diabetes Metab Res Rev. 2020; 36 Suppl 1:e3276.
Article4. Scaglioni MF, Rittirsch D, Giovanoli P. Reconstruction of the heel, middle foot sole, and plantar forefoot with the medial plantar artery perforator flap: clinical experience with 28 cases. Plast Reconstr Surg. 2018; 141:200–8.5. Oh SJ, Moon M, Cha J, Koh SH, Chung CH. Weight-bearing plantar reconstruction using versatile medial plantar sensate flap. J Plast Reconstr Aesthet Surg. 2011; 64:248–54.
Article6. Hayashida K, Yamakawa S, Saijo H, Fujioka M. Foot reconstruction with the superficial circumflex iliac artery perforator flap under local anesthesia: two case reports. Medicine (Baltimore). 2019; 98:e13888.7. Suh HS, Oh TS, Hong JP. Innovations in diabetic foot reconstruction using supermicrosurgery. Diabetes Metab Res Rev. 2016; 32 Suppl 1:275–80.
Article8. Crowe CS, Cho DY, Kneib CJ, Morrison SD, Friedrich JB, Keys KA. Strategies for reconstruction of the plantar surface of the foot: a systematic review of the literature. Plast Reconstr Surg. 2019; 143:1223–44.9. Tamai S. History of microsurgery: from the beginning until the end of the 1970s. Microsurgery. 1993; 14:6–13.10. Tamai S. The history of microsurgery. Plast Reconstr Surg. 2009; 124(6 Suppl):e282–94.11. Hollenbeck ST, Woo S, Komatsu I, Erdmann D, Zenn MR, Levin LS. Longitudinal outcomes and application of the subunit principle to 165 foot and ankle free tissue transfers. Plast Reconstr Surg. 2010; 125:924–34.
Article12. Heidekrueger PI, Ehrl D, Prantl L, et al. Microsurgical reconstruction of the plantar foot: long-term functional outcomes and quality of life. J Reconstr Microsurg. 2019; 35:379–88.
Article13. D’Arpa S, Moschella F. Introduction to the current concepts in lower extremity reconstruction by the Italian Society for Microsurgery. J Reconstr Microsurg. 2017; 33(S 01):S01–2.
Article14. Löfstrand JG, Lin CH. Reconstruction of defects in the weight-bearing plantar area using the innervated free medial plantar (instep) flap. Ann Plast Surg. 2018; 80:245–51.
Article15. Hosseinian MA, Gharibi Loron A, Nemati Honar B. Reconstruction of the plantar toe with a distal reverse instep sensory island flap. Microsurgery. 2018; 38:667–73.
Article16. Lykoudis EG, Seretis K, Lykissas MG. Free sensate medial plantar flap for contralateral plantar forefoot reconstruction with flap reinnervation using end-to-side neurorrhaphy: a case report and literature review. Microsurgery. 2013; 33:227–31.
Article17. May JW Jr, Halls MJ, Simon SR. Free microvascular muscle flaps with skin graft reconstruction of extensive defects of the foot: a clinical and gait analysis study. Plast Reconstr Surg. 1985; 75:627–41.
Article18. Oliver-Allen H, Piper M, Vaughn C, Sbitany H. Immediate reconstruction for plantar melanoma: a paradigm shift. Ann Plast Surg. 2017; 78(5 Suppl 4):S194–8.19. Scaglioni MF, Franchi A, Uyulmaz S, Giovanoli P. The bipedicled medial plantar flap: vascular enhancement of a reverse flow Y-V medial plantar flap by the inclusion of a metatarsal artery perforator for the reconstruction of a forefoot defect: a case report. Microsurgery. 2018; 38:698–701.20. Eroğlu L, Güneren E, Keskin M, Uysal OA, Tomak Y. The extended V-Y flap for coverage of a mid-planatar defect. Br J Plast Surg. 2000; 53:708–10.21. Giraldo F, De Haro F, Ferrer A. Opposed transverse extended V-Y plantar flaps for reconstruction of neuropathic metatarsal head ulcers. Plast Reconstr Surg. 2001; 108:1019–24.
Article22. Gahalaut P, Pinto J, Pai GS, Kamath J, Joshua TV. A novel treatment for plantar ulcers in leprosy: local superficial flaps. Lepr Rev. 2005; 76:220–31.
Article23. Macedo JL, Rosa SC, Neto AV, Silva AA, Amorim AC. Reconstruction of soft-tissue lesions of the foot with the use of the medial plantar flap. Rev Bras Ortop. 2017; 52:699–704.
Article24. Wang CL, Shau YW, Hsu TC, Chen HC, Chien SH. Mechanical properties of heel pads reconstructed with flaps. J Bone Joint Surg Br. 1999; 81:207–11.
Article25. Cho EH, Shammas RL, Carney MJ, et al. Muscle versus fasciocutaneous free flaps in lower extremity traumatic reconstruction: a multicenter outcomes analysis. Plast Reconstr Surg. 2018; 141:191–9.26. Olivan MV, Busnardo FF, Faria JC, Coltro PS, Grillo VA, Gemperli R. Chimerical anterolateral thigh flap for plantar reconstruction. Microsurgery. 2015; 35:546–52.
Article27. Hong JP, Kim EK. Sole reconstruction using anterolateral thigh perforator free flaps. Plast Reconstr Surg. 2007; 119:186–93.
Article28. Sekido M, Yamamoto Y, Furukawa H, Sugihara T. Change of weight-bearing pattern before and after plantar reconstruction with free anterolateral thigh flap. Microsurgery. 2004; 24:289–92.
Article29. Chang NJ, Waughlock N, Kao D, Lin CH, Lin CH, Hsu CC. Efficient design of split anterolateral thigh flap in extremity reconstruction. Plast Reconstr Surg. 2011; 128:1242–9.
Article30. Yildirim S, Avci G, Aköz T. Soft-tissue reconstruction using a free anterolateral thigh flap: experience with 28 patients. Ann Plast Surg. 2003; 51:37–44.
Article31. Kadam D. Microsurgical reconstruction of plantar ulcers of the insensate foot. J Reconstr Microsurg. 2016; 32:402–10.
Article32. Zhu YL, Wang Y, He XQ, Zhu M, Li FB, Xu YQ. Foot and ankle reconstruction: an experience on the use of 14 different flaps in 226 cases. Microsurgery. 2013; 33:600–4.
Article33. Kuran I, Turgut G, Bas L, Ozkan T, Bayri O, Gulgonen A. Comparison between sensitive and nonsensitive free flaps in reconstruction of the heel and plantar area. Plast Reconstr Surg. 2000; 105:574–80.
Article34. Heymans O, Verhelle N, Lahaye T. Covering small defects on the weight bearing surfaces of the foot: the free temporal fasciocutaneous flap. Br J Plast Surg. 2005; 58:460–5.
Article35. Karşıdağ S, Akçal A, Turgut G, Uğurlu K, Baş L. Lower extremity soft tissue reconstruction with free flap based on subscapular artery. Acta Orthop Traumatol Turc. 2011; 45:100–8.
Article36. Emsen IM. Reconstruction with distally based dorsalis pedis fasciocutaneous flap for the coverage of distal toe-plantar defects. Can J Plast Surg. 2012; 20:e25–7.
Article37. Santanelli F, Tenna S, Pace A, Scuderi N. Free flap reconstruction of the sole of the foot with or without sensory nerve coaptation. Plast Reconstr Surg. 2002; 109:2314–24.
Article38. Sönmez A, Bayramiçli M, Sönmez B, Numanoğlu A. Reconstruction of the weight-bearing surface of the foot with nonneurosensory free flaps. Plast Reconstr Surg. 2003; 111:2230–6.39. Jeng SF, Wei FC. Classification and reconstructive options in foot plantar skin avulsion injuries. Plast Reconstr Surg. 1997; 99:1695–705.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Medial Plantar Island or Free Flap for Heel Reconstruction
- Reconstruction of Tissue Defects with Anterolateral Thigh Sensate Free Flap
- Sensate Medial Plantar Free Flap Transfer and Adductor Pollicis Myotomy for Treatment of Palmar Burn Scar Contracture
- Reconstruction of Plantar Forefoot in Diabetic Foot Ulcers: A Comparative Study of Perforator Flaps and Random Flaps
- Second Toe Plantar Free Flap for Volar Tissue Defects of the Fingers