Ann Hepatobiliary Pancreat Surg.
2021 Feb;25(1):160-166. 10.14701/ahbps.2021.25.1.160.
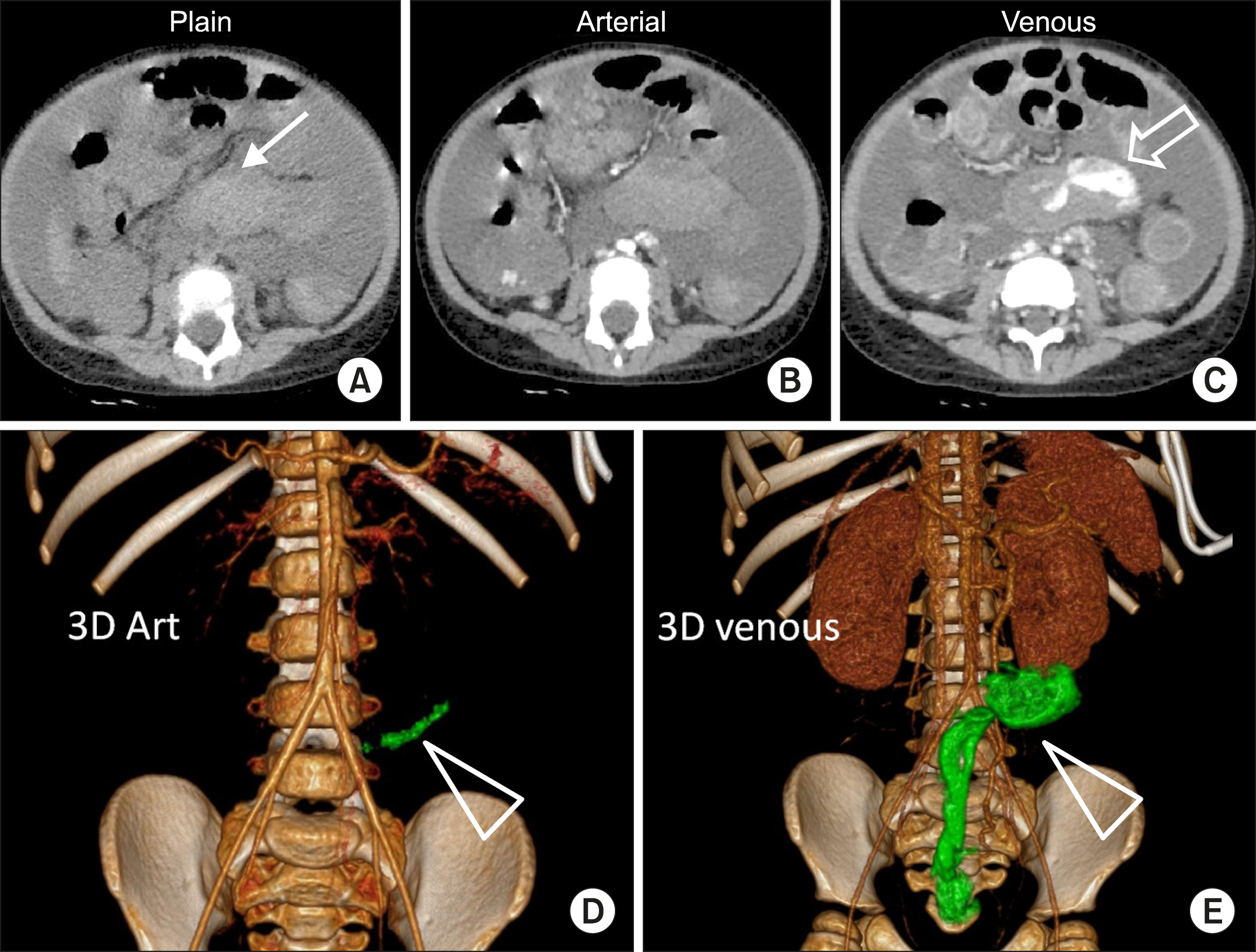
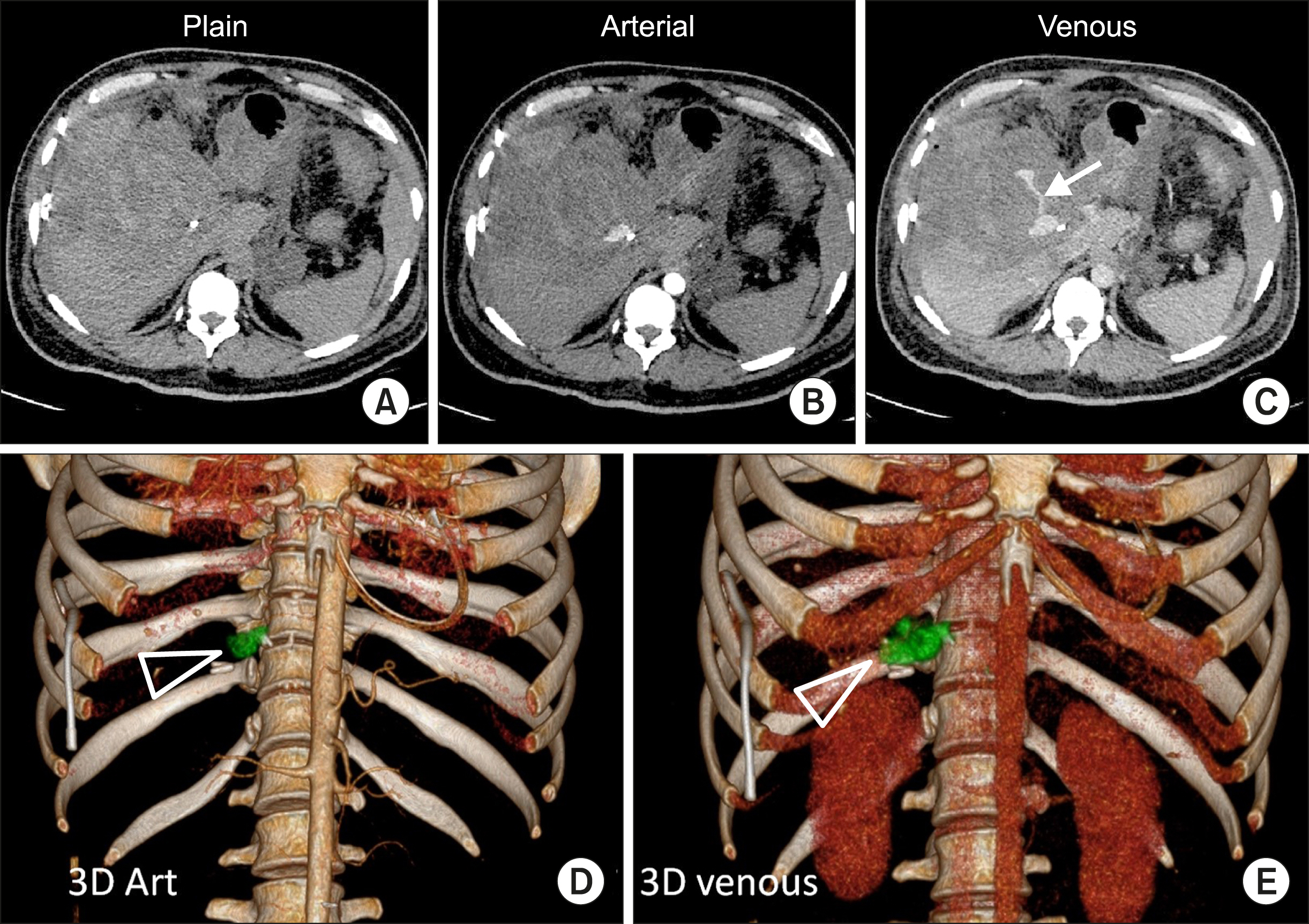
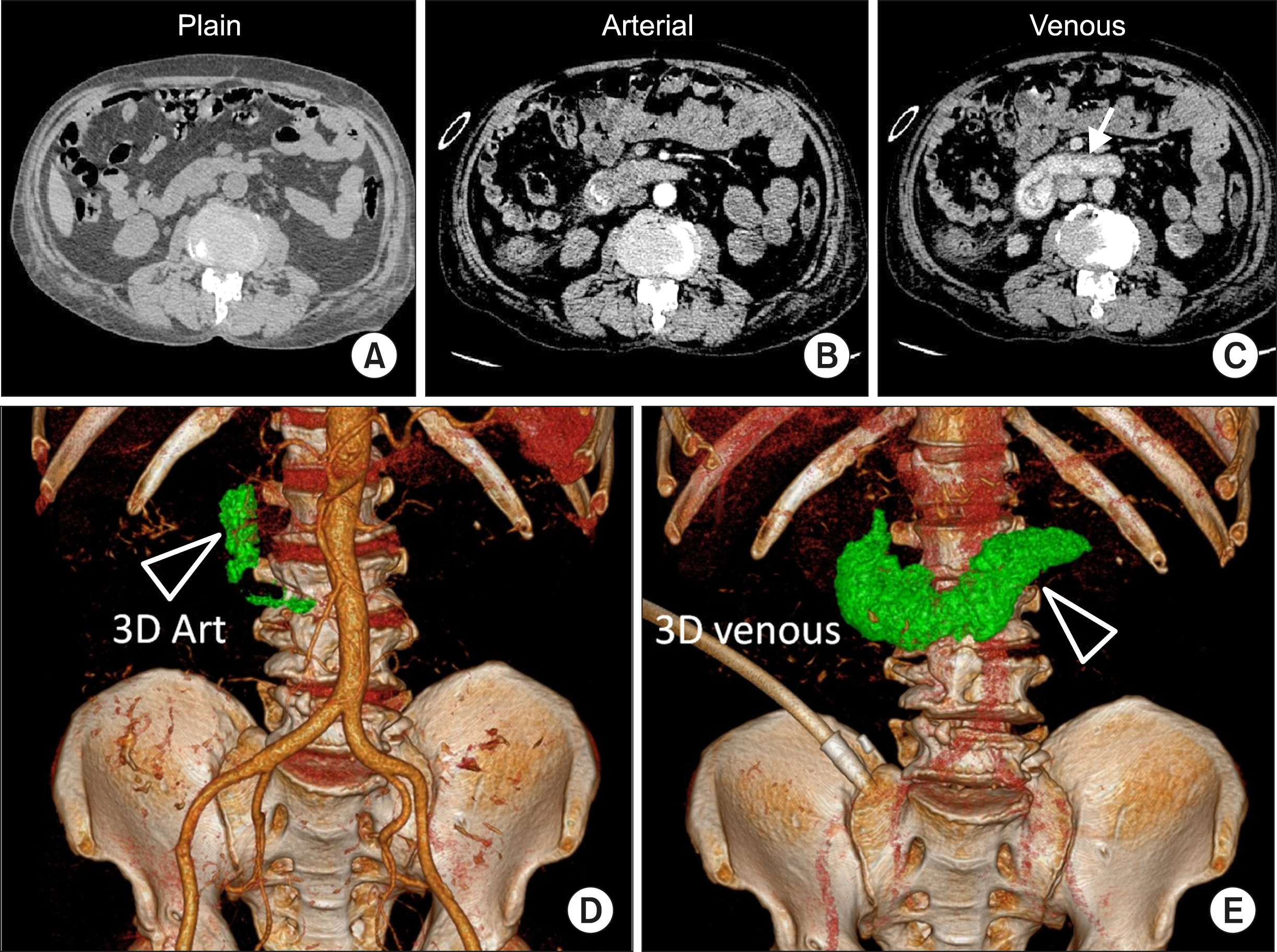
A novel concept on volumetric assessment and quantification of gastrointestinal bleed on computed tomography angiography: Observations based on a case series
- Affiliations
-
- 1Department of Radiology, Mazumdar Shaw Medical Centre - Narayana Multispecialty Hospital, Narayana Health, Bommasandra, Bengaluru, India
- KMID: 2513192
- DOI: http://doi.org/10.14701/ahbps.2021.25.1.160
Abstract
- Estimation of quantity and rate of bleeding is of great value in the management of patients with acute GI bleed. Endoscopy and multiphase contrast enhanced computed tomography (MCECT) are the presently employed two important methods for this purpose. Still there is a lacuna in the methods of precise estimation of amount of bleed, which at the moment are somewhat unreliable and subjectively evaluated. We present the value of dynamic contrast-enhanced CT examination in quantitatively estimating the amount of extravasated blood with the help of three illustrative clinical examples. Technique CT examination, the methodology for assessment of quantity of bleed is presented and the discussion of existing literature regarding the estimation methods is presented.
Keyword
Figure
Reference
-
1. Zhao Y, Encinosa W. 2008. Hospitalizations for gastrointestinal bleeding in 1998 and 2006: statistical brief #65. Agency for Healthcare Research and Quality (US);Rockville: Available from: http://www.ncbi.nlm.nih.gov/pubmed/21595135. cited 2008 Dec.2. Gunjan D, Sharma V, Rana SS, Bhasin DK. 2014; Small bowel bleeding: a comprehensive review. Gastroenterol Rep (Oxf). 2:262–275. DOI: 10.1093/gastro/gou025. PMID: 24874805. PMCID: PMC4219139.
Article3. Wu LM, Xu JR, Yin Y, Qu XH. 2010; Usefulness of CT angiography in diagnosing acute gastrointestinal bleeding: a meta-analysis. World J Gastroenterol. 16:3957–3963. DOI: 10.3748/wjg.v16.i31.3957. PMID: 20712058. PMCID: PMC2923771.
Article4. Wells ML, Hansel SL, Bruining DH, Fletcher JG, Froemming AT, Barlow JM, et al. 2018; CT for evaluation of acute gastrointestinal bleeding. Radiographics. 38:1089–1107. DOI: 10.1148/rg.2018170138. PMID: 29883267.
Article5. Ren JZ, Zhang MF, Rong AM, Fang XJ, Zhang K, Huang GH, et al. 2015; Lower gastrointestinal bleeding: role of 64-row computed tomographic angiography in diagnosis and therapeutic planning. World J Gastroenterol. 21:4030–4037. DOI: 10.3748/wjg.v21.i13.4030. PMID: 25852291. PMCID: PMC4385553.
Article6. Artigas JM, Martí M, Soto JA, Esteban H, Pinilla I, Guillén E. 2013; Multidetector CT angiography for acute gastrointestinal bleeding: technique and findings. Radiographics. 33:1453–1470. DOI: 10.1148/rg.335125072. PMID: 24025935.
Article7. Kleinman JT, Hillis AE, Jordan LC. 2011; ABC/2: estimating intracerebral haemorrhage volume and total brain volume, and predicting outcome in children. Dev Med Child Neurol. 53:281–284. DOI: 10.1111/j.1469-8749.2010.03798.x. PMID: 20875043. PMCID: PMC3026070.
Article8. Chikamatsu Y, Matsuda K, Takeuchi Y, Kagaya S, Ojima Y, Fukami H, et al. 2017; Quantification of bleeding volume using computed tomography and clinical complications after percutaneous renal biopsy. Clin Kidney J. 10:9–15. DOI: 10.1093/ckj/sfw131. PMID: 28638600. PMCID: PMC5469571.
Article9. Monteiro S, Gonçalves TC, Magalhães J, Cotter J. 2016; Upper gastrointestinal bleeding risk scores: who, when and why? World J Gastrointest Pathophysiol. 7:86–96. DOI: 10.4291/wjgp.v7.i1.86. PMID: 26909231. PMCID: PMC4753192.
Article10. Stanley AJ. 2012; Update on risk scoring systems for patients with upper gastrointestinal haemorrhage. World J Gastroenterol. 18:2739–2744. DOI: 10.3748/wjg.v18.i22.2739. PMID: 22719181. PMCID: PMC3374976.
Article11. Cañamares P, Alfaro E, Lanas A. 2017; Safe hospital discharge based on lower GI bleeding scores: a long way to go. AME Med J. 2:147. DOI: 10.21037/amj.2017.09.08.
Article12. Yoon W, Jeong YY, Kim JK. 2006; Acute gastrointestinal bleeding: contrast-enhanced MDCT. Abdom Imaging. 31:1–8. DOI: 10.1007/s00261-005-0367-8. PMID: 16333701.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Evaluation of Myocardial Ischemia Using Coronary Computed Tomography Angiography in Patients with Stable Angina
- Provocative mesenteric angiography for diagnosis and treatment of occult gastrointestinal hemorrhage
- A preliminary quantification of Tc-HMPAO brain SPECT images for assessment of volumetric regional cerebral blood flow
- Role of computed tomography angiography for acute gastrointestinal bleeding
- Recent Progress in Abdominal CT Imaging