Clin Exp Otorhinolaryngol.
2021 Feb;14(1):93-99. 10.21053/ceo.2019.01921.
Cluster Analysis of Inhalant Allergens in South Korea: A Computational Model of Allergic Sensitization
- Affiliations
-
- 1Department of Otorhinolaryngology-Head and Neck Surgery, Chuncheon Sacred Heart Hospital, Hallym University College of Medicine, Chuncheon, Korea
- 2Department of Mathematics and Institute of Natural Sciences, Hanyang University College of Natural Sciences, Seoul, Korea
- 3Department of Occupational and Environmental Medicine, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea
- 4Department of Otorhinolaryngology-Head and Neck Surgery, Hanyang University College of Medicine, Seoul, Korea
- 5Department of Internal Medicine, Hanyang University College of Medicine, Seoul, Korea
- KMID: 2512887
- DOI: http://doi.org/10.21053/ceo.2019.01921
Abstract
Objectives
. Sensitization to specific inhalant allergens is a major risk factor for the development of atopic diseases, which impose a major socioeconomic burden and significantly diminish quality of life. However, patterns of inhalant allergic sensitization have yet to be precisely described. Therefore, to enhance the understanding of aeroallergens, we performed a cluster analysis of inhalant allergic sensitization using a computational model.
Methods
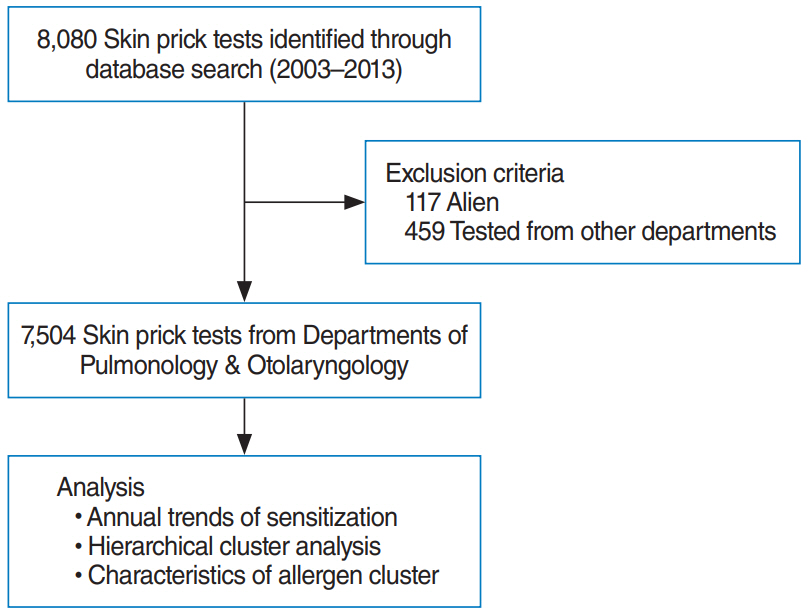
. Skin prick data were collected from 7,504 individuals. A positive skin prick response was defined as an allergen-to-histamine wheal ratio ≥1. To identify the clustering of inhalant allergic sensitization, we performed computational analysis using the four-parameter unified-Richards model.
Results
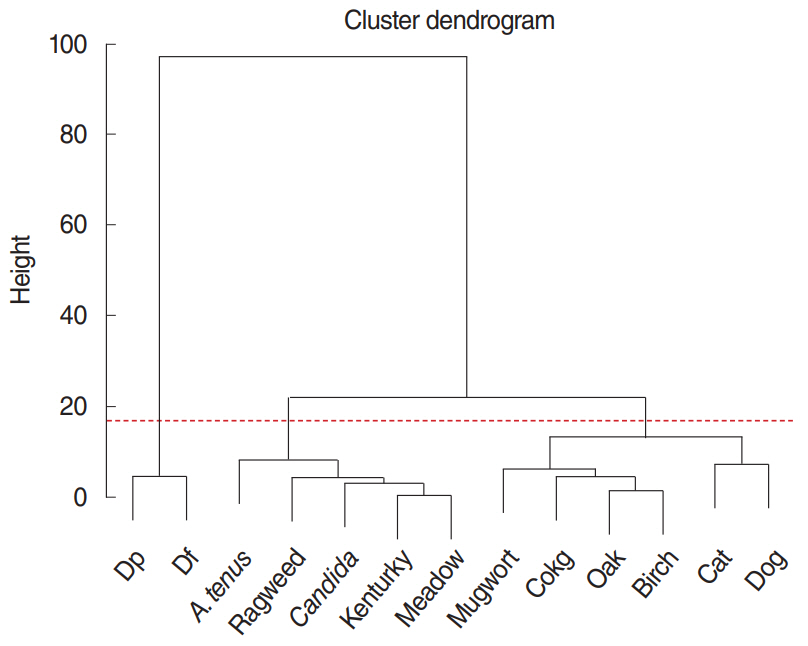
. Hierarchical cluster analysis grouped inhalant allergens into three clusters based on the Davies-Bouldin index (0.528): cluster 1 (Dermatophagoides pteronyssinus and Dermatophagoides farinae), cluster 2 (mugwort, cockroach, oak, birch, cat, and dog), and cluster 3 (Alternaria tenus, ragweed, Candida albicans, Kentucky grass, and meadow grass). Computational modeling revealed that each allergen cluster had a different trajectory over the lifespan. Cluster 1 showed a high level (>50%) of sensitization at an early age (before 19 years), followed by a sharp decrease in sensitization. Cluster 2 showed a moderate level (10%–20%) of sensitization before 29 years of age, followed by a steady decrease in sensitization. However, cluster 3 revealed a low level (<10%) of sensitization at all ages.
Conclusion
. Computational modeling suggests that allergic sensitization consists of three clusters with distinct patterns at different ages. The results of this study will be helpful to allergists in managing patients with atopic diseases.
Keyword
Figure
Cited by 1 articles
-
Understanding the Patterns and Clustering of Inhalant Allergic Sensitization
Shin Hyuk Yoo, Ji-Hun Mo
Clin Exp Otorhinolaryngol. 2021;14(1):11-12. doi: 10.21053/ceo.2021.00073.
Reference
-
1. Park HJ, Lim HS, Park KH, Lee JH, Park JW, Hong CS. Changes in allergen sensitization over the last 30 years in Korea respiratory allergic patients: a single-center. Allergy Asthma Immunol Res. 2014; Sep. 6(5):434–43.
Article2. Kang MG, Kim MY, Song WJ, Kim S, Jo EJ, Lee SE, et al. Patterns of inhalant allergen sensitization and geographical variation in Korean adults: a multicenter retrospective study. Allergy Asthma Immunol Res. 2017; Nov. 9(6):499–508.
Article3. Shin JH, Lee DH. How does the pattern of aeroallergen sensitization change over time across all ages? Int Forum Allergy Rhinol. 2017; Jul. 7(7):652–9.
Article4. Yong SB, Wu CC, Tzeng YC, Hung WC, Yang KD. Different profiles of allergen sensitization in different ages and geographic areas in Changhua, Taiwan. J Microbiol Immunol Infect. 2013; Aug. 46(4):295–301.
Article5. Mehulic M, Mehulic K, Vuljanko IM, Kukulj S, Grle SP, Vukic AD, et al. Changing pattern of sensitization in Croatia to aeroallergens in adult population referring to allergy clinic during a period of 15 years. Coll Antropol. 2011; Jun. 35(2):529–36.6. Veskitkul J, Vichyanond P, Visitsunthorn N, Jirapongsananuruk O. The development of allergic rhinitis in children previously diagnosed as nonallergic rhinitis. Am J Rhinol Allergy. 2013; Jan. 27(1):43–7.
Article7. Linneberg A, Nielsen NH, Madsen F, Frolund L, Dirksen A, Jorgensen T. Increasing prevalence of specific IgE to aeroallergens in an adult population: two cross-sectional surveys 8 years apart: the Copenhagen Allergy Study. J Allergy Clin Immunol. 2000; Aug. 106(2):247–52.8. Demain JG. Climate change and the impact on respiratory and allergic disease: 2018. Curr Allergy Asthma Rep. 2018; Mar. 18(4):22.
Article9. D’Amato G, Bergmann KC, Cecchi L, Annesi-Maesano I, Sanduzzi A, Liccardi G, et al. Climate change and air pollution: effects on pollen allergy and other allergic respiratory diseases. Allergo J Int. 2014; 23(1):17–23.10. D’Amato G, Vitale C, Lanza M, Molino A, D’Amato M. Climate change, air pollution, and allergic respiratory diseases: an update. Curr Opin Allergy Clin Immunol. 2016; Oct. 16(5):434–40.
Article11. Jerrett M, Burnett RT, Pope CA 3rd, Ito K, Thurston G, Krewski D, et al. Long-term ozone exposure and mortality. N Engl J Med. 2009; Mar. 360(11):1085–95.
Article12. McGeachie MJ, Yates KP, Zhou X, Guo F, Sternberg AL, van Natta ML, et al. Patterns of growth and decline in lung function in persistent childhood asthma. N Engl J Med. 2016; May. 374(19):1842–52.
Article13. McConnell R, Berhane K, Yao L, Jerrett M, Lurmann F, Gilliland F, et al. Traffic, susceptibility, and childhood asthma. Environ Health Perspect. 2006; May. 114(5):766–72.
Article14. Jerrett M, Finkelstein MM, Brook JR, Arain MA, Kanaroglou P, Stieb DM, et al. A cohort study of traffic-related air pollution and mortality in Toronto, Ontario, Canada. Environ Health Perspect. 2009; May. 117(5):772–7.
Article15. Burbach GJ, Heinzerling LM, Edenharter G, Bachert C, Bindslev-Jensen C, Bonini S, et al. GA(2)LEN skin test study II: clinical relevance of inhalant allergen sensitizations in Europe. Allergy. 2009; Oct. 64(10):1507–15.16. Schmitz R, Ellert U, Kalcklosch M, Dahm S, Thamm M. Patterns of sensitization to inhalant and food allergens: findings from the German Health Interview and Examination Survey for Children and Adolescents. Int Arch Allergy Immunol. 2013; 162(3):263–70.17. Salo PM, Arbes SJ Jr, Jaramillo R, Calatroni A, Weir CH, Sever ML, et al. Prevalence of allergic sensitization in the United States: results from the National Health and Nutrition Examination Survey (NHANES) 2005-2006. J Allergy Clin Immunol. 2014; Aug. 134(2):350–9.
Article18. Voloshin S, Smoldovskaya O, Feyzkhanova G, Arefieva A, Pavlushkina L, Filatova T, et al. Patterns of sensitization to inhalant and food allergens among pediatric patients from the Moscow region (Russian Federation). PLoS One. 2018; Mar. 13(3):e0194775.
Article19. Tjorve KMC, Tjorve E. The use of Gompertz models in growth analyses, and new Gompertz-model approach: an addition to the Unified-Richards family. PLoS One. 2017; Jun. 12(6):e0178691.
Article20. Tjorve E, Tjorve KM. A unified approach to the Richards-model family for use in growth analyses: why we need only two model forms. J Theor Biol. 2010; Dec. 267(3):417–25.21. Walker S, Khan-Wasti S, Fletcher M, Cullinan P, Harris J, Sheikh A. Seasonal allergic rhinitis is associated with a detrimental effect on examination performance in United Kingdom teenagers: case-control study. J Allergy Clin Immunol. 2007; Aug. 120(2):381–7.
Article22. Lee DJ, Chung YJ, Yang YJ, Mo JH. The impact of allergic rhinitis on symptom improvement in pediatric patients after adenotonsillectomy. Clin Exp Otorhinolaryngol. 2018; Mar. 11(1):52–7.
Article23. Kim MJ, Bae SH, Lee SM, Lee KH, Kim DK. Effect of adenotonsillectomy on attention in Korean children with sleep-disordered breathing. Clin Exp Otorhinolaryngol. 2018; Sep. 11(3):199–204.
Article24. Zar HJ, Ehrlich RI, Workman L, Weinberg EG. The changing prevalence of asthma, allergic rhinitis and atopic eczema in African adolescents from 1995 to 2002. Pediatr Allergy Immunol. 2007; Nov. 18(7):560–5.
Article25. Maziak W, Behrens T, Brasky TM, Duhme H, Rzehak P, Weiland SK, et al. Are asthma and allergies in children and adolescents increasing? Results from ISAAC phase I and phase III surveys in Munster, Germany. Allergy. 2003; Jul. 58(7):572–9.
Article26. Lee SL, Wong W, Lau YL. Increasing prevalence of allergic rhinitis but not asthma among children in Hong Kong from 1995 to 2001 (Phase 3 International Study of Asthma and Allergies in Childhood). Pediatr Allergy Immunol. 2004; Feb. 15(1):72–8.
Article27. Pearce N, Ait-Khaled N, Beasley R, Mallol J, Keil U, Mitchell E, et al. Worldwide trends in the prevalence of asthma symptoms: phase III of the International Study of Asthma and Allergies in Childhood (ISAAC). Thorax. 2007; Sep. 62(9):758–66.
Article28. Bjorksten B, Clayton T, Ellwood P, Stewart A, Strachan D; ISAAC Phase III Study Group. Worldwide time trends for symptoms of rhinitis and conjunctivitis: phase III of the International Study of Asthma and Allergies in Childhood. Pediatr Allergy Immunol. 2008; Mar. 19(2):110–24.
Article29. Asher MI, Montefort S, Bjorksten B, Lai CK, Strachan DP, Weiland SK, et al. Worldwide time trends in the prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and eczema in childhood: ISAAC phases one and three repeat multicountry cross-sectional surveys. Lancet. 2006; Aug. 368(9537):733–43.
Article30. Kim SY, Jung JY, Park MS, Kang YA, Kim EY, Kim SK, et al. Increased prevalence of self-reported asthma among Korean adults: an analysis of KNHANES I and IV data. Lung. 2013; Jun. 191(3):281–8.
Article31. Yoo B, Park Y, Park K, Kim H. A 9-year trend in the prevalence of allergic disease based on national health insurance data. J Prev Med Public Health. 2015; Nov. 48(6):301–9.
Article32. Kim J, Hahm MI, Lee SY, Kim WK, Chae Y, Park YM, et al. Sensitization to aeroallergens in Korean children: a population-based study in 2010. J Korean Med Sci. 2011; Sep. 26(9):1165–72.
Article33. Luoma R, Koivikko A, Viander M. Development of asthma, allergic rhinitis and atopic dermatitis by the age of five years: a prospective study of 543 newborns. Allergy. 1983; Jul. 38(5):339–46.
Article34. Olsson P, Berglind N, Bellander T, Stjarne P. Prevalence of self-reported allergic and non-allergic rhinitis symptoms in Stockholm: relation to age, gender, olfactory sense and smoking. Acta Otolaryngol. 2003; Jan. 123(1):75–80.
Article35. Shen CY, Lin MC, Lin HK, Lin CH, Fu LS, Fu YC. The natural course of eczema from birth to age 7 years and the association with asthma and allergic rhinitis: a population-based birth cohort study. Allergy Asthma Proc. 2013; Jan-Feb. 34(1):78–83.
Article36. Cazzoletti L, Ferrari M, Olivieri M, Verlato G, Antonicelli L, Bono R, et al. The gender, age and risk factor distribution differs in self-reported allergic and non-allergic rhinitis: a cross-sectional population-based study. Allergy Asthma Clin Immunol. 2015; Dec. 11:36.
Article37. Yu HT, Shin EC. T cell immunosenescence, hypertension, and arterial stiffness. Epidemiol Health. 2014; May. 36:e2014005.
Article38. Maue AC, Yager EJ, Swain SL, Woodland DL, Blackman MA, Haynes L. T-cell immunosenescence: lessons learned from mouse models of aging. Trends Immunol. 2009; Jul. 30(7):301–5.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Change of Inhalant Allergen Sensitization in Children with Allergic Respiratory Diseases during Recent 10 Years
- Sensitization to Inhalant Allergens and Its Association with Allergic Diseases in Preschool Children
- Blood eosinophil counts as a biomarker for allergen sensitization in childhood allergic diseases in comparison with total IgE
- A comparison of Sensitization to Major Indoor & Outdoor Inhalant Allergens in Children with Respiratory Allergic Diseases
- Classification and Epidemiology of Allergic Rhinitis