Ann Surg Treat Res.
2021 Feb;100(2):67-75. 10.4174/astr.2021.100.2.67.
Comparing the short-term outcomes and cost between solo single-incision distal gastrectomy and conventional multiport totally laparoscopic distal gastrectomy for early gastric cancer: a propensity score-matched analysis
- Affiliations
-
- 1Department of Surgery, Seoul National University Bundang Hospital, Seongnam, Korea
- 2Department of Surgery, Ewha Womans University Hospital, Seoul, Korea
- 3Department of Surgery, Seoul National University College of Medicine, Seoul, Korea
- 4Department of Surgery, Seoul National University Hospital, Seoul, Korea
- KMID: 2512478
- DOI: http://doi.org/10.4174/astr.2021.100.2.67
Abstract
- Purpose
Single-incision laparoscopic distal gastrectomy (SIDG) requires experienced camera operators for a stable image. Since it is difficult for skilled camera operators to participate in all SIDG, we began performing solo surgery using mechanical camera holders. We aimed to compare the short-term outcomes and cost between solo SIDG and conventional multiport laparoscopic distal gastrectomy (MLDG) for early gastric cancer (EGC).
Methods
From January 2014 to December 2016, a total of 938 consecutive patients underwent laparoscopic gastrectomy for EGC. Solo SIDG (n = 99) and MLDG patients (n = 198) were selected and 1:2 propensity score matching was done to compare the quality of operation and cost-effectiveness. All solo SIDG was performed by a surgeon using a camera holder, without any assistant.
Results
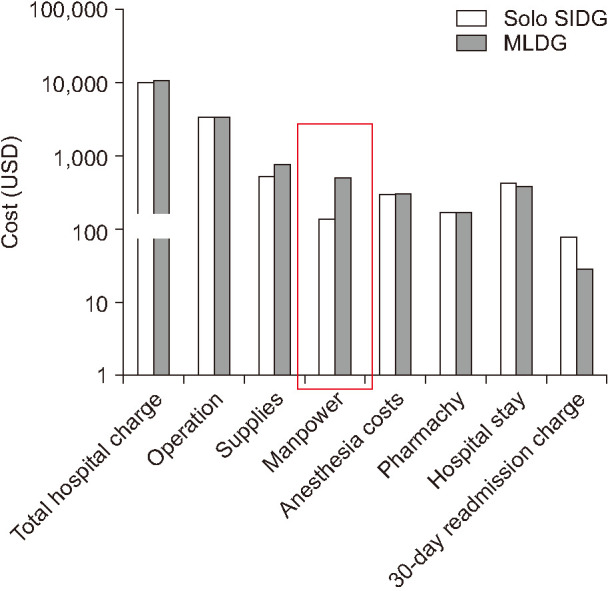
Mean operation time (120 ± 35.3 vs. 178 ± 53.4 minutes, P = 0.001) and estimated blood loss (24.6 ± 47.4 vs. 46.7 ± 66.5 mL, P = 0.001) were significantly lower in the solo SIDG group. Hospital stay, use of analgesics, and postoperative inflammatory markers (WBC, CRP) were similar between the 2 groups. The early (<30 days) complication rate in solo SIDG and MLDG groups was 21.2% and 23.7%, respectively (P = 0.240); the late (≥30 days) complication rate was 7.1% and 11.1%, respectively (P = 0.672). The manpower cost of solo SIDG was significantly lower than that of MLDG (P = 0.001).
Conclusion
This study demonstrated that solo SIDG performed by experienced laparoscopic surgeons is safe and feasible for EGC. Solo SIDG is expected to be a promising potential treatment for EGC.
Keyword
Figure
Reference
-
1. Omori T, Tanaka K, Tori M, Ueshima S, Akamatsu H, Nishida T. Intracorporeal circular-stapled Billroth I anastomosis in single-incision laparoscopic distal gastrectomy. Surg Endosc. 2012; 26:1490–1494. PMID: 22044985.
Article2. Ahn SH, Son SY, Jung DH, Park DJ, Kim HH. Pure single-port laparoscopic distal gastrectomy for early gastric cancer: comparative study with multi-port laparoscopic distal gastrectomy. J Am Coll Surg. 2014; 219:933–943. PMID: 25256369.
Article3. Omori T, Fujiwara Y, Moon J, Sugimura K, Miyata H, Masuzawa T, et al. Comparison of single-incision and conventional multiport laparoscopic distal gastrectomy with D2 lymph node dissection for gastric cancer: a propensity score-matched analysis. Ann Surg Oncol. 2016; 23(Suppl 5):817–824. PMID: 27510844.
Article4. Kim SJ, Choi BJ, Jeong W, Lee SC. The feasibility of single-port laparoscopic appendectomy using a solo approach: a comparative study. Ann Surg Treat Res. 2016; 90:164–170. PMID: 26942160.
Article5. Velthuis S, van den Boezem PB, Lips DJ, Prins HA, Cuesta MA, Sietses C. Comparison of short-term surgical outcomes after single-incision laparoscopic versus multiport laparoscopic right colectomy: a two-center, prospective case-controlled study of 100 patients. Dig Surg. 2012; 29:477–483. PMID: 23364285.
Article6. Lurje G, Raptis DA, Steinemann DC, Amygdalos I, Kambakamba P, Petrowsky H, et al. Cosmesis and body image in patients undergoing single-port versus conventional laparoscopic cholecystectomy: a multicenter double-blinded randomized controlled trial (SPOCC-trial). Ann Surg. 2015; 262:728–735. PMID: 26583659.7. Podda M, Saba A, Porru F, Pisanu A. Systematic review with meta-analysis of studies comparing single-incision laparoscopic colectomy and multiport laparoscopic colectomy. Surg Endosc. 2016; 30:4697–4720. PMID: 26905578.
Article8. Jaspers JE, Breedveld P, Herder JL, Grimbergen CA. Camera and instrument holders and their clinical value in minimally invasive surgery. Surg Laparosc Endosc Percutan Tech. 2004; 14:145–152. PMID: 15471021.
Article9. Arezzo A, Ulmer F, Weiss O, Schurr MO, Hamad M, Buess GF. Experimental trial on solo surgery for minimally invasive therapy: comparison of different systems in a phantom model. Surg Endosc. 2000; 14:955–959. PMID: 11080411.10. Caliendo M, Kopeinig S. Some practical guidance for the implementation of propensity score matching. J Econ Surv. 2008; 22:31–72.
Article11. Daabiss M. American Society of Anaesthesiologists physical status classification. Indian J Anaesth. 2011; 55:111–115. PMID: 21712864.
Article12. Kang SH, Cho YS, Min SH, Park YS, Ahn SH, Park DJ, et al. Early experience and learning curve of solo single-incision distal gastrectomy for gastric cancer: a review of consecutive 100 cases. Surg Endosc. 2019; 33:3412–3418. PMID: 30604257.
Article13. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6,336 patients and results of a survey. Ann Surg. 2004; 240:205–213. PMID: 15273542.14. Japanese Gastric Cancer Association. Japanese classi fication of gastric carcinoma: 3rd English edition. Gastric Cancer. 2011; 14:101–112. PMID: 21573743.15. Berlth F, Bollschweiler E, Drebber U, Hoelscher AH, Moenig S. Pathohistological classification systems in gastric cancer: diagnostic relevance and prognostic value. World J Gastroenterol. 2014; 20:5679–5684. PMID: 24914328.
Article16. Park DJ, Lee JH, Ahn SH, Eng AK, Kim HH. Single-port laparoscopic distal gastrectomy with D1+β lymph node dissection for gastric cancers: report of 2 cases. Surg Laparosc Endosc Percutan Tech. 2012; 22:e214–e216. PMID: 22874704.17. Ozdemir BA, Thomas RL, Soon Y. Single-port laparoscopic subtotal gastrectomy with DIα lymphadenectomy. Surg Innov. 2011; 18:NP1–NP4.
Article18. Suh YS, Lee HJ, Yang HK. Single incision gastrectomy for gastric cancer. Transl Gastroenterol Hepatol. 2016; 1:41. PMID: 28138608.
Article19. Kim SJ, Lee SC. Technical and instrumental prerequisites for single-port laparoscopic solo surgery: state of art. World J Gastroenterol. 2015; 21:4440–4446. PMID: 25914453.
Article20. Interleukin-6 Receptor Mendelian Randomisation Analysis (IL6R MR) Consortium. Swerdlow DI, Holmes MV, Kuchenbaecker KB, Engmann JE, Shah T, et al. The interleukin-6 receptor as a target for prevention of coronary heart disease: a mendelian randomization analysis. Lancet. 2012; 379:1214–1224. PMID: 22421340.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Laparoscopy-Assisted and Totally Laparoscopic Distal Gastrectomy: The Short-Term Outcome at a Low Volume Center
- Single-incision Laparoscopic Gastrectomy for Gastric Cancer
- Laparoscopic Distal Gastrectomy for Gastric Cancer
- Intracorporeal Anastomosis in Laparoscopic Gastric Cancer Surgery
- Corrigendum: Comparison of Short-Term Postoperative Outcomes in Totally Laparoscopic Distal Gastrectomy Versus Laparoscopy-Assisted Distal Gastrectomy