Clin Endosc.
2021 Jan;54(1):55-63. 10.5946/ce.2020.040.
Confocal Laser Endomicroscopic Findings of Refractory Erosive Reflux Disease versus Non-Erosive Reflux Disease with Anti-Reflux Mucosectomy: An in vivo and ex vivo Study
- Affiliations
-
- 1Department of Gastroenterology, CHA Bundang Medical Center, CHA University College of Medicine, Seongnam, Korea
- 2Division of Gastroenterology, Department of Internal Medicine, Tokat Gaziosmanpaşa University, Faculty of Medicine, Tokat, Turkey
- 3Department of Pediatrics, CHA Bundang Medical Center, CHA University College of Medicine, Seongnam, Korea
- KMID: 2512310
- DOI: http://doi.org/10.5946/ce.2020.040
Abstract
- Background/Aims
To date, there is no standard tool to diagnose gastroesophageal reflux disease (GERD). Typically, GERD is a non-erosive reflux disease (NERD) that does not present endoscopic abnormalities. Confocal laser endomicroscopy (CLE) has been shown to be an effective tool to identify and diagnose GERD. We aimed to investigate the cellular and vascular changes in vivo and ex vivo through CLE in patients with GERD.
Methods
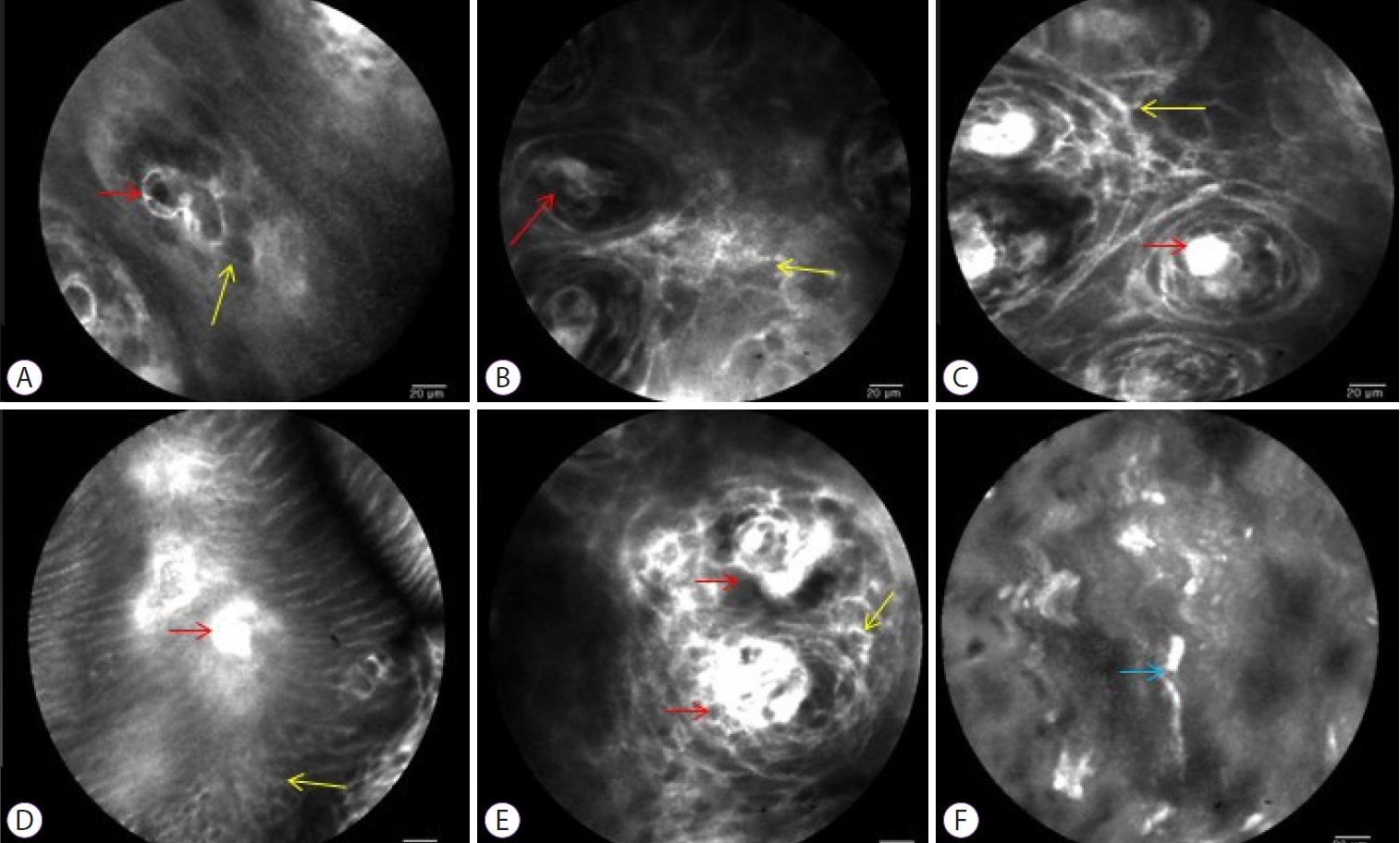
Patients with refractory GERD who underwent mucosectomy were recruited. The distal esophagus was observed in vivo using CLE. Mucosectomy tissue was stained with acriflavine and CLE image was obtained ex vivo. We compared cellular and vascular changes in CLE between erosive reflux disease (ERD), NERD, and a control group.
Results
Eleven patients who underwent anti-reflux mucosectomy and five control patients were enrolled in the study. Patients with ERD and NERD presented greater dilated intercellular space than patients in the control group on CLE image. The diameter, number, and cross-sectional area of the intra-papillary capillary loops (IPCLs) were significantly larger in the ERD group than in the NERD group. The irregular shape of the IPCLs were observed in both patients with ERD and NERD.
Conclusions
The irregular shape of the IPCLs were significantly correlated with a positive diagnosis of GERD. CLE may diagnose NERD with high sensitivity and accuracy.
Keyword
Figure
Reference
-
1. Kim JH, Park H, Lee YC. Is minimal change esophagitis really part of the spectrum of endoscopic findings of gastroesophageal reflux disease? A prospective, multicenter study. Endoscopy. 2011; 43:190–195.
Article2. van Malenstein H, Farré R, Sifrim D. Esophageal dilated intercellular spaces (DIS) and nonerosive reflux disease. Am J Gastroenterol. 2008; 103:1021–1028.
Article3. Armstrong D, Bennett JR, Blum AL, et al. The endoscopic assessment of esophagitis: a progress report on observer agreement. Gastroenterology. 1996; 111:85–92.
Article4. Kahrilas PJ. Diagnosis of symptomatic gastroesophageal reflux disease. Am J Gastroenterol. 2003; 98(3 Suppl):S15–S23.
Article5. Miwa H, Yokoyama T, Hori K, et al. Interobserver agreement in endoscopic evaluation of reflux esophagitis using a modified Los Angeles classification incorporating grades N and M: a validation study in a cohort of Japanese endoscopists. Dis Esophagus. 2008; 21:355–363.
Article6. Edebo A, Tam W, Bruno M, et al. Magnification endoscopy for diagnosis of nonerosive reflux disease: a proposal of diagnostic criteria and critical analysis of observer variability. Endoscopy. 2007; 39:195–201.
Article7. Wasielica-Berger J, Kemona A, Kiśluk J, et al. The added value of magnifying endoscopy in diagnosing patients with certain gastroesophageal reflux disease. Adv Med Sci. 2018; 63:359–366.
Article8. Kiesslich R, Gossner L, Goetz M, et al. In vivo histology of Barrett’s esophagus and associated neoplasia by confocal laser endomicroscopy. Clin Gastroenterol Hepatol. 2006; 4:979–987.
Article9. Polglase AL, McLaren WJ, Skinner SA, Kiesslich R, Neurath MF, Delaney PM. A fluorescence confocal endomicroscope for in vivo microscopy of the upper- and the lower-GI tract. Gastrointest Endosc. 2005; 62:686–695.
Article10. Gheorghe C, Iacob R, Becheanu G, Dumbrav Abreve M. Confocal endomicroscopy for in vivo microscopic analysis of upper gastrointestinal tract premalignant and malignant lesions. J Gastrointestin Liver Dis. 2008; 17:95–100.11. Ismail-Beigi F, Horton PF, Pope CE 2nd. Histological consequences of gastroesophageal reflux in man. Gastroenterology. 1970; 58:163–174.
Article12. Tobey NA, Carson JL, Alkiek RA, Orlando RC. Dilated intercellular spaces: a morphological feature of acid reflux--damaged human esophageal epithelium. Gastroenterology. 1996; 111:1200–1205.13. Xue Y, Zhou LY, Lin SR. Dilated intercellular spaces in gastroesophageal reflux disease patients and the changes of intercellular spaces after omeprazole treatment. Chin Med J (Engl). 2008; 121:1297–1301.
Article14. Dunbar KB, Agoston AT, Odze RD, et al. Association of acute gastroesophageal reflux disease with esophageal histologic changes. JAMA. 2016; 315:2104–2112.
Article15. Kim SE, Kim N, Oh S, et al. Predictive factors of response to proton pump inhibitors in Korean patients with gastroesophageal reflux disease. J Neurogastroenterol Motil. 2015; 21:69–77.
Article16. Inoue H, Ito H, Ikeda H, et al. Anti-reflux mucosectomy for gastroesophageal reflux disease in the absence of hiatus hernia: a pilot study. Ann Gastroenterol. 2014; 27:346–351.17. Sifrim D, Zerbib F. Diagnosis and management of patients with reflux symptoms refractory to proton pump inhibitors. Gut. 2012; 61:1340–1354.
Article18. Frazzoni M, Piccoli M, Conigliaro R, Frazzoni L, Melotti G. Laparoscopic fundoplication for gastroesophageal reflux disease. World J Gastroenterol. 2014; 20:14272–14279.
Article19. Yoo IK, Ko WJ, Kim HS, et al. Anti-reflux mucosectomy using a cap-assisted endoscopic mucosal resection method for refractory gastroesophageal disease: a prospective feasibility study. Surg Endosc. 2020; 34:1124–1131.
Article20. Ho SH, Uedo N, Aso A, et al. Development of image-enhanced endoscopy of the gastrointestinal tract: a review of history and current evidences. J Clin Gastroenterol. 2018; 52:295–306.21. Lv J, Liu D, Ma SY, Zhang J. Investigation of relationships among gastroesophageal reflux disease subtypes using narrow band imaging magnifying endoscopy. World J Gastroenterol. 2013; 19:8391–8397.
Article22. Goetz M. Endomicroscopy and targeted imaging of gastric neoplasia. Gastrointest Endosc Clin N Am. 2013; 23:597–606.
Article23. Bertani H, Frazzoni M, Dabizzi E, et al. Improved detection of incident dysplasia by probe-based confocal laser endomicroscopy in a Barrett’s esophagus surveillance program. Dig Dis Sci. 2013; 58:188–193.
Article24. Canto MI, Anandasabapathy S, Brugge W, et al. In vivo endomicroscopy improves detection of Barrett’s esophagus-related neoplasia: a multicenter international randomized controlled trial (with video). Gastrointest Endosc. 2014; 79:211–221.
Article25. Urban G, Tripathi P, Alkayali T, et al. Deep learning localizes and identifies polyps in real time with 96% accuracy in screening colonoscopy. Gastroenterology. 2018; 155:1069–1078.e8.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Minimal Change Esophagitis
- A Case of Barrett Esophagus Associated with Erosive Reflux Esophagitis in a Patient with Hiatal Hernia
- Underlying Mechanisms and Management of Refractory Gastroesophageal Reflux Disease
- Association Between Non-erosive Reflux Disease and High Risk of Obstructive Sleep Apnea in Korean Population
- Diagnostic Utility of Impedance-pH Monitoring in Refractory Non-erosive Reflux Disease