J Dent Rehabil Appl Sci.
2020 Dec;36(4):232-241. 10.14368/jdras.2020.36.4.232.
Complications of implants confronting the extruded posterior teeth
- Affiliations
-
- 1Department of Prosthodontics, College of Dentistry, Chosun University, Gwangju, Republic of Korea
- KMID: 2512118
- DOI: http://doi.org/10.14368/jdras.2020.36.4.232
Abstract
- Purpose
This study investigated the complications and patterns of implants that confronted with the extruded natural teeth.
Materials and Methods
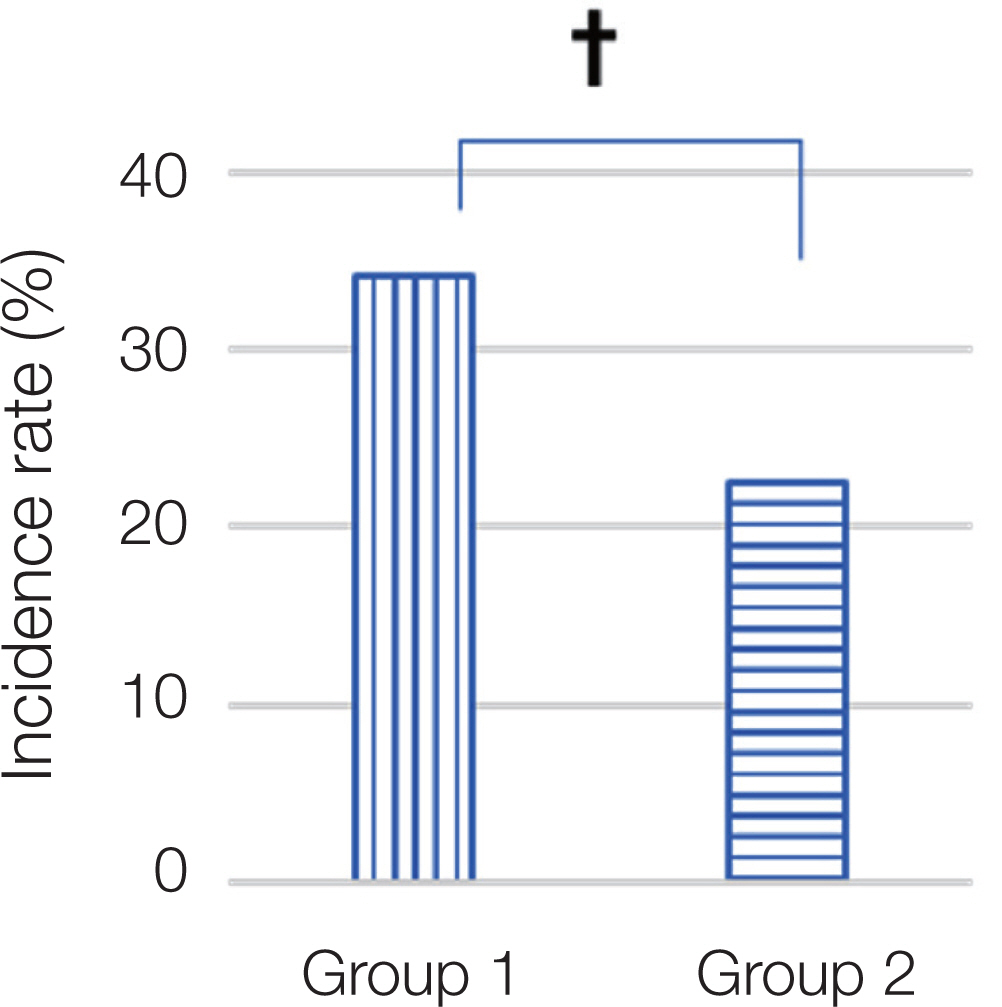
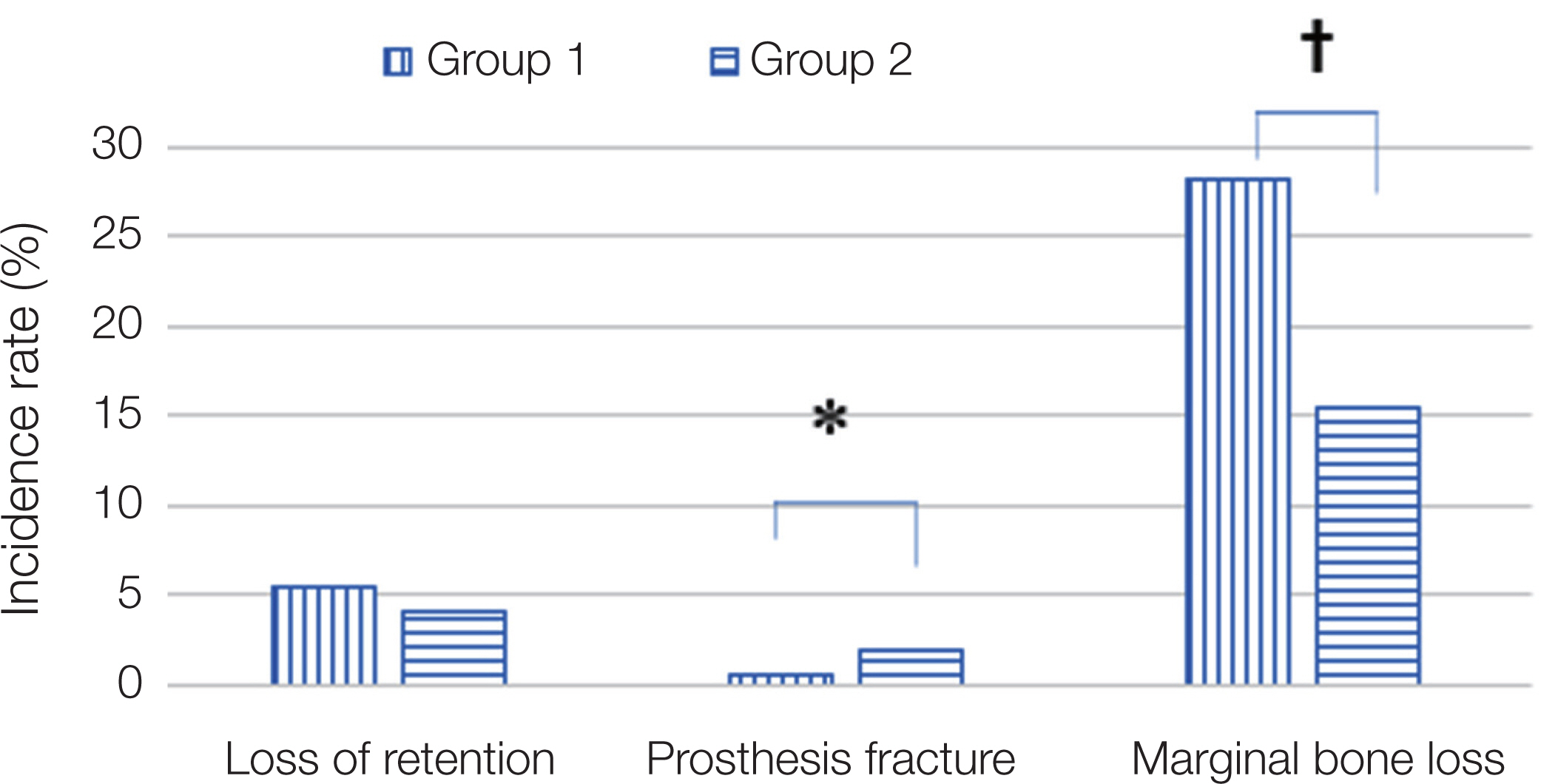
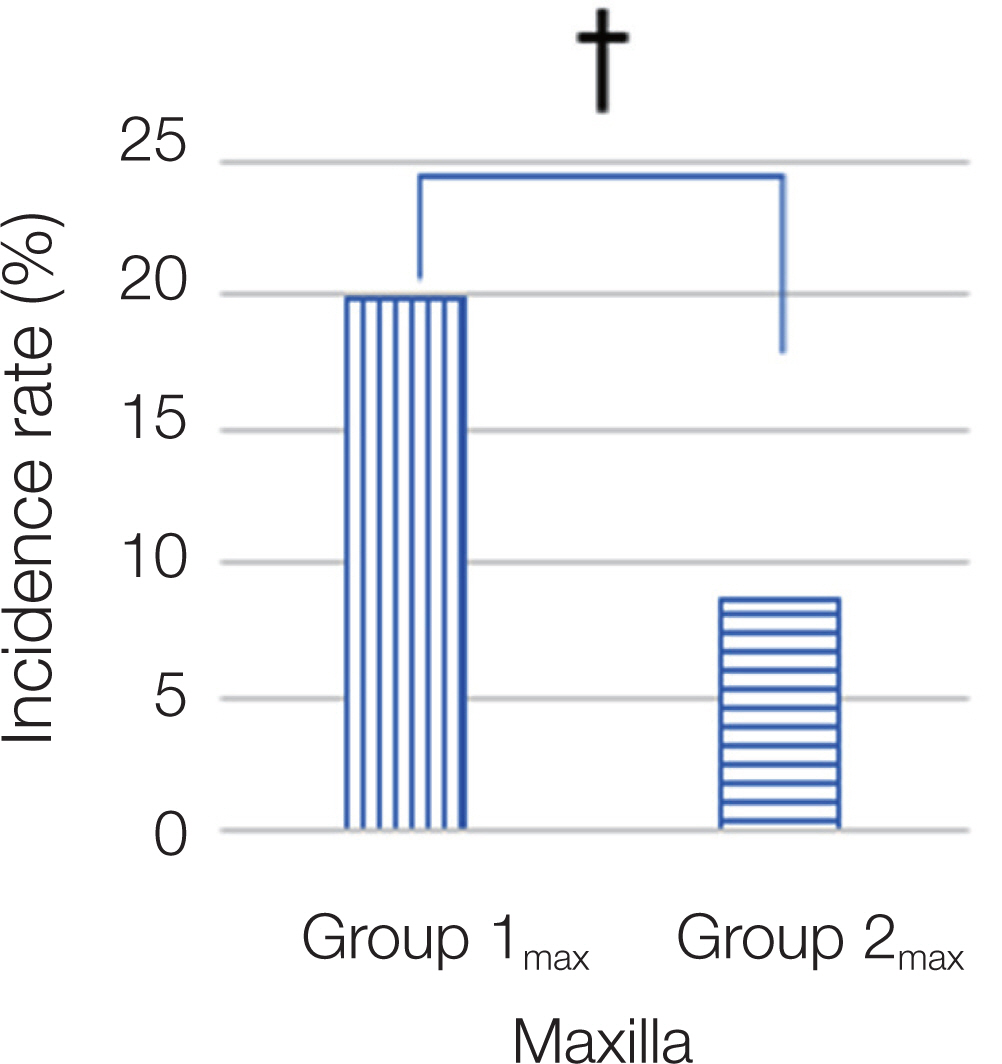
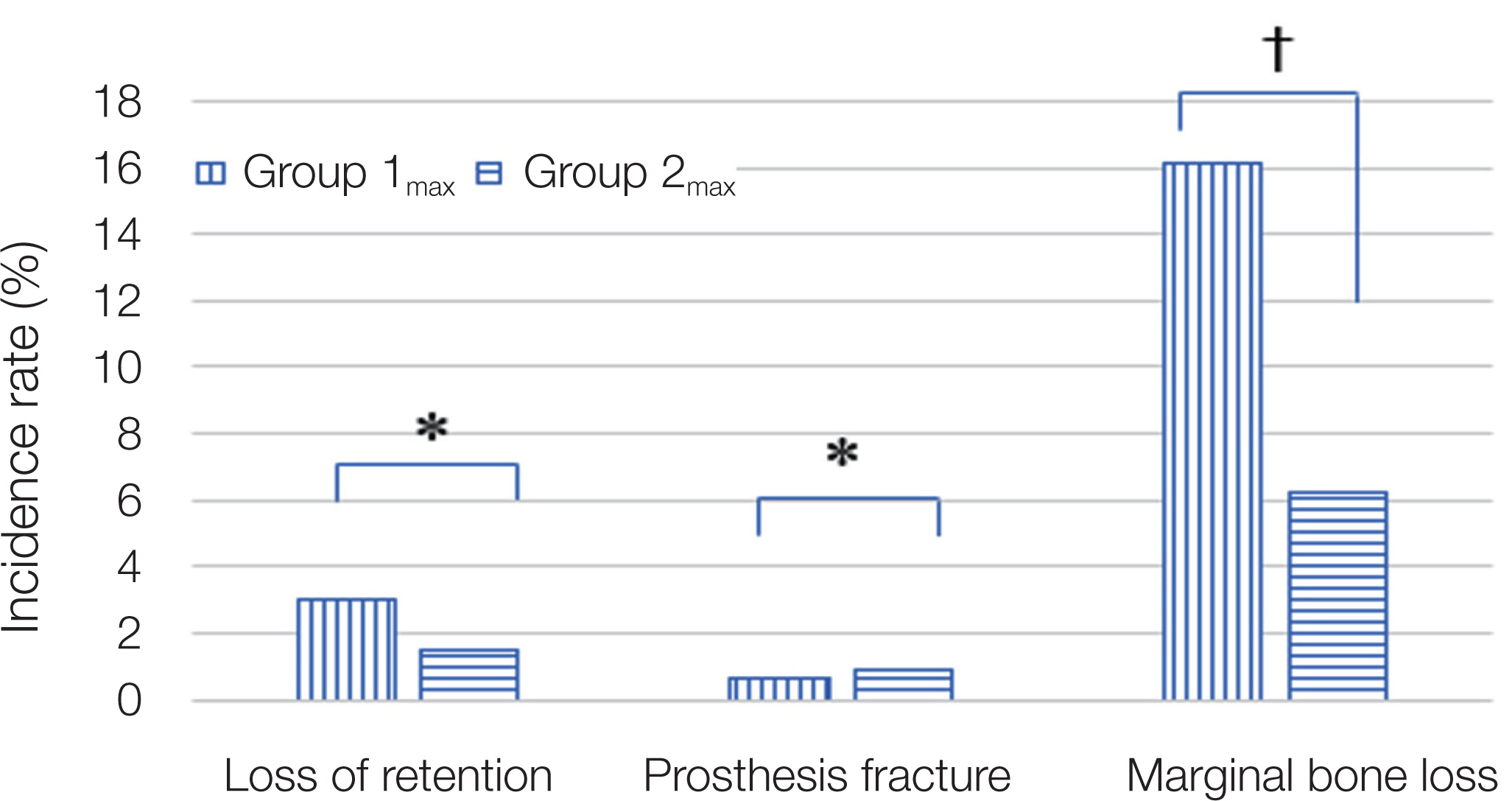
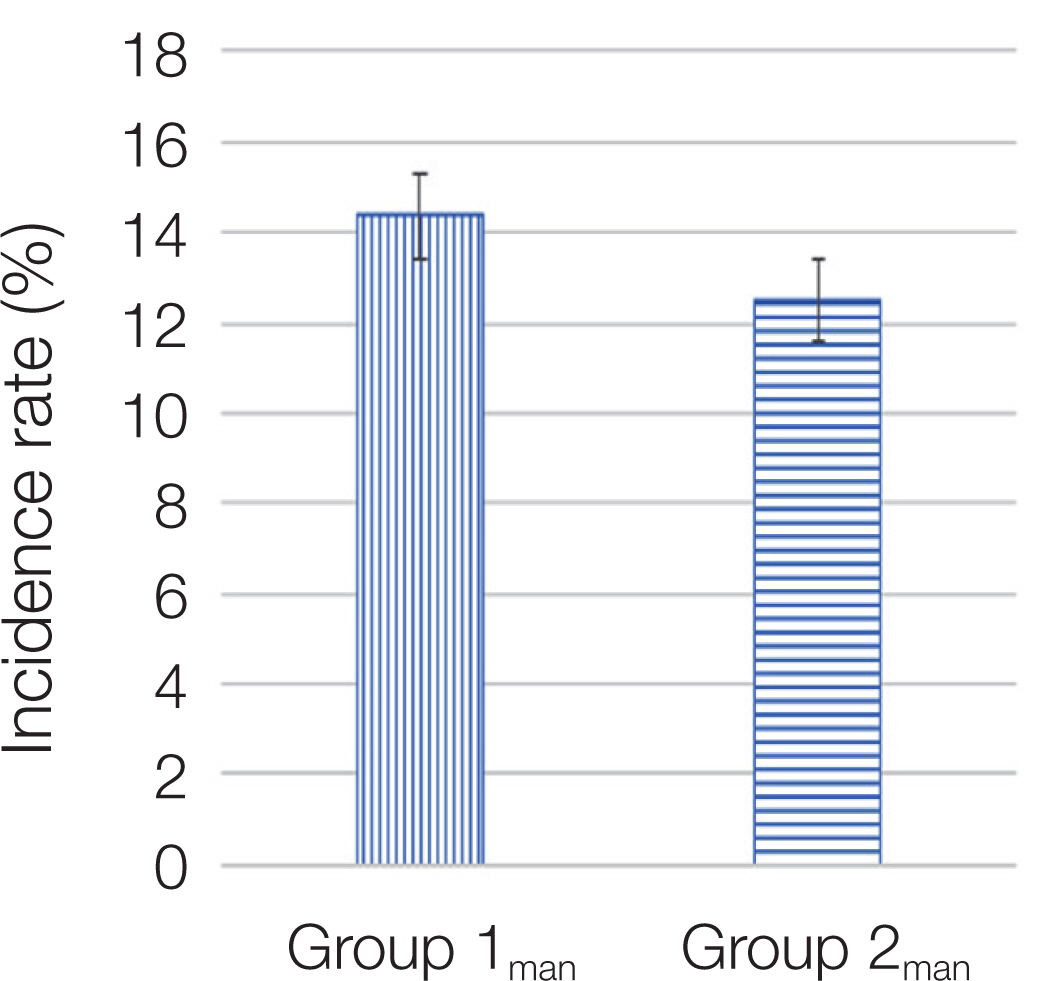
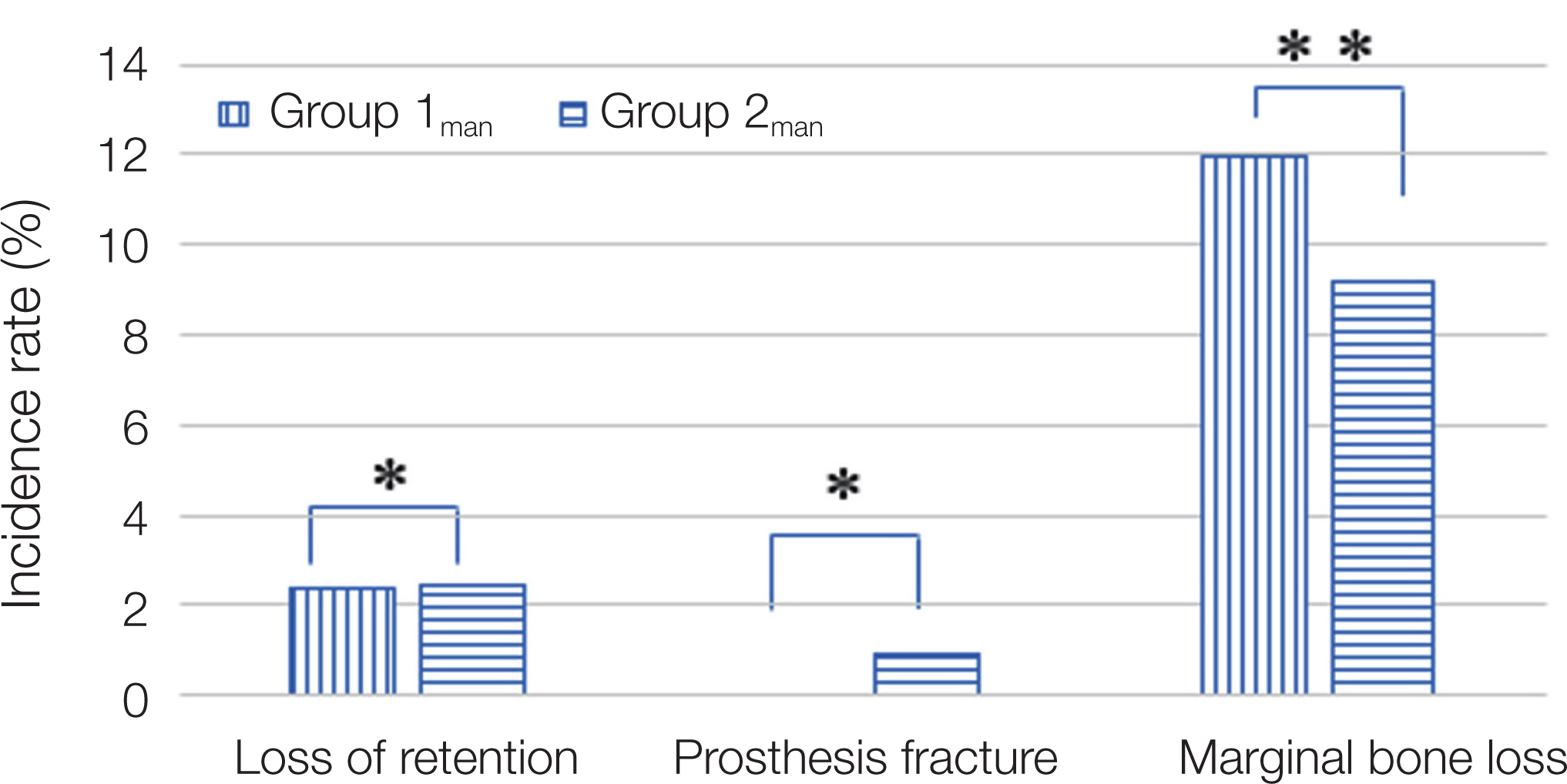
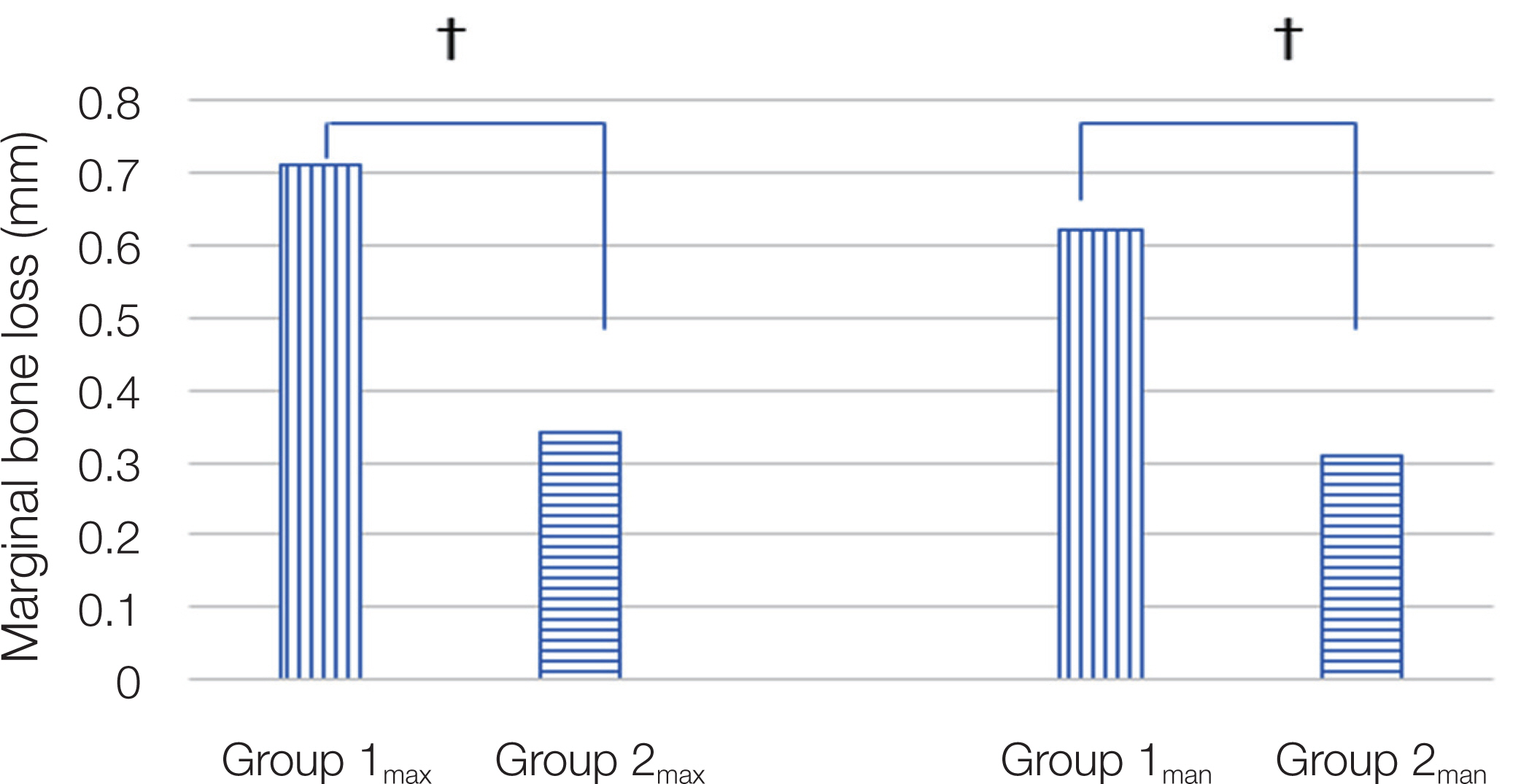
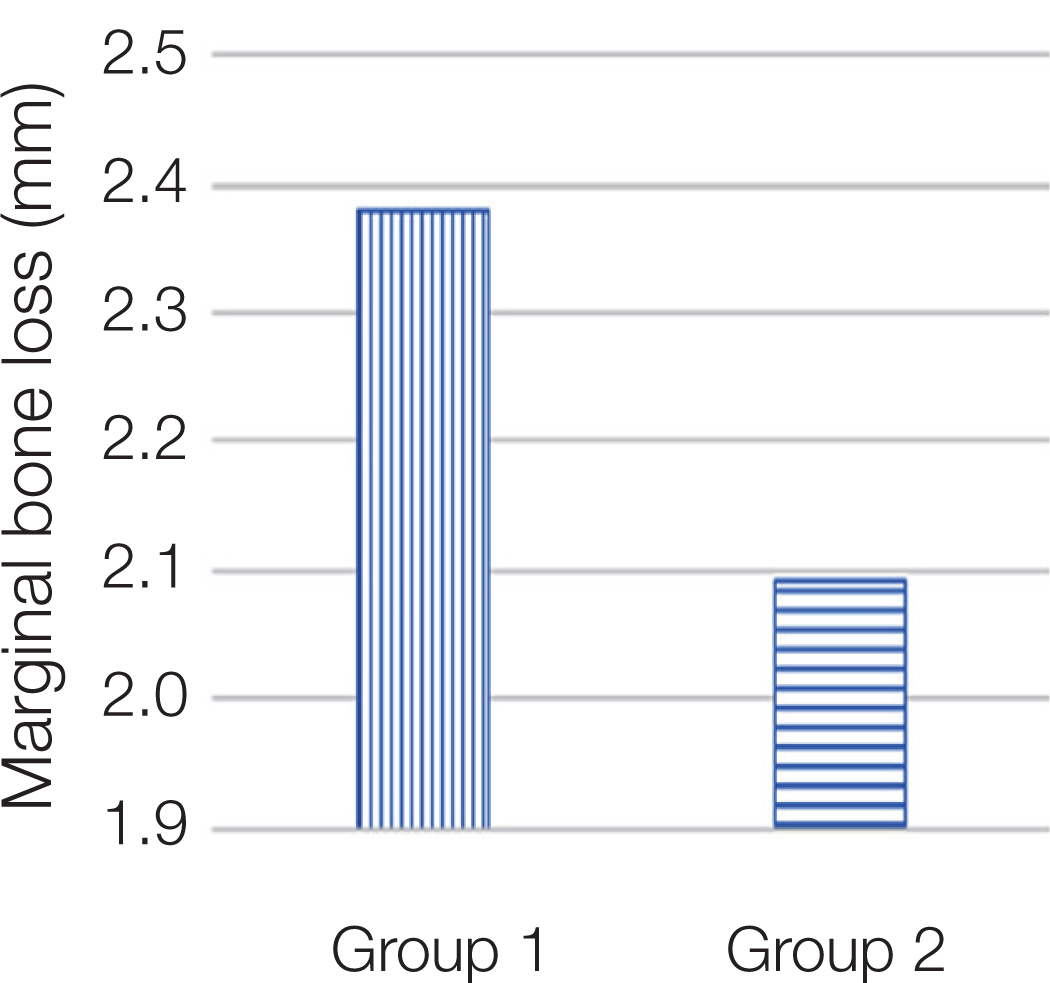
Among patients who received implant treatment between 2006 and 2018 at Chosun University Dental Hos-pital, only implants that had a maintenance period of at least 5 years and that both implants and confronting natural teeth could be measured and compared on a radiograph were selected. They were divided into two groups. Group 1, experimental group consisted of Implants confronting the extruded natural posterior teeth (n = 167: maxilla (Group 1max ) = 92, mandible (Group 1man ) = 75) and Group 2, control group consisted of Implants confronting the normal natural posterior teeth (n = 656: maxilla (Group 2max ) = 272, mandible (Group 2man ) = 384).
Results
The incidence of complications between Group 1 and Group 2 was statistically significant. In particular, there was a statistically significant difference between the frequency of marginal bone loss and the amount of marginal bone loss.
Conclusion
The extruded natural tooth may cause more frequent complications including bone resorption in the oppos-ing implant.
Keyword
Figure
Reference
-
References
1. Berglundh T, Persson L, Klinge B. 2002; A systematic review of the incidence of biological and technical complications in implant dentistry reported in prospective longitudinal studies of at least 5 years. J Clin Periodontol. 29 Suppl 3:197–212. DOI: 10.1034/j.1600-051X.29.s3.12.x. PMID: 12787220.2. Bornstein MM, Halbritter S, Harnisch H, Weber HP, Buser D. 2008; A retrospective analysis of patients referred for implant placement to a specialty clinic: indications, surgical procedures, and early failures. Int J Oral Maxillofac Implants. 23:1109–16. PMID: 19216281.3. Karoussis IK, Müller S, Salvi GE, Heitz-Mayfield LJ, Brägger U, Lang NP. 2004; Association between periodontal and peri-implant conditions: a 10-year prospective study. Clin Oral Implants Res. 15:1–7. DOI: 10.1111/j.1600-0501.2004.00982.x. PMID: 14731172.4. Karoussis IK, Kotsovilis S, Fourmousis I. 2007; A comprehensive and critical review of dental implant prognosis in periodontally compromised partially edentulous patients. Clin Oral Implants Res. 18:669–79. DOI: 10.1111/j.1600-0501.2007.01406.x. PMID: 17868376.5. Lang NP, Pjetursson BE, Tan K, Brägger U, Egger M, Zwahlen M. 2004; A systematic review of the survival and complication rates of fixed partial dentures (FPDs) after an observation period of at least 5 years. II. Combined tooth-implant-supported FPDs. Clin Oral Implants Res. 15:643–53. DOI: 10.1111/j.1600-0501.2004.01118.x. PMID: 15533125.6. Goodacre CJ, Bernal G, Rungcharassaeng K, Kan JY. 2003; Clinical complications with implants and implant prostheses. J Prosthet Dent. 90:121–32. DOI: 10.1016/S0022-3913(03)00212-9. PMID: 12886205.7. Jung RE, Pjetursson BE, Glauser R, Zembic A, Zwahlen M, Lang NP. 2008; A systematic review of the 5-year survival and complication rates of implantsupported single crowns. Clin Oral Implants Res. 19:119–30. DOI: 10.1111/j.1600-0501.2007.01453.x. PMID: 18067597.8. Hanif A, Qureshi S, Sheikh Z, Rashid H. 2017; Complications in implant dentistry. Eur J Dent. 11:135–40. DOI: 10.4103/ejd.ejd_340_16. PMID: 28435381. PMCID: PMC5379828.9. Henry PJ, Laney WR, Jemt T, Harris D, Krogh PH, Polizzi G, Zarb GA, Herrmann I. 1996; Osseointegrated implants for single-tooth replacement: a prospective 5-year multicenter study. Int J Oral Maxillofac Implants. 11:450–5. PMID: 8803340.10. Taylor RC, McGlumphy EA, Tatakis DN, Beck FM. 2004; Radiographic and clinical evaluation of singletooth Biolok implants: a 5-year study. Int J Oral Maxillofac Implants. 19:849–54. PMID: 15623060.11. Jemt T. 2008; Single implants in the anterior maxilla after 15 years of follow-up: comparison with central implants in the edentulous maxilla. Int J Prosthodont. 21:400–8. PMID: 18950060.12. Pjetursson BE, Asgeirsson AG, Zwahlen M, Sailer I. 2014; Improvements in implant dentistry over the last decade: comparison of survival and complication rates in older and newer publications. Int J Oral Maxillofac Implants. 29 suppl:308–24. DOI: 10.11607/jomi.2014suppl.g5.2. PMID: 24660206.13. Sadid-Zadeh R, Kutkut A, Kim H. 2015; Prosthetic failure in implant dentistry. Dent Clin North Am. 59:195–214. DOI: 10.1016/j.cden.2014.08.008. PMID: 25434566.14. Galindo-Moreno P, León-Cano A, Ortega-Oller I, Monje A, Valle FO, Catena A. 2015; Marginal bone loss as success criterion in implant dentistry: beyond 2 mm. Clin Oral Implants Res. 26:e28–34. DOI: 10.1111/clr.12324. PMID: 24383987.15. Kiliaridis S, Lyka I, Friede H, Carlsson GE, Ahlqwist M. 2000; Vertical position, rotation, and tipping of molars without antagonists. Int J Prosthodont. 13:480–6. PMID: 11203673.16. Craddock HL, Youngson CC. 2004; A study of the incidence of overeruption and occlusal interferences in unopposed posterior teeth. Br Dent J. 196:341–8. DOI: 10.1038/sj.bdj.4811082. PMID: 15044991.17. Craddock HL, Youngson CC, Manogue M, Blance A. 2007; Occlusal changes following posterior tooth loss in adults. Part 1: a study of clinical parameters associated with the extent and type of supra-eruption in unopposed posterior teeth. J Prosthodont. 16:485–94. DOI: 10.1111/j.1532-849X.2007.00212.x. PMID: 17559530.18. Hirschfeld I. 1937; The individual missing tooth: a factor in dental and periodontal disease. J Am Dent Assoc. 24:67–82. DOI: 10.14219/jada.archive.1937.0005.19. Kim YK, Ahn KJ, Yun PY, Yi YJ, Kim SG. 2016; The clinical prognosis of implants that are placed against super-erupted opposing dentition. J Korean Assoc Oral Maxillofac Surg. 42:139–43. DOI: 10.5125/jkaoms.2016.42.3.139. PMID: 27429935. PMCID: PMC4940198.20. Han HJ. 2010. Evaluation of implant failure causes: a 19-Year retrospective study. PhD Thesis. The Graduate School, Yonsei University.21. Garaicoa-Pazmiño C, Suárez-López del Amo F, Monje A, Catena A, Ortega-Oller I, Galindo-Moreno P, Wang HL. 2014; Influence of crown/implant ratio on marginal bone loss: a systematic review. 85:1214–21. DOI: 10.1902/jop.2014.130615. PMID: 24444399.22. Monje A, Suarez F, Galindo-Moreno P, García-Nogales A, Fu JH, Wang HL. 2014; A systematic review on marginal bone loss around short dental implants (<10 mm) for implant-supported fixed prostheses. Clin Oral Implants Res. 25:1119–24. DOI: 10.1111/clr.12236. PMID: 23937287.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Complications of Teeth and Implants Adjacent to Canine Implants: A Retrospective Study
- A photoelastic study of the stress distribution by multiloop edgewise arch wire
- Orthodontic intrusion treatment of mandibular anterior teeth in a periodontal patient with hyperdivergent skeletal pattern: 8-year follow-up
- Surgical Repositioning of the Extruded Dento-alveolar Segments by the Single-Stage Posterior Maxillary Segmental Osteotomy
- An anatomical study using CT images for the implantation of micro-implants