Obstet Gynecol Sci.
2021 Jan;64(1):34-41. 10.5468/ogs.20157.
Effects of excessive tea consumption on pregnancy weight gain and neonatal birth weight
- Affiliations
-
- 1Department of Obstetrics and Gynecology, College of Medicine, University of Baghdad, Iraq
- 2Department of Pediatrics, Al-Kindy College of Medicine, University of Baghdad, Baghdad, Iraq
- KMID: 2511563
- DOI: http://doi.org/10.5468/ogs.20157
Abstract
Objective
Tea lovers are increasing worldwide. We hope that this report is the first to discuss the possible impacts of high black tea consumption on gestational weight gain (GWG) and birth parameters.
Methods
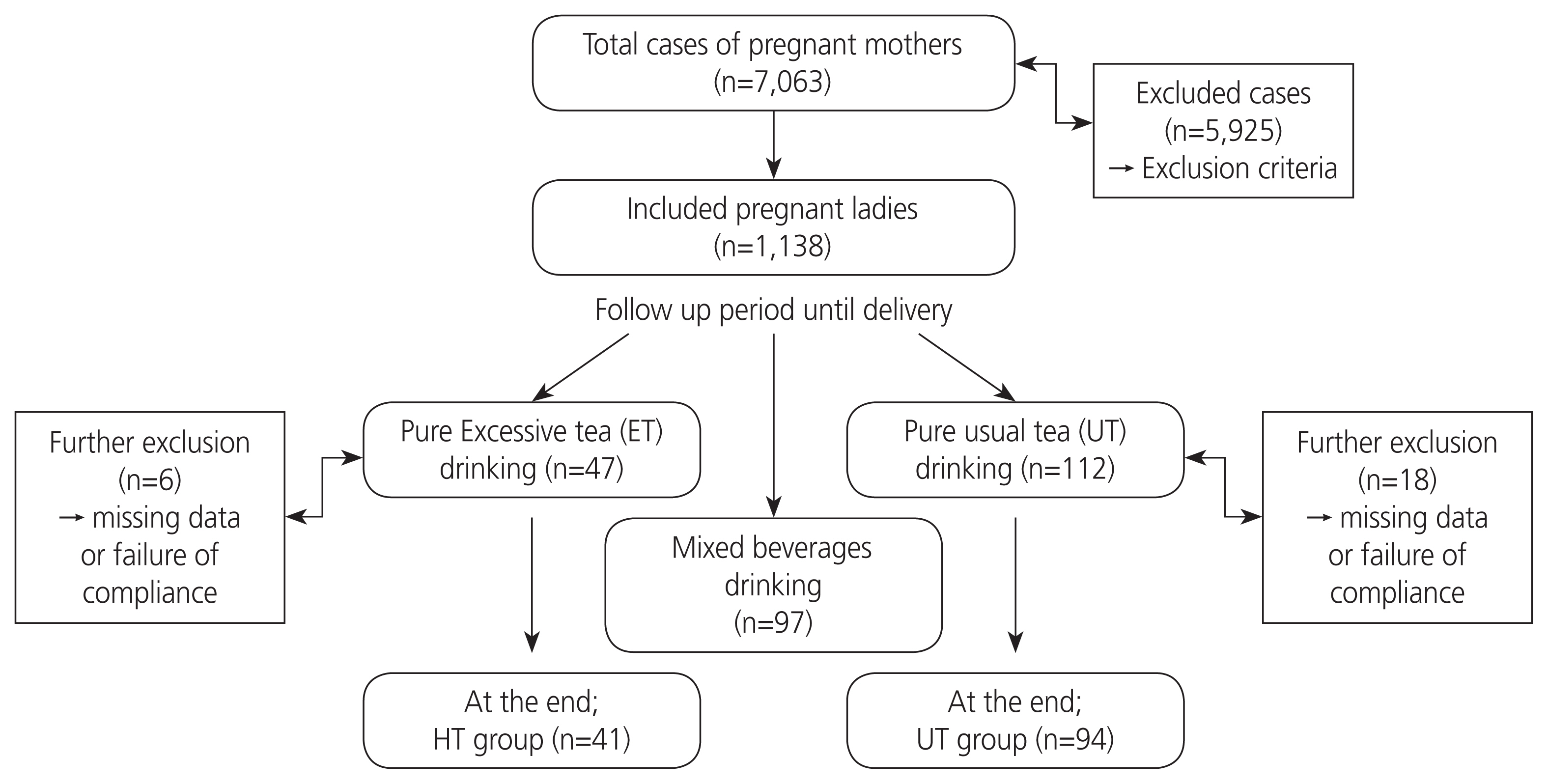
Throughout one year, a total of 7,063 pregnant ladies coming for first antenatal visit were screened in a major tertiary center. Of them, 1,138 were involved and divided according to their preference into 3 groups: excessive tea (ET), usual tea (UT), and mixed beverages group. The study included women who gave birth to healthy neonates.
Results
The rate of ET consumption was 4.13% with a total of 41 cases. The UT group (controls) comprised 94 women. ET was significantly associated (P<0.05) with maternal age, parity, occupation, smoking, and poor GWG starting from 30 weeks’ gestation until delivery, low birth weight, and small for gestational age (SGA). Poor GWG had a higher relative risk (with 95% confidence interval) in the ET group than in the UT group in crude (1.84 [0.85–2.43]) and risk adjusted models (1.25 [0.28–2.26]). Further, similar results were obtained for SGA in the crude and 3 adjusted models, where the first model was adjusted for bio-obstetrical variables, the second for social parameters, and the third for all factors included in the previous models (1.53 [0.62–2.81], 1.52 [0.71–2.50], and 1.46 [0.78–2.39]), respectively.
Conclusion
Consumption of large amounts of daily black tea during pregnancy (≥1,500 mL) is a significant cause of poor GWG and SGA.
Keyword
Figure
Reference
-
References
1. Karalexi MA, Dessypris N, Clavel J, Metayer C, Erdmann F, Orsi L, et al. Coffee and tea consumption during pregnancy and risk of childhood acute myeloid leukemia: a Childhood Leukemia International Consortium (CLIC) study. Cancer Epidemiol. 2019; 62:101581.
Article2. Dey A, Gomes A, Dasgupta SC. Black tea (Camellia sinensis) extract induced changes in blood and liver parameters on pregnant and lactating experimental albino rats. Proc Zool Soc. 2019; 72:25–31.
Article3. Vuong QV. Epidemiological evidence linking tea consumption to human health: a review. Crit Rev Food Sci Nutr. 2014; 54:523–36.
Article4. Kadhim Jasim S, Al-Momen H, Al-Asadi F. Maternal anemia prevalence and subsequent neonatal complications in Iraq. Open Access Maced J Med Sci. 2020; 8:71–5.
Article5. Badon SE, Miller RS, Qiu C, Sorensen TK, Williams MA, Enquobahrie DA. Maternal healthy lifestyle during early pregnancy and offspring birthweight: differences by offspring sex. J Matern Fetal Neonatal Med. 2018; 31:1111–7.
Article6. Brown SM, Aljefri K, Waas R, Hampton P. Systemic medications used in treatment of common dermatological conditions: safety profile with respect to pregnancy, breast feeding and content in seminal fluid. J Dermatolog Treat. 2019; 30:2–18.
Article7. Qian J, Chen Q, Ward SM, Duan E, Zhang Y. Impacts of caffeine during pregnancy. Trends Endocrinol Metab. 2020; 31:218–27.
Article8. Darakjian LI, Kaddoumi A. Physiologically based pharmacokinetic/ pharmacodynamic model for caffeine disposition in pregnancy. Mol Pharm. 2019; 16:1340–9.9. Hahn M, Baierle M, Charão MF, Bubols GB, Gravina FS, Zielinsky P, et al. Polyphenol-rich food general and on pregnancy effects: a review. Drug Chem Toxicol. 2017; 40:368–74.
Article10. Vazquez-Gomez M, Garcia-Contreras C, Torres-Rovira L, Pesantez JL, Gonzalez-Añover P, Gomez-Fidalgo E, et al. Polyphenols and IUGR pregnancies: maternal hydroxytyrosol supplementation improves prenatal and early–postnatal growth and metabolism of the offspring. PLoS One. 2017; 12:e0177593.
Article11. Okubo H, Miyake Y, Tanaka K, Sasaki S, Hirota Y. Maternal total caffeine intake, mainly from Japanese and Chinese tea, during pregnancy was associated with risk of preterm birth: the Osaka Maternal and Child Health Study. Nutr Res. 2015; 35:309–16.
Article12. Chen IJ, Liu CY, Chiu JP, Hsu CH. Therapeutic effect of high-dose green tea extract on weight reduction: a randomized, double-blind, placebo-controlled clinical trial. Clin Nutr. 2016; 35:592–9.
Article13. Jiang AC, Chan EY, Jakate S, Shah N. Abstracts 1296: Elevated CA 19-9 associated with heavy black tea consumption. Am J Gastroenterol. 2019; 114:S719–20.14. Kadhim Jasim S, Al-Momen H, Majeed BA, Hussein MJ. Rate of fetal macrosomia with maternal and early neonatal complications in internally moved people affected by violence. Int J Med Res Health Sci. 2018; 7:141–6.15. Al-Momen H, Muhammed MK, Alshaheen AA. Neonatal seizures in Iraq: cause and outcome. Tohoku J Exp Med. 2018; 246:245–9.
Article16. Vitti FP, Grandi C, Cavalli RC, Simões VM, Batista RF, Cardoso VC. Association between caffeine consumption in pregnancy and low birth weight and preterm birth in the birth Cohort of Ribeirão Preto. Rev Bras Ginecol Obstet. 2018; 40:749–56.
Article17. Pacheco AH, Araujo DM, Lacerda EM, Kac G. Caffeine consumption by pregnant women selected from a Health Care Center in the municipality of Rio de Janeiro, Brazil. Rev Bras Ginecol Obstet. 2008; 30:232–40.18. Dong Y, Zhang FD, Wang T, Yu HL, Ling WH, Cai MQ. Tea drinking habits among residents in Beijing, Shanghai, and Guangzhou. J Environ Occup Med. 2012; 29:569–71.19. van der Hoeven T, Browne JL, Uiterwaal CS, van der Ent CK, Grobbee DE, Dalmeijer GW. Antenatal coffee and tea consumption and the effect on birth outcome and hypertensive pregnancy disorders. PLoS One. 2017; 12:e0177619.
Article20. Lu JH, He JR, Shen SY, Wei XL, Chen NN, Yuan MY, et al. Does tea consumption during early pregnancy have an adverse effect on birth outcomes? Birth. 2017; 44:281–9.
Article21. Chang CS, Chang YF, Liu PY, Chen CY, Tsai YS, Wu CH. Smoking, habitual tea drinking and metabolic syndrome in elderly men living in rural community: the Tianliao old people (TOP) study 02. PLoS One. 2012; 7:e38874.
Article22. Al-Momen H, Hussein HK, Al-Attar Z, Hussein MJ. Green tea influence on iron overload in thalassemia intermedia patients: a randomized controlled trial. F1000Res. 2020; 9:1136.
Article23. Rothenberg DO, Zhou C, Zhang L. A review on the weight-loss effects of oxidized tea polyphenols. Molecules. 2018; 23:1176.
Article24. Machmud PB, Hatma RD, Syafiq A. Tea consumption and iron-deficiency anemia among pregnant woman in Bogor District, Indonesia. Indones J Micronutrient. 2019; 10:91–100.
Article25. Sato AP, Fujimori E. Nutritional status and weight gain in pregnant women. Rev Lat Am Enfermagem. 2012; 20:462–8.
Article26. Scholl TO, Hediger ML. Anemia and iron-deficiency anemia: compilation of data on pregnancy outcome. Am J Clin Nutr. 1994; 59:492S–500S.
Article27. Chen X, Zhao D, Mao X, Xia Y, Baker PN, Zhang H. Maternal dietary patterns and pregnancy outcome. Nutrients. 2016; 8:351.
Article28. Shin D, Lee KW, Song WO. Dietary patterns during pregnancy are associated with gestational weight gain. Matern Child Health J. 2016; 20:2527–38.
Article29. Goldstein RF, Abell SK, Ranasinha S, Misso M, Boyle JA, Black MH, et al. Association of gestational weight gain with maternal and infant outcomes: a systematic review and meta-analysis. JAMA. 2017; 317:2207–25.
Article30. Kominiarek MA, Saade G, Mele L, Bailit J, Reddy UM, Wapner RJ, et al. Association between gestational weight gain and perinatal outcomes. Obstet Gynecol. 2018; 132:875–81.
Article31. Rhee J, Kim R, Kim Y, Tam M, Lai Y, Keum N, et al. Maternal caffeine consumption during pregnancy and risk of low birth weight: a dose-response meta-analysis of observational studies. PLoS One. 2015; 10:e0132334.
Article32. Sasaki S, Limpar M, Sata F, Kobayashi S, Kishi R. Interaction between maternal caffeine intake during pregnancy and CYP1A2 C164A polymorphism affects infant birth size in the Hokkaido study. Pediatr Res. 2017; 82:19–28.
Article33. Abdul-Hussain DA, Hamad MN. Gravimetric estimation of caffeine in different commercial kinds of tea found in the Iraqi market. Iraqi J Pharm Sci. 2010; 19:48–53.34. Hoyt AT, Browne M, Richardson S, Romitti P, Druschel C. National Birth Defects Prevention Study. Maternal caffeine consumption and small for gestational age births: results from a population-based case-control study. Matern Child Health J. 2014; 18:1540–51.
Article35. Sengpiel V, Elind E, Bacelis J, Nilsson S, Grove J, Myhre R, et al. Maternal caffeine intake during pregnancy is associated with birth weight but not with gestational length: results from a large prospective observational cohort study. BMC Med. 2013; 11:42.
Article36. Jarosz M, Wierzejska R, Siuba M. Maternal caffeine intake and its effect on pregnancy outcomes. Eur J Obstet Gynecol Reprod Biol. 2012; 160:156–60.
Article37. Kadhim Jasim S, Al-Momen H, Al-Naddawi AM. Prediction of maternal diabetes and adverse neonatal outcome in normotensive pregnancy using serum uric acid. Int J Res Pharm Sci. 2019; 10:3563–9.38. Ha S, Hu H, Roussos-Ross D, Haidong K, Roth J, Xu X. The effects of air pollution on adverse birth outcomes. Environ Res. 2014; 134:198–204.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Maternal Weight Gain Pattern and Birth Weight
- The influence of maternal weight gain to birth weight
- Prepregnancy weight, maternal weight gain, and birth weight
- The Effect of Prepregnancy Body Mass Index and Weight Gain during Pregnancy on Infant Birth Weight
- Association between maternal weight gain rate of each trimester and neonatal birth weight