Clin Endosc.
2020 Nov;53(6):727-734. 10.5946/ce.2020.017.
Outcomes of Endoscopic Management among Patients with Bile Leak of Various Etiologies at a Tertiary Care Center
- Affiliations
-
- 1Department of Gastroenterology, Seth GS Medical College and KEM Hospital, Mumbai, India
- KMID: 2511233
- DOI: http://doi.org/10.5946/ce.2020.017
Abstract
- Background/Aims
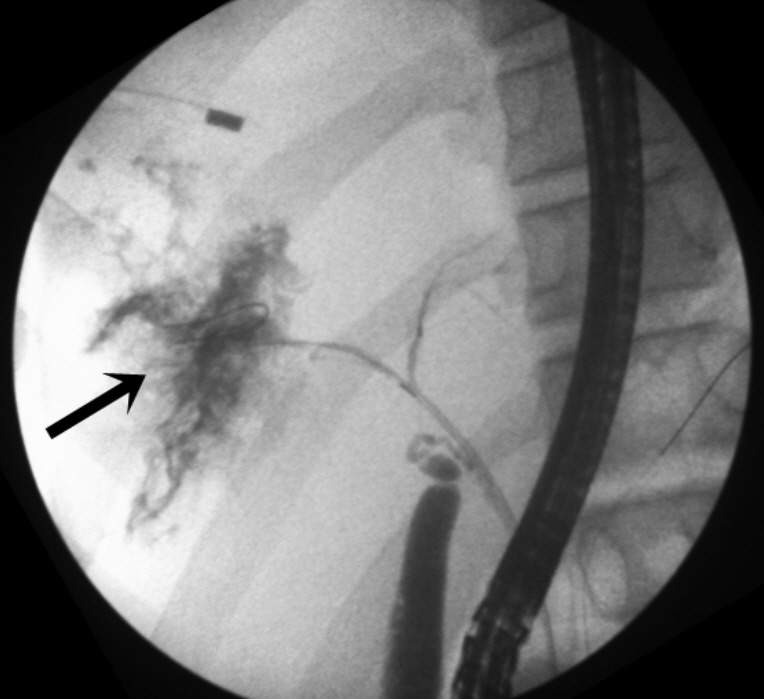
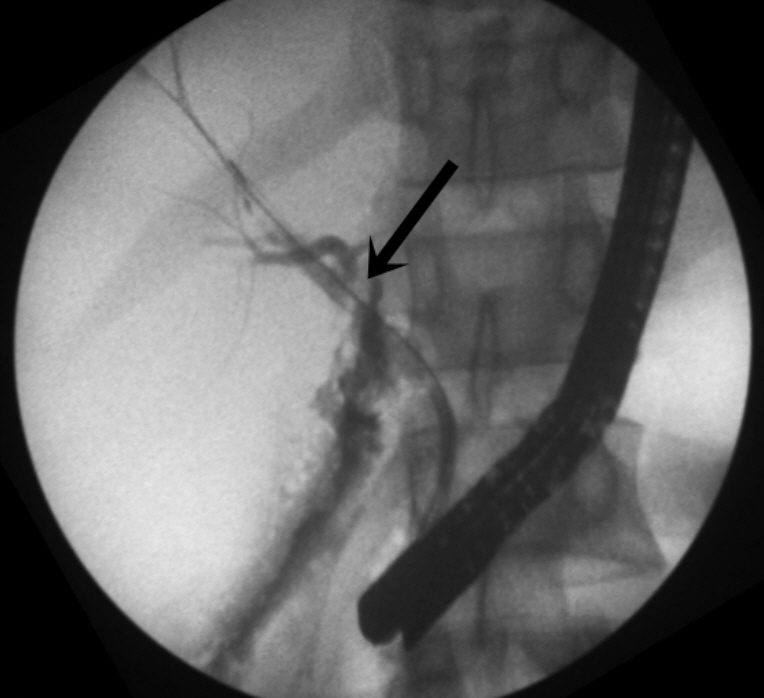
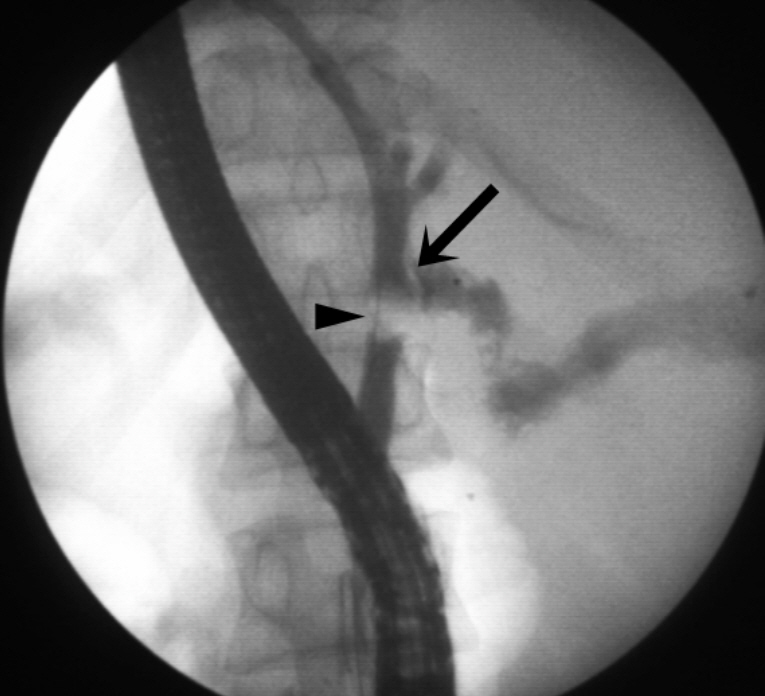
Bile leak is a common complication of cholecystectomy, and it is also observed in other conditions such as ruptured liver abscess, hydatid cyst, and trauma. Endoscopic retrograde cholangiopancreatography (ERCP) is the first-line management for such conditions. However, studies on the outcomes of endoscopic management for bile leaks with etiologies other than post-cholecystectomy injury are extremely limited.
Methods
We conducted a retrospective review of patients with symptomatic bile leak who were referred to a tertiary care center and who underwent ERCP between April 2016 and April 2019. The primary outcome was complete symptomatic resolution without extravasation of the contrast medium during the second ERCP conducted after 6 weeks.
Results
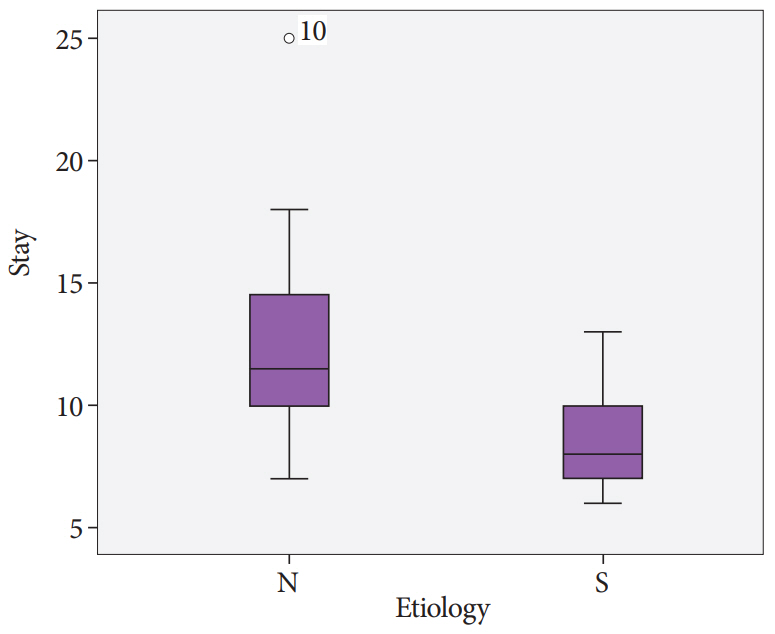
In total, 71 patients presented with symptomatic bile leak. The etiologies of bile leak were post-cholecystectomy injury in 34 (47.8%), liver abscess in 20 (28.1%), and post-hydatid cyst surgery in 11 (15.4%) patients. All patients were managed with ERCP, sphincterotomy, and stent placement for 6 weeks, except for one who underwent surgery. The primary outcome was achieved in 65 (91.5%) of 71 patients. There was no significant difference in terms of outcome in relation to the interval between the diagnosis of bile leak and ERCP.
Conclusions
Most patients with bile leak can be successfully managed with ERCP even when performed on an elective basis.
Keyword
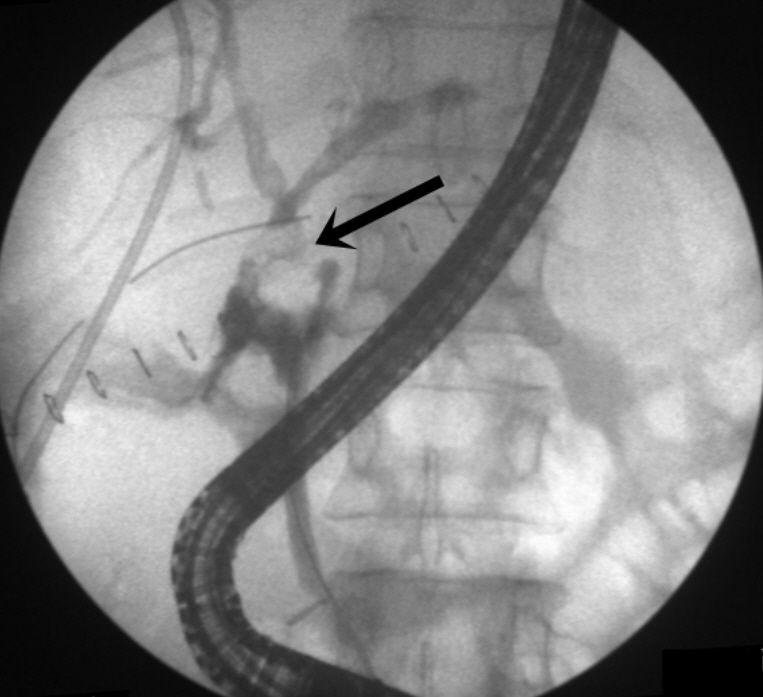
Figure
Cited by 1 articles
-
The Need for a Better-Designed Study of the Outcomes of Endoscopic Management of Bile Leak
Hyung Ku Chon, Eun Ji Shin, Seong-Hun Kim
Clin Endosc. 2020;53(6):633-635. doi: 10.5946/ce.2020.263.
Reference
-
1. Koch M, Garden OJ, Padbury R, et al. Bile leakage after hepatobiliary and pancreatic surgery: a definition and grading of severity by the International Study Group of Liver Surgery. Surgery. 2011; 149:680–688.
Article2. Morgenstern L, Wong L, Berci G. Twelve hundred open cholecystectomies before the laparoscopic era. A standard for comparison. Arch Surg. 1992; 127:400–403.3. Roslyn JJ, Binns GS, Hughes EF, Saunders-Kirkwood K, Zinner MJ, Cates JA. Open cholecystectomy. A contemporary analysis of 42,474 patients. Ann Surg. 1993; 218:129–137.
Article4. Deziel DJ, Millikan KW, Economou SG, Doolas A, Ko ST, Airan MC. Complications of laparoscopic cholecystectomy: a national survey of 4,292 hospitals and an analysis of 77,604 cases. Am J Surg. 1993; 165:9–14.
Article5. Albasini JL, Aledo VS, Dexter SP, Marton J, Martin IG, McMahon MJ. Bile leakage following laparoscopic cholecystectomy. Surg Endosc. 1995; 9:1274–1278.
Article6. Barkun AN, Rezieg M, Mehta SN, et al. Postcholecystectomy biliary leaks in the laparoscopic era: risk factors, presentation, and management. McGill Gallstone Treatment Group. Gastrointest Endosc. 1997; 45:277–282.7. Agarwal DK, Baijal SS, Roy S, Mittal BR, Gupta R, Choudhuri G. Percutaneous catheter drainage of amebic liver abscesses with and without intrahepatic biliary communication: a comparative study. Eur J Radiol. 1995; 20:61–64.8. Chautems R, Bühler LH, Gold B, et al. Surgical management and long-term outcome of complicated liver hydatid cysts caused by Echinococcus granulosus. Surgery. 2005; 137:312–316.
Article9. Huang CS, Lichtenstein DR. Postcholecystectomy bile leak: what is the optimal treatment? Gastrointest Endosc. 2005; 61:276–278.
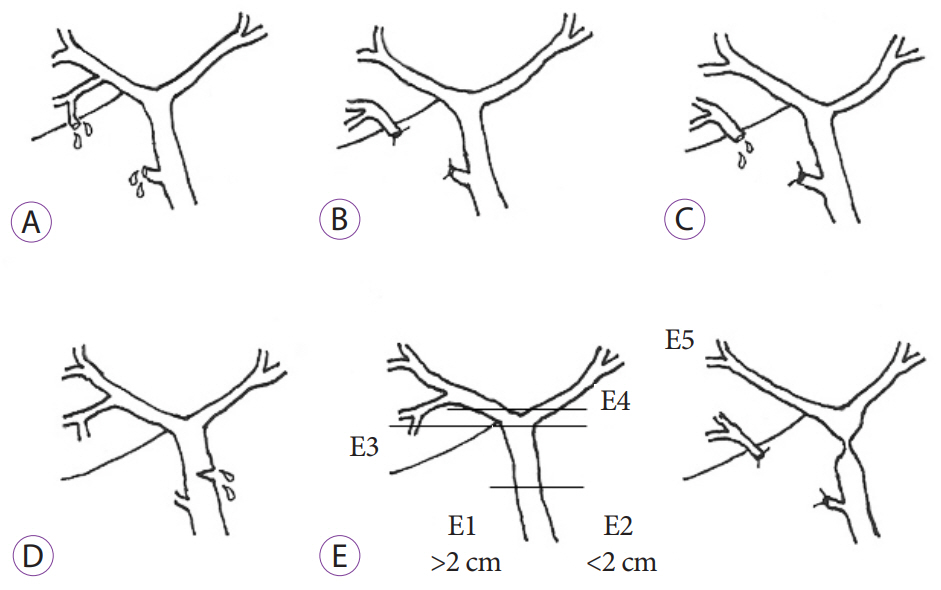
Article10. Sandha GS, Bourke MJ, Haber GB, Kortan PP. Endoscopic therapy for bile leak based on a new classification: results in 207 patients. Gastrointest Endosc. 2004; 60:567–574.
Article11. Abbas A, Sethi S, Brady P, Taunk P. Endoscopic management of postcholecystectomy biliary leak: when and how? A nationwide study. Gastrointest Endosc. 2019; 90:233–241.e1.
Article12. Kim KH, Kim TN. Endoscopic management of bile leakage after cholecystectomy: a single-center experience for 12 years. Clin Endosc. 2014; 47:248–253.
Article13. Strasberg SM, Hertl M, Soper NJ. An analysis of the problem of biliary injury during laparoscopic cholecystectomy. J Am Coll Surg. 1995; 180:101–125.14. Sharma BC, Garg V, Reddy R. Endoscopic management of liver abscess with biliary communication. Dig Dis Sci. 2012; 57:524–527.
Article15. Ghosh S, Sharma S, Gadpayle AK, et al. Clinical, laboratory, and management profile in patients of liver abscess from northern India. J Trop Med. 2014; 2014:142382.
Article16. Santini L, Conzo G, Giordano A, Caracò C, Candela G. Uncommon left hepatic duct injury during laparoscopic cholecystectomy. Surg Laparosc Endosc Percutan Tech. 2000; 10:89–92.
Article17. Lillemoe KD, Melton GB, Cameron JL, et al. Postoperative bile duct strictures: management and outcome in the 1990s. Ann Surg. 2000; 232:430–441.
Article18. Kochar B, Akshintala VS, Afghani E, et al. Incidence, severity, and mortality of post-ERCP pancreatitis: a systematic review by using randomized, controlled trials. Gastrointest Endosc. 2015; 81:143–149.e9.
Article19. Pawar V, Sonthalia N, Pawar S, Surude R, Contractor Q, Rathi P. Successful endoscopic management of bile leak: a single-center experience. Journal of Digestive Endoscopy. 2017; 8:170–175.
Article20. Tuxun T, Zhang JH, Zhao JM, et al. World review of laparoscopic treatment of liver cystic echinococcosis--914 patients. Int J Infect Dis. 2014; 24:43–50.
Article21. El-Gendi AM, El-Shafei M, Bedewy E. The role of prophylactic endoscopic sphincterotomy for prevention of postoperative bile leak in hydatid liver disease: a randomized controlled study. J Laparoendosc Adv Surg Tech A. 2018; 28:990–996.
Article22. Sharma BC, Reddy RS, Garg V. Endoscopic management of hepatic hydatid cyst with biliary communication. Dig Endosc. 2012; 24:267–270.
Article23. Adler DG, Papachristou GI, Taylor LJ, et al. Clinical outcomes in patients with bile leaks treated via ERCP with regard to the timing of ERCP: a large multicenter study. Gastrointest Endosc. 2017; 85:766–772.
Article24. Yun SU, Cheon YK, Shim CS, et al. The outcome of endoscopic management of bile leakage after hepatobiliary surgery. Korean J Intern Med. 2017; 32:79–84.
Article25. Alila M, Bourakkadi Idrissi M, Dkhissi Y, Benjelloun E. Endoscopic management of biliobronchial fistulas. J Lung Pulm Respir Res. 2017; 4:00150.
Article26. Mukkada RJ, Antony R, Francis JV, et al. Bronchobiliary fistula treated successfully with endoscopic microcoils and glue. Ann Thorac Surg. 2014; 98:e33–e34.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endoscopic Management of Bile Leakage after Cholecystectomy: A Single-Center Experience for 12 Years
- Endoscopic Nasobiliary Drainage for Bile Leak Caused by Injury to the Ducts of Luschka
- The Causes and Endoscopic Management of Bile Leak
- A Case of Bile Leak from the Accessory Bile Duct after Laparoscopic Cholecystectomy
- Endoscopic Management of Bile Leakage after Liver Transplantation