J Cerebrovasc Endovasc Neurosurg.
2020 Dec;22(4):225-236. 10.7461/jcen.2020.E2020.06.005.
Result of coiling versus clipping of unruptured anterior communicating artery aneurysms treated by a hybrid vascular neurosurgeon
- Affiliations
-
- 1Department of Neurosurgery, Medical Research Institute, Pusan National University Hospital, Busan, Korea
- 2Diagnostic Radiology, Medical Research Institute, Pusan National University Hospital, Busan, Korea
- KMID: 2511036
- DOI: http://doi.org/10.7461/jcen.2020.E2020.06.005
Abstract
Objective
This study will evaluate the outcomes of coiling versus clipping of unruptured anterior communicating artery (A-com) aneurysms treated by a hybrid vascular neurosurgeon to suggest the best protocol of management for these conditions.
Methods
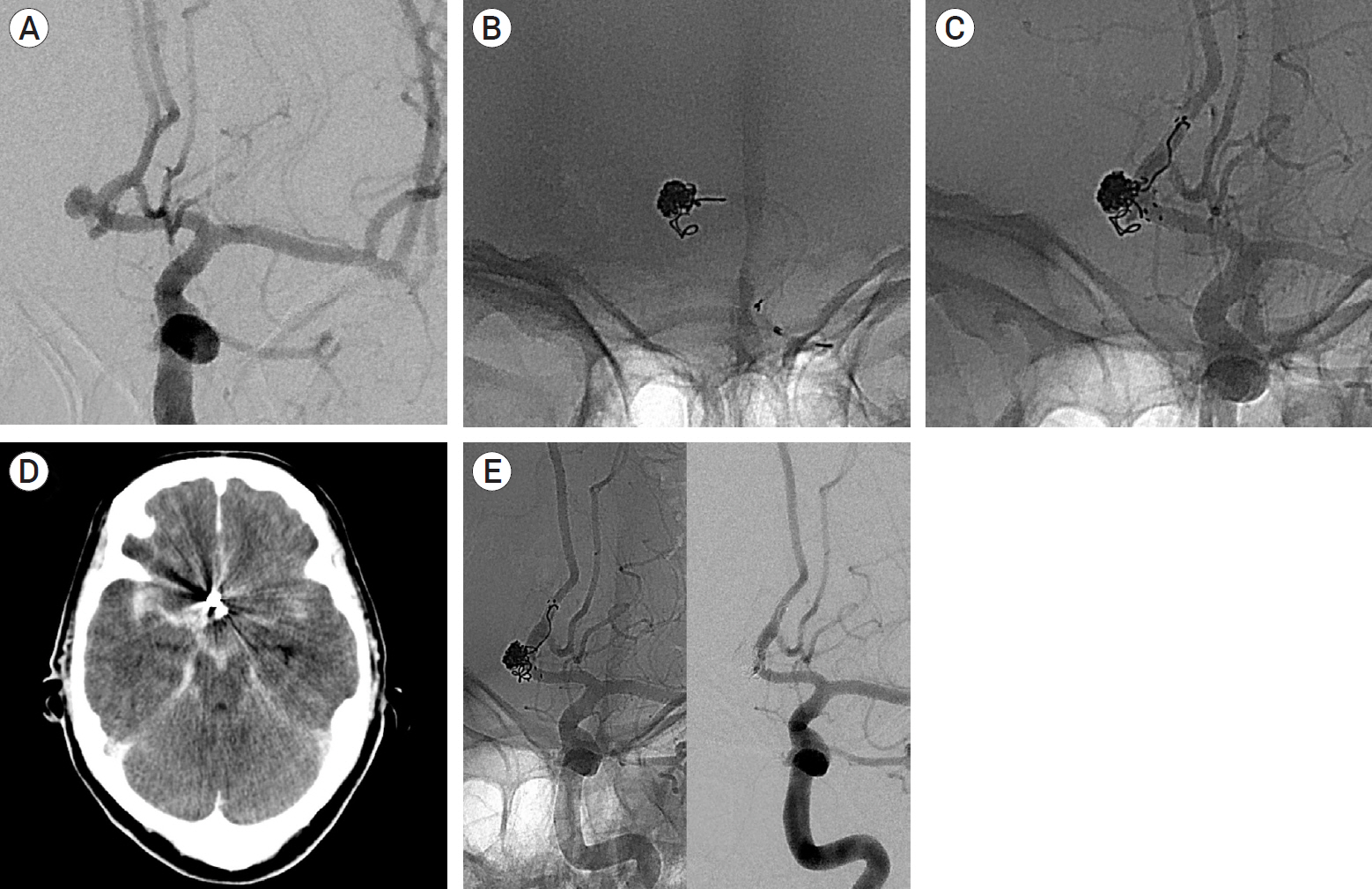
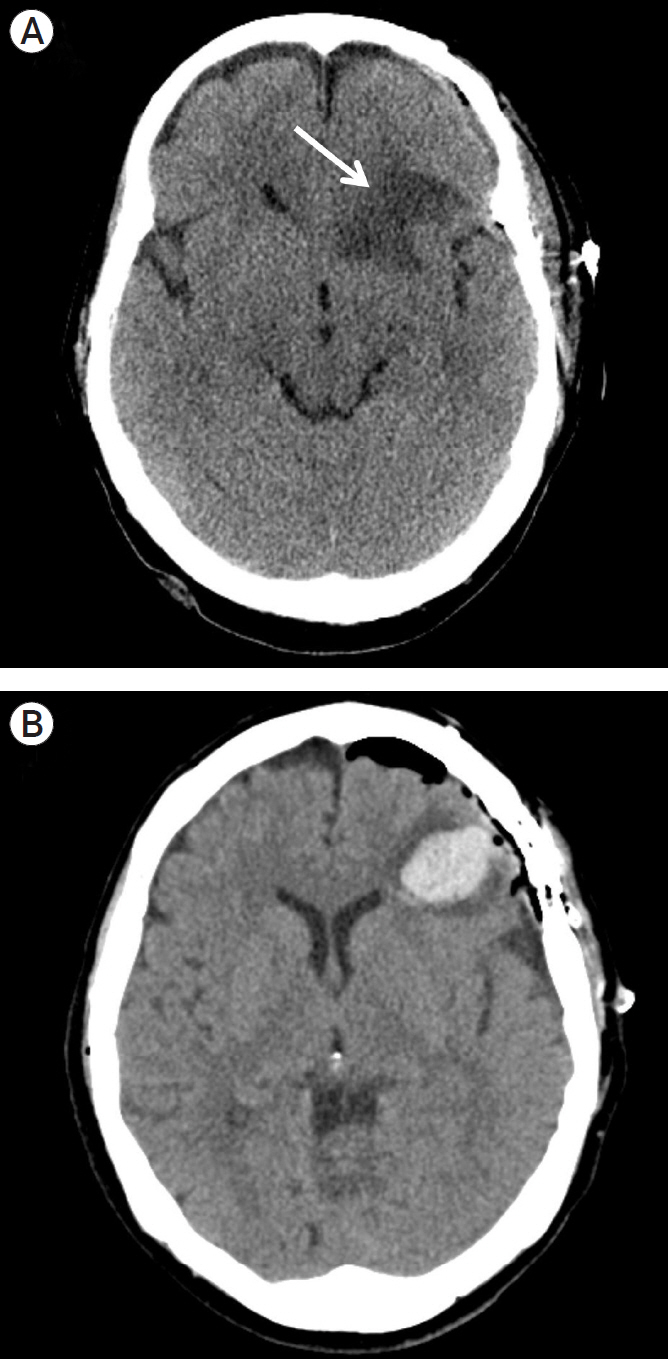
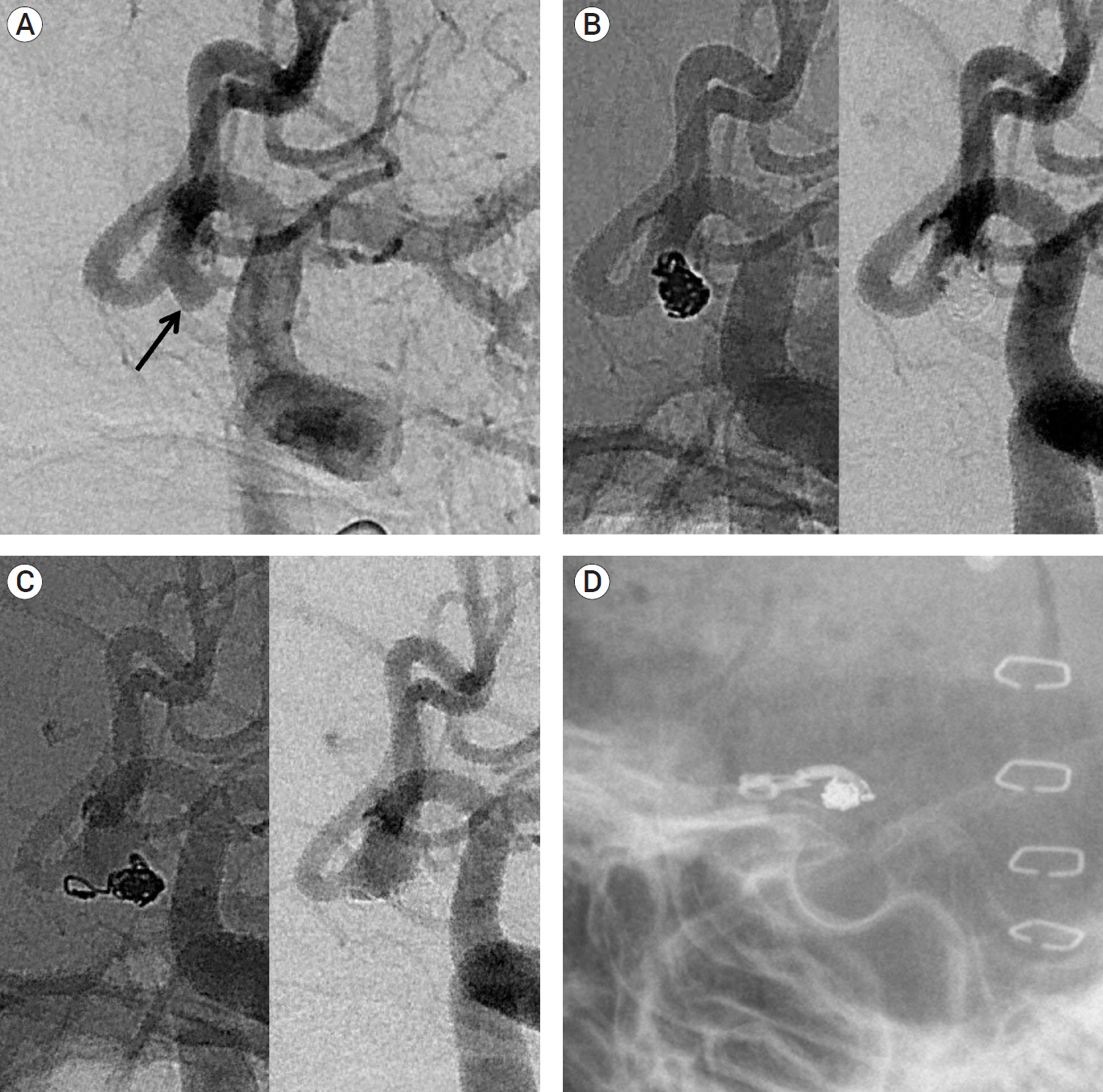
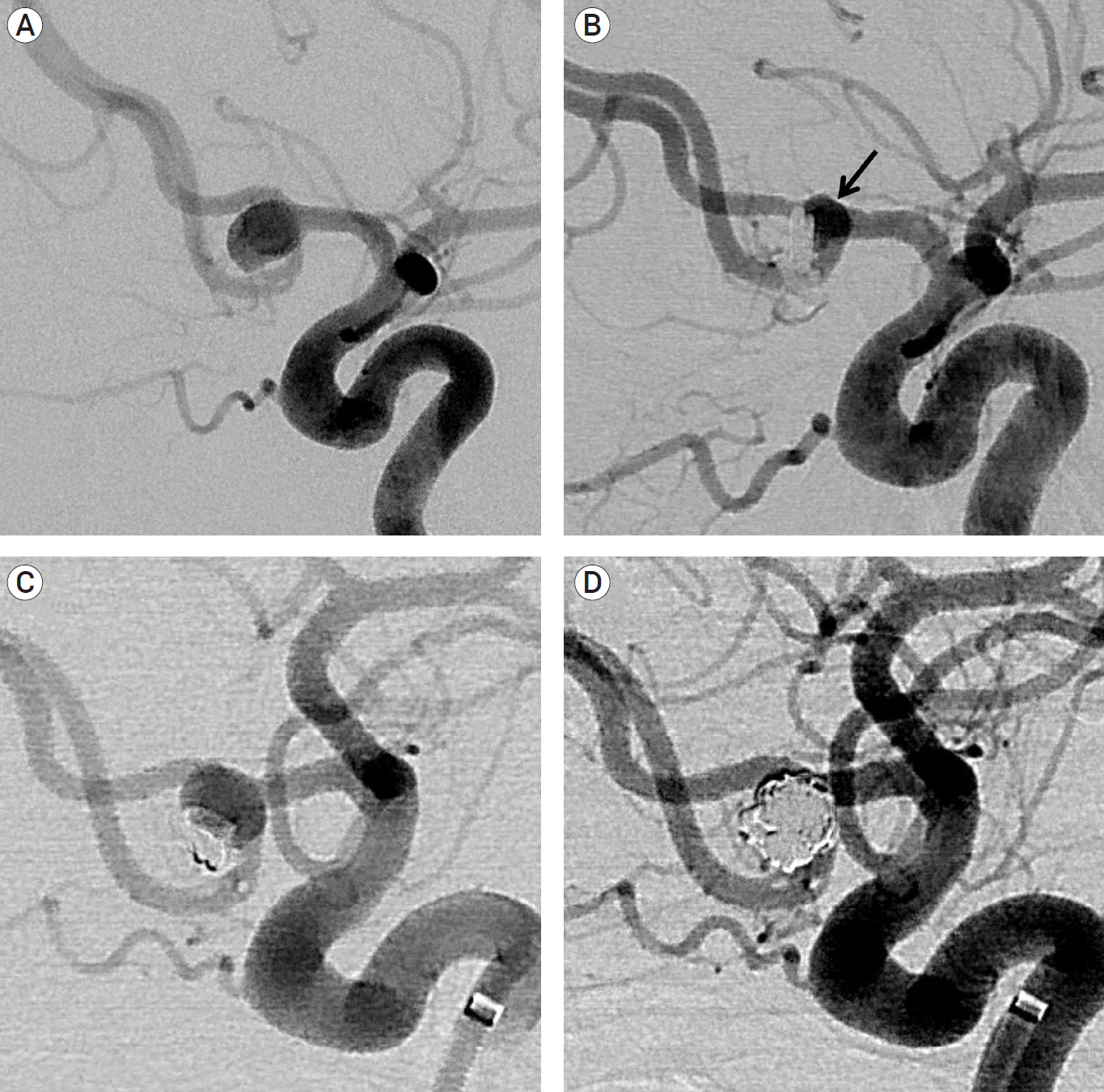
We retrospectively reviewed the records of 70 patients with an unruptured A-com aneurysm treated with coiling or clipping performed by a hybrid vascular neurosurgeon between March 2012 and December 2019. The patients were dichotomized, into the coil group or clip group. Treatment-related complications, clinical and radiological results were evaluated.
Results
Of the 70 patients identified, 37 underwent coiling and 33 clipping. Procedure-related symptomatic complications occurred in 2 patients (5.4%) in the coil group and 3 patients (9.1%) in the clip group. Poor clinical outcome (modified Rankin Scale [mRS] of 3 to 6) at 6 months of follow-up was seen in only one patient (2.7%) for the coil group, and none for the clip group. The one poor outcome was the result of intra-procedural rupture during coiling. Follow-up conventional angiography data (mean duration, 15.0 months) revealed that the major recanalization rate is 5.6% for the coil group and 10.0% for the clip group.
Conclusions
Management of A-com aneurysms requires more collaboration between microsurgical clipping and endovascular therapy. Evaluation of patient and aneurysm characteristics by considering the advantages and disadvantages of both techniques could provide an optimal treatment modality. A hybrid vascular neurosurgeon is expected to be a proper solution for the management of these conditions.
Keyword
Figure
Cited by 1 articles
-
Commentary on: Result of coiling versus clipping of unruptured anterior communicating artery aneurysms treated by a hybrid vascular neurosurgeon
Jorn Van Der Veken
J Cerebrovasc Endovasc Neurosurg. 2021;23(2):169-171. doi: 10.7461/jcen.2021.E2020.10.008.
Reference
-
1. Beeckmans K, Crunelle CL, Van den Bossche J, Dierckx E, Michiels K, Vancoillie P, et al. Cognitive outcome after surgical clipping versus endovascular coiling in patients with subarachnoid hemorrhage due to ruptured anterior communicating artery aneurysm. Acta Neurol Belg. 2020; Feb. 120(1):123–32.
Article2. Birknes JK, Hwang SK, Pandey AS, Cockroft K, Dyer AM, Benitez RP, et al. Feasibility and limitations of endovascular coil embolization of anterior communicating artery aneurysms: morphological considerations. Neurosurgery. 2006; Jul. 59(1):43–52. discussion 43-52.
Article3. Cherian MP, Pranesh MB, Mehta P, Vijayan K, Baskar P, Kalyanpur TM, et al. Outcomes of endovascular coiling of anterior communicating artery aneurysms in the early post-rupture period: a prospective analysis. Neurol India. 2011; Mar-Apr. 59(2):218–23.
Article4. Fang S, Brinjikji W, Murad MH, Kallmes DF, Cloft HJ, Lanzino G. Endovascular treatment of anterior communicating artery aneurysms: a systematic review and meta-analysis. AJNR Am J Neuroradiol. 2014; May. 35(5):943–7.
Article5. Finitsis S, Anxionnat R, Lebedinsky A, Albuquerque PC, Clayton MF, Picard L, et al. Endovascular treatment of ACom intracranial aneurysms. Report on series of 280 patients. Interv Neuroradiol. 2010; Mar. 16(1):7–16.6. Guglielmi G, Vinuela F, Duckwiler G, Jahan R, Cotroneo E, Gigli R. Endovascular treatment of 306 anterior communicating artery aneurysms: overall, perioperative results. J Neurosurg. 2009; May. 110(5):874–9.
Article7. Hernesniemi J, Dashti R, Lehecka M, Niemela M, Rinne J, Lehto H, et al. Microneurosurgical management of anterior communicating artery aneurysms. Surg Neurol. 2008; Jul. 70(1):8–28. discussion 29.
Article8. Kassell NF, Torner JC, Haley EC Jr, Jane JA, Adams HP, Kongable GL. The International Cooperative Study on the Timing of Aneurysm Surgery. Part 1: Overall management results. J Neurosurg. 1990; Jul. 73(1):18–36.9. Lai LT, Gragnaniello C, Morgan MK. Outcomes for a case series of unruptured anterior communicating artery aneurysm surgery. J Clin Nneurosci. 2013; Dec. 20(12):1688–92.
Article10. Mortimer AM, Steinfort B, Faulder K, Erho T, Scherman DB, Rao PJ, et al. Rates of local procedural-related structural injury following clipping or coiling of anterior communicating artery aneurysms. J Neurointerv Surg. 2016; Mar. 8(3):256–64.
Article11. Nathal E, Yasui N, Sampei T, Suzuki A. Intraoperative anatomical studies in patients with aneurysms of the anterior communicating artery complex. J Neurosurg. 1992; Apr. 76(4):629–34.
Article12. O'Neill AH, Chandra RV, Lai LT. Safety and effectiveness of microsurgical clipping, endovascular coiling, and stent assisted coiling for unruptured anterior communicating artery aneurysms: a systematic analysis of observational studies. J Neurointerv Surg. 2017; Aug. 9(8):761–5.13. Onkuma H, Munakata A, Shimamura N. Microsurgical anatomy and standard technique for anterior communicating artery aneurysms. No Shinkei Geka. 2008; Jan. 36(1):27–43.14. Proust F, Debono B, Hannequin D, Gerardin E, Clavier E, Langlois O, et al. Treatment of anterior communicating artery aneurysms: complementary aspects of microsurgical and endovascular procedures. J Neurosurg. 2003; Jul. 99(1):3–14.
Article15. Rhoton AL Jr, Perlmutter D. Microsurgical anatomy of anterior communicating artery aneurysms. Neurol Res. 1980; 2(3-4):217–51.
Article16. Riina HA, Lemole GM Jr, Spetzler RF. Anterior communicating artery aneurysms. Neurosurgery. 2002; Oct. 51(4):993–6. discussion 996.
Article17. Schmalz PGR, Enriquez-Marulanda A, Alturki A, Stapleton CJ, Thomas AJ, Ogilvy CS. Combined outcomes of endovascular or surgical treatment of unruptured anterior communicating artery aneurysms: is a more aggressive management strategy warranted? World Neurosurg. 2018; Jul. 115:e331–6.18. Zanaty M, Chalouhi N, Starke RM, Daou B, Todd M, Bayman E, et al. Short-term outcome of clipping versus coiling of ruptured intracranial aneurysms treated by dual-trained cerebrovascular surgeon: single-institution experience. World Neurosurg. 2016; Nov. 95:262–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Commentary on: Result of coiling versus clipping of unruptured anterior communicating artery aneurysms treated by a hybrid vascular neurosurgeon
- ERRATUM: Result of coiling versus clipping of unruptured anterior communicating artery aneurysms treated by a hybrid vascular neurosurgeon
- Seven Intracranial Aneurysms in One Patient: Treatment and Review of Literature
- Microsurgical anatomy of the Anterior Cerebral-anterior Communicating Artery
- Comprehension of Two Modalities: Endovascular Coiling and Microsurgical Clipping in Treatment of Intracranial Aneurysms