J Korean Neurosurg Soc.
2021 Jan;64(1):39-50. 10.3340/jkns.2020.0028.
Clinical Outcomes of Large (>10 mm) Unruptured Posterior Circulation Aneurysms and Their Predictors
- Affiliations
-
- 1Department of Neurosurgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2510758
- DOI: http://doi.org/10.3340/jkns.2020.0028
Abstract
Objective
: The treatment of large aneurysms of the posterior circulation is complicated and remains challenging. We here analyzed our institutional clinical outcomes of large unruptured aneurysms of the posterior circulation.
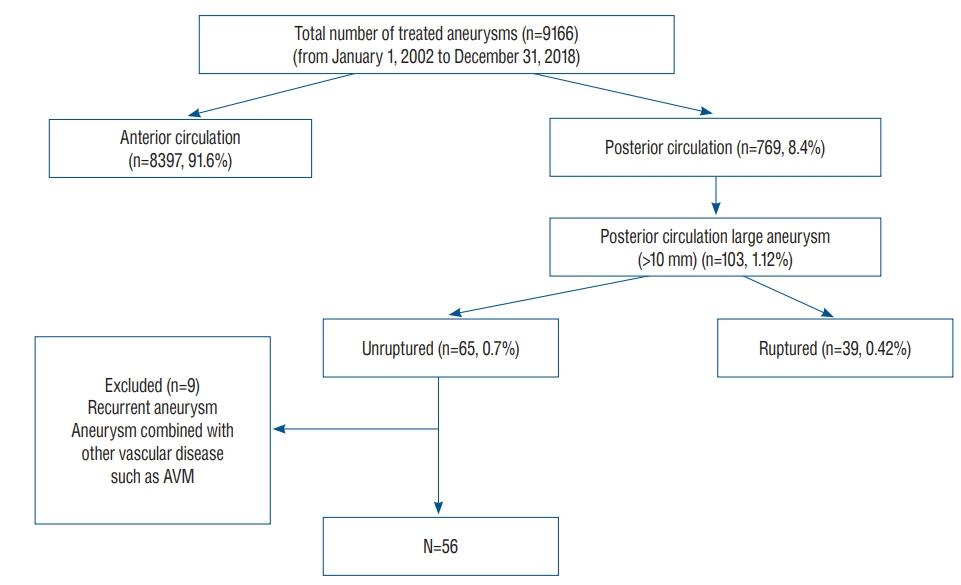
Methods
: This study included 56 patients who presented with a large (>10 mm) unruptured aneurysm of the posterior circulation between 2002 and 2018.
Results
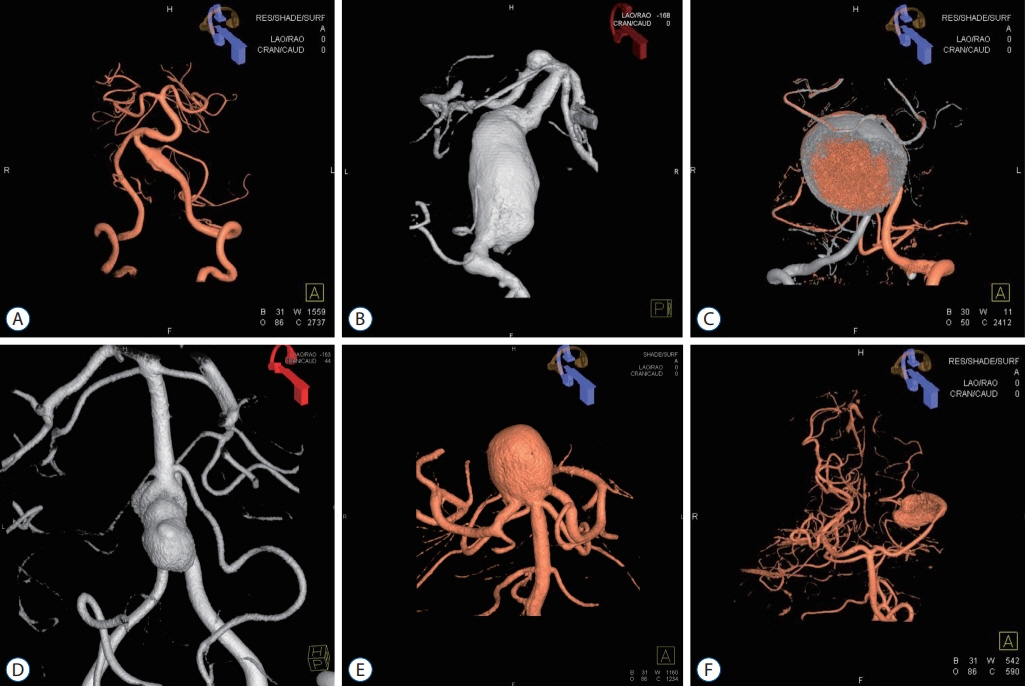
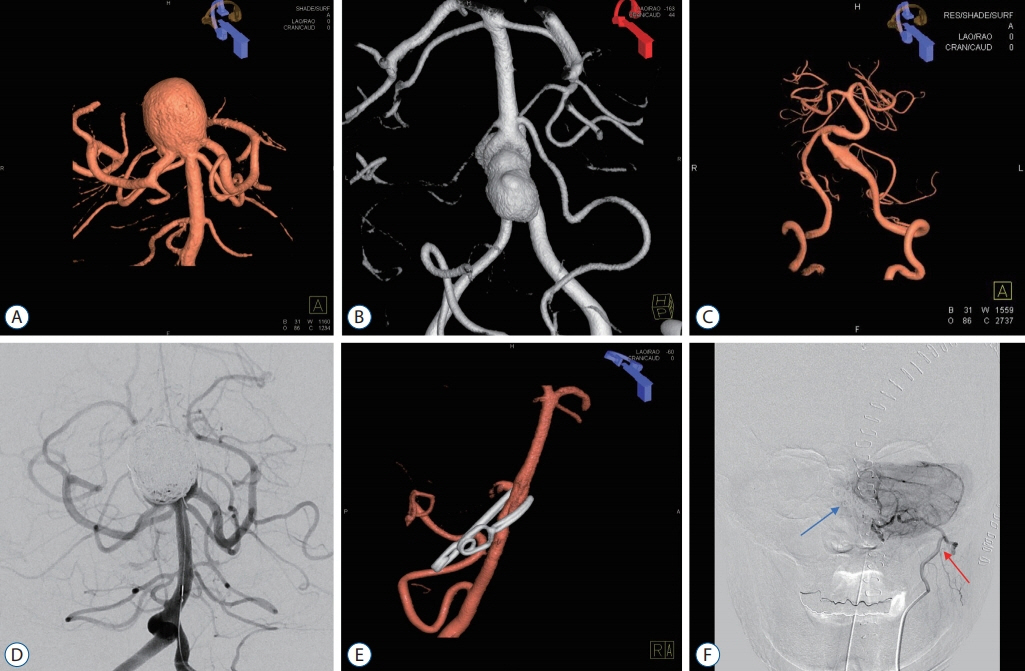
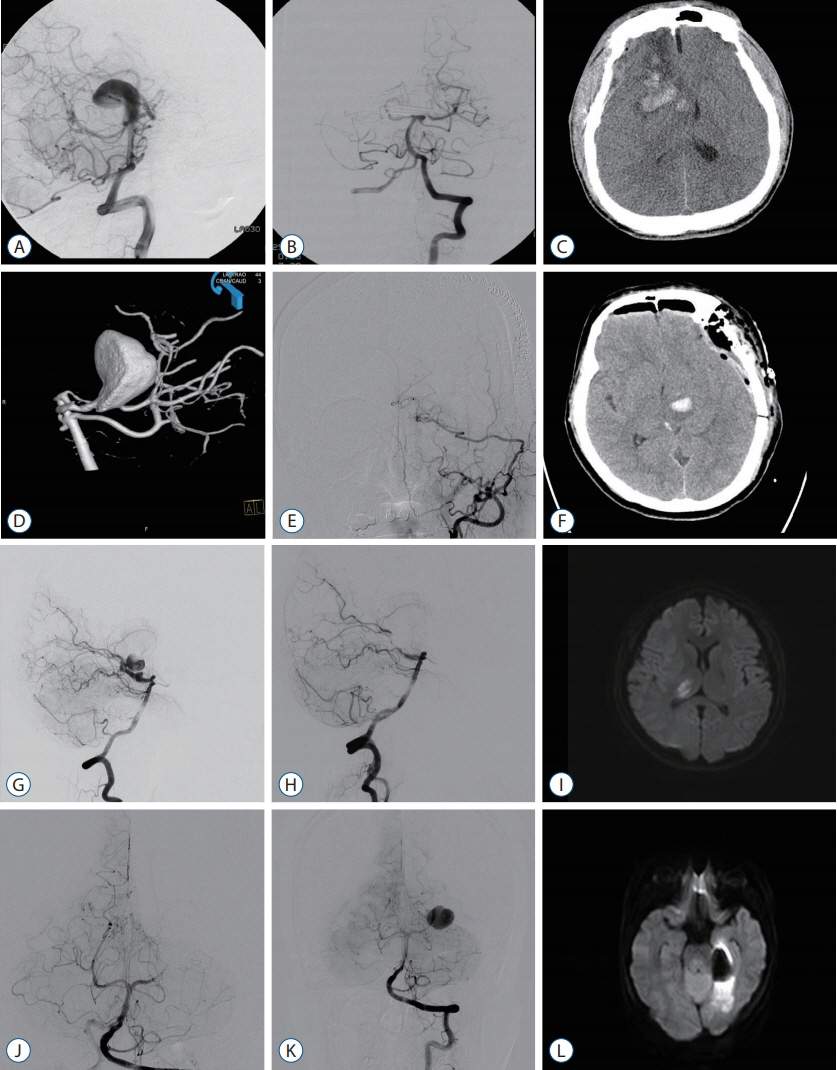
: There were 18 (32.1%) male and 38 (67.9%) female patients, with a mean age of 53.4 years. The most common location was the vertebral artery, followed by the basilar tip and posterior cerebral artery. The median follow-up duration was 29 months. Eighteen patients (32.1%) were treated by transcranial surgery and 38 (67.9%) were treated by endovascular treatment (EVT). Posttreatment complications occurred in 16 patients (28.6%), with there being no significant difference between the transcranial surgery and EVT groups. Complete obliteration was achieved in 30 patients (53.6%), with there being no statistically significant difference between the transcranial surgery and EVT groups. Recurrence occurred in 17 patients (30.4%), and the rate of recurrence was higher in the EVT group than in the transcranial surgery group (39.5% vs. 11.1%, p=0.03). Forty-four (84%) of 56 patients showed a favorable functional outcome. In saccular aneurysm, EVT was negative predictor of worsening of functional status.
Conclusion
: Treatment of these aneurysms harbors an inherent high risk of morbidity. No superiority was found between transcranial surgery and EVT in terms of complications and complete obliteration, but transcranial surgery showed a higher treatment durability than EVT.
Keyword
Figure
Reference
-
References
1. Ban VS, El Ahmadieh TY, Aoun SG, Plitt AR, Lyon KA, Eddleman C, et al. Prediction of outcomes for ruptured aneurysm surgery: the Southwestern aneurysm severity index. Stroke. 50:595–601. 2019.
Article2. Besser M, Khurana VG. Management of giant intracranial aneurysms of the posterior circulation. J Clin Neurosci. 5:161–168. 1998.
Article3. Bhogal P, Pérez MA, Ganslandt O, Bäzner H, Henkes H, Fischer S. Treatment of posterior circulation non-saccular aneurysms with flow diverters: a single-center experience and review of 56 patients. J Neurointerv Surg. 9:471–481. 2017.
Article4. Cagnazzo F, Mantilla D, Rouchaud A, Brinjikji W, Lefevre PH, Dargazanli C, et al. Endovascular treatment of very large and giant intracranial aneurysms: comparison between reconstructive and deconstructive techniques-a meta-analysis. AJNR Am J Neuroradiol. 39:852–858. 2018.
Article5. Chua MH, Griessenauer CJ, Stapleton CJ, He L, Thomas AJ, Ogilvy CS. Documentation of improved outcomes for intracranial aneurysm management over a 15-year interval. Stroke. 47:708–712. 2016.
Article6. Eller JL, Dumont TM, Mokin M, Sorkin GC, Levy EI, Snyder KV, et al. Endovascular treatment of posterior circulation aneurysms. Neurol Res. 36:339–343. 2014.
Article7. International Study of Unruptured Intracranial Aneurysms Investigators. Unruptured intracranial aneurysms--risk of rupture and risks of surgical intervention. N Engl J Med. 339:1725–1733. 1998.8. Lee SH, Ahn JS, Kwun BD, Park W, Park JC, Roh SW. Surgical flow alteration for the treatment of intracranial aneurysms that are unclippable, untrappable, and uncoilable. J Korean Neurosurg Soc. 58:518–527. 2015.
Article9. Lempert TE, Malek AM, Halbach VV, Phatouros CC, Meyers PM, Dowd CF, et al. Endovascular treatment of ruptured posterior circulation cerebral aneurysms. Clinical and angiographic outcomes. Stroke. 31:100–110. 2000.
Article10. Ng P, Khangure MS, Phatouros CC, Bynevelt M, ApSimon H, McAuliffe W. Endovascular treatment of intracranial aneurysms with guglielmi detachable coils: analysis of midterm angiographic and clinical outcomes. Stroke. 33:210–217. 2002.
Article11. Park JH, Kim YI, Lim YC. Clinical outcomes of treatment for intracranial aneurysm in elderly patients. J Cerebrovasc Endovasc Neurosurg. 16:193–199. 2014.
Article12. Tsianaka E, Al-Shawish A, Potapov A, Fountas K, Spyrou M, Konovalov N. Clipping versus coiling in posterior circulation intracranial aneurysms: a meta-analysis. Chin Neurosurg J. 5:1. 2019.
Article13. Zhao J, Wang S, Yang L, Zhao Y. Clinical experience of 153 patients with posterior circulation aneurysms. J Clin Neurosci. 12:17–20. 2005.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Unruptured Aneurysms-Endovascular Treatment
- What Is the Significance of a Large Number of Ruptured Aneurysms Smaller than 7 mm in Diameter?
- The Merits of Endovascular Coil Surgery for Patients with Unruptured Intracranial Aneurysms
- Surgical Treatment of Unruptured Cerebral Aneurysms
- Management Outcome and Clinical Manifestation of Posterior Circulation Aneurysms VS. Anterior Circulation Aneurysm