Acute Crit Care.
2020 Nov;35(4):263-270. 10.4266/acc.2020.00444.
Experience of percutaneous tracheostomy in critically ill COVID-19 patients
- Affiliations
-
- 1Department of Internal Medicine, Daegu Catholic University Medical Center, Daegu Catholic University School of Medicine, Daegu, Korea
- 2Department of Laboratory Medicine, Daegu Catholic University Medical Center, Daegu Catholic University School of Medicine, Daegu, Korea
- KMID: 2510545
- DOI: http://doi.org/10.4266/acc.2020.00444
Abstract
- Background
Coronavirus disease 2019 (COVID-19) is a highly contagious disease that causes respiratory failure. Tracheostomy is an essential procedure in critically ill COVID-19 patients; however, it is an aerosol-generating technique and thus carries the risk of infection transmission. We report our experience with percutaneous tracheostomy and its safety in a real medical setting.
Methods
During the COVID-19 outbreak, 13 critically ill patients were admitted to the intensive care unit (ICU) at Daegu Catholic University Medical Center between February 24 and April 30, 2020. Seven of these patients underwent percutaneous tracheostomy using Ciaglia Blue Rhino. The medical environment, percutaneous tracheostomy method, and COVID-19 reverse transcriptase-polymerase chain reaction (RT-PCR) results were retrospectively reviewed. After treatment, the COVID-19 infection status of healthcare personnel was investigated by RT-PCR.
Results
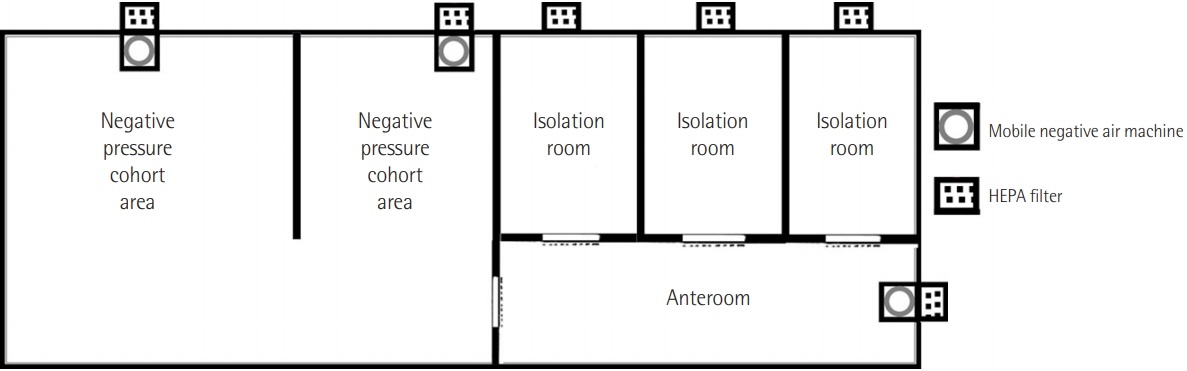
The ICU contained negative pressure cohort areas and isolation rooms, and healthcare personnel wore a powered air-purifying respirator system. We performed seven cases of percutaneous tracheostomy in the same way as in patients without COVID-19. Five patients (71.4%) tested positive for COVID-19 by RT-PCR at the time of tracheostomy. The median cycle threshold value for the RNA-dependent RNA polymerase was 30.60 (interquartile range [IQR], 25.50–36.56) in the upper respiratory tract and 35.04 (IQR, 28.40–36.74) in the lower respiratory tract. All healthcare personnel tested negative for COVID-19 by RT-PCR.
Conclusions
Percutaneous tracheostomy was performed with conventional methods in the negative pressure cohort area. It was safe to perform percutaneous tracheostomy in an environment of COVID-19 infection.
Figure
Reference
-
1. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020; 395:497–506.
Article2. Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020; 395:507–13.
Article3. Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020; 323:1061–9.
Article4. Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020; 382:1708–20.
Article5. Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020; 395:1054–62.
Article6. Li X, Ma X. Acute respiratory failure in COVID-19: is it “typical” ARDS? Crit Care. 2020; 24:198.
Article7. Tay JK, Khoo ML, Loh WS. Surgical considerations for tracheostomy during the COVID-19 pandemic: lessons learned from the severe acute respiratory syndrome outbreak. JAMA Otolaryngol Head Neck Surg. 2020; 146:517–8.8. McGrath BA, Brenner MJ, Warrillow SJ, Pandian V, Arora A, Cameron TS, et al. Tracheostomy in the COVID-19 era: global and multidisciplinary guidance. Lancet Respir Med. 2020; 8:717–25.
Article9. Ahmed N, Hare GM, Merkley J, Devlin R, Baker A. Open tracheostomy in a suspect severe acute respiratory syndrome (SARS) patient: brief technical communication. Can J Surg. 2005; 48:68–71.10. Kwan A, Fok WG, Law KI, Lam SH. Tracheostomy in a patient with severe acute respiratory syndrome. Br J Anaesth. 2004; 92:280–2.
Article11. Wei WI, Tuen HH, Ng RW, Lam LK. Safe tracheostomy for patients with severe acute respiratory syndrome. Laryngoscope. 2003; 113:1777–9.
Article12. Song JH, Kim HC, Kang JG, Roh DH. Tracheotomy in Middle East respiratory syndrome: report of a case. J Clin Otolaryngol. 2015; 26:301–6.13. Takhar A, Walker A, Tricklebank S, Wyncoll D, Hart N, Jacob T, et al. Recommendation of a practical guideline for safe tracheostomy during the COVID-19 pandemic. Eur Arch Otorhinolaryngol. 2020; 277:2173–84.
Article14. Parker NP, Schiff BA, Fritz MA, Rapoport SK, Schild S, Altman KW, et al. AAO position statement: tracheotomy recommendations during the COVID-19 pandemic [Internet]. Alexandria (VA): American Academy of Otolaryngology-Head and Neck Surgery;2020. [cited 2020 Oct 15]. Available from: https://www.entnet.org/content/aao-position-statement-tracheotomy-recommendations-during-covid-19-pandemic.15. Engels PT, Weitzel E, Witterick IJ, Khalili S, Corsten M, Tewfik MA, et al. Recommendations from the CSO-HNS taskforce on performance of tracheotomy during the COVID-19 pandemic [Internet]. Elora (ON): Canadian Society of Otolaryngology-Head and Neck Surgery;2020. [cited 2020 Oct 15]. Available from: https://www.entcanada.org/wp-content/uploads/COVID-19-Guidelines-CSOHNS-Task-Force-Mar-23-2020.pdf.16. Lee SY, Choi SH, Park JE, Hwang S, Kwon KT. Crucial role of temporary airborne infection isolation rooms in an intensive care unit: containing the COVID-19 outbreak in South Korea. Crit Care. 2020; 24:238.
Article17. Ambesh SP, Pandey CK, Srivastava S, Agarwal A, Singh DK. Percutaneous tracheostomy with single dilatation technique: a prospective, randomized comparison of Ciaglia blue rhino versus Griggs’ guidewire dilating forceps. Anesth Analg. 2002; 95:1739–45.
Article18. Zhang X, Huang Q, Niu X, Zhou T, Xie Z, Zhong Y, et al. Safe and effective management of tracheostomy in COVID-19 patients. Head Neck. 2020; 42:1374–81.19. Angel L, Kon ZN, Chang SH, Rafeq S, Palasamudram Shekar S, Mitzman B, et al. Novel percutaneous tracheostomy for critically ill patients with COVID-19. Ann Thorac Surg. 2020; 110:1006–11.
Article20. Vargas M, Russo G, Iacovazzo C, Servillo G. Modified percutaneous tracheostomy in COVID-19 critically ill patients. Head Neck. 2020; 42:1363–6.21. Al Yaghchi C, Ferguson C, Sandhu G. Percutaneous tracheostomy in patients with COVID-19: sealing the bronchoscope with an in-line suction sheath. Br J Anaesth. 2020; 125:e185–6.
Article22. Heikkinen M, Aarnio P, Hannukainen J. Percutaneous dilational tracheostomy or conventional surgical tracheostomy? Crit Care Med. 2000; 28:1399–402.
Article23. Dulguerov P, Gysin C, Perneger TV, Chevrolet JC. Percutaneous or surgical tracheostomy: a meta-analysis. Crit Care Med. 1999; 27:1617–25.24. Pauliny M, Christova E, Mackova J, Liska M. Percutaneous dilation tracheostomy versus surgical tracheostomy in critically ill patients. Bratisl Lek Listy. 2012; 113:409–11.
Article25. Salna M, Tipograf Y, Liou P, Chicotka S, Biscotti M 3rd, Agerstrand C, et al. tracheostomy is safe during extracorporeal membrane oxygenation support. ASAIO J. 2020; 66:652–6.
Article26. Dimopoulos S, Joyce H, Camporota L, Glover G, Ioannou N, Langrish CJ, et al. Safety of percutaneous dilatational tracheostomy during veno-venous extracorporeal membrane oxygenation support in adults with severe respiratory failure. Crit Care Med. 2019; 47:e81–8.
Article27. Han MS, Byun JH, Cho Y, Rim JH. RT-PCR for SARS-CoV-2: quantitative versus qualitative. Lancet Infect Dis. 2020; May. 20. [Epub]. https://doi.org/10.1016/S1473-3099(20)30424-2.
Article28. Fang Y, Zhang H, Xie J, Lin M, Ying L, Pang P, et al. Sensitivity of chest CT for COVID-19: comparison to RT-PCR. Radiology. 2020; 296:E115–7.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Percutaneous Dilatational Tracheostomy
- Ultrasound-Guided Percutaneous Dilatational Tracheostomy for Critically Ill Patients With COVID-19
- Experience of Treating Critically Ill COVID-19 Patients in Daegu, South Korea
- How We Have Treated Severe to Critically Ill Patients With Coronavirus Disease 2019 in Korea
- Characteristics of Critically Ill COVID-19 Patients in Busan, Republic of Korea