J Korean Med Sci.
2021 Jan;36(1):e11. 10.3346/jkms.2021.36.e11.
Pediatric Emergency Department Utilization and Coronavirus Disease in Daegu, Korea
- Affiliations
-
- 1Department of Pediatrics, Yeungnam University School of Medicine, Yeungnam University Hospital, Daegu, Korea
- 2Department of Pediatrics, Keimyung University School of Medicine, Daegu, Korea
- 3Department of Emergency Medicine, School of Medicine, Daegu Catholic University, Daegu, Korea
- 4Department of Pediatrics, School of Medicine, Kyungpook National University, Daegu, Korea
- 5Department of Pediatrics, Daegu Fatima Hospital, Korea
- 6Department of Emergency Medicine, School of Medicine, Kyungpook National University, Daegu, Korea
- KMID: 2510379
- DOI: http://doi.org/10.3346/jkms.2021.36.e11
Abstract
- Background
Limited data exist on children's utilization of the emergency department (ED) in the ongoing coronavirus disease 2019 (COVID-19) pandemic. Thus, we aimed to examine ED utilization among pediatric patients and the impact of COVID-19 in one large city affected by the outbreak.
Methods
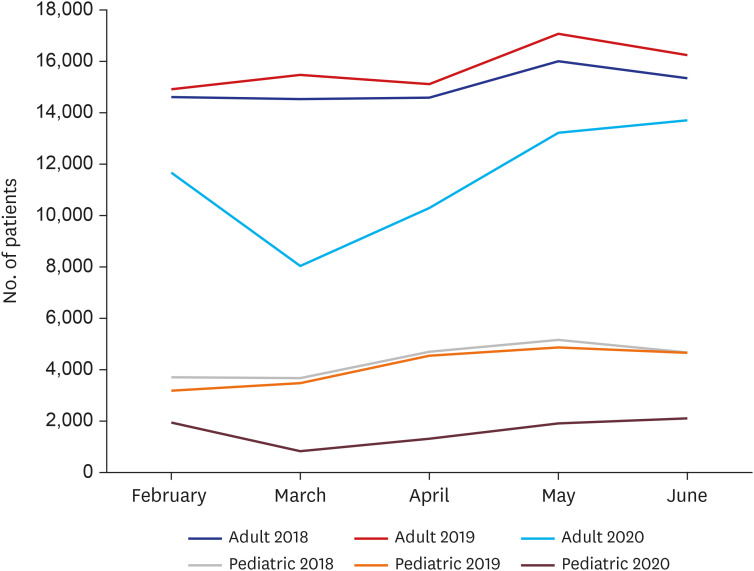
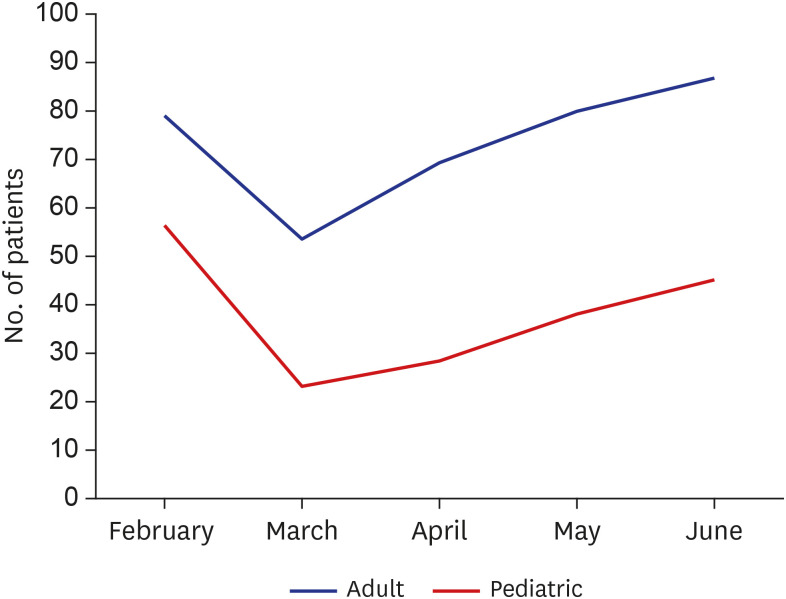
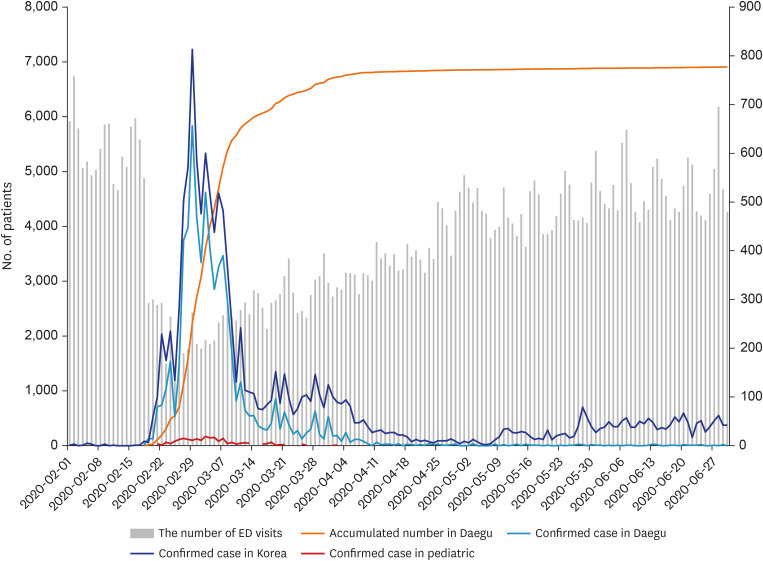
This retrospective study included data from six EDs in Daegu, Korea. We compared the demographic and clinical data of patients presenting to the ED during the COVID-19 pandemic (February 1st–June 30th 2020) with those of patients who visited the ED in this period during 2018 and 2019.
Results
Fewer patients, particularly children visited the EDs during the study period in 2020 than those in the previous (2018/2019) year period: the number of adult patient decreased by 46.4% and children by 76.9%. Although the number of patients increased from the lowest point of the decrease in March 2020, the number of pediatric patients visiting the ED remained less than half (45.2%) in June 2020 compared with that of previous years. The proportion of patients with severe conditions increased in adults, infants, and school-aged children, and consequently resulted in increased ambulance use and higher hospitalization rates. Fewer infants and young children but more school-aged children visited the ED with febrile illnesses in 2020 than in 2018/2019.
Conclusion
The COVID-19 pandemic has led to a substantial decrease in pediatric ED utilization. These findings can help reallocate human and material resources in the EDs during infectious disease outbreaks.
Figure
Cited by 1 articles
-
Long-term impact of coronavirus disease 2019 pandemic on emergency department utilization in a metropolitan emergency department in Korea
Seung Yeon Hwang, Jae Kwang Lee, Hyun Sik Ryu, Seong Soo Park, Jun Young Choi, Hye Ji Lee, Seung Ho Hur, Yeong Geun Park, Hyun Soo Choi
Pediatr Emerg Med J. 2021;8(2):57-65. doi: 10.22470/pemj.2021.00346.
Reference
-
1. Li H, Liu SM, Yu XH, Tang SL, Tang CK. Coronavirus disease 2019 (COVID-19): current status and future perspectives. Int J Antimicrob Agents. 2020; 55(5):105951. PMID: 32234466.
Article2. Cao Y, Cai K, Xiong L. Coronavirus disease 2019: a new severe acute respiratory syndrome from Wuhan in China. Acta Virol. 2020; 64(2):245–250. PMID: 32551792.
Article3. Vaishya R, Javaid M, Khan IH, Haleem A. Artificial intelligence (AI) applications for COVID-19 pandemic. Diabetes Metab Syndr. 2020; 14(4):337–339. PMID: 32305024.
Article4. Wosik J, Fudim M, Cameron B, Gellad ZF, Cho A, Phinney D, et al. Telehealth transformation: COVID-19 and the rise of virtual care. J Am Med Inform Assoc. 2020; 27(6):957–962. PMID: 32311034.
Article5. Fagbuyi DB, Brown KM, Mathison DJ, Kingsnorth J, Morrison S, Saidinejad M, et al. A rapid medical screening process improves emergency department patient flow during surge associated with novel H1N1 influenza virus. Ann Emerg Med. 2011; 57(1):52–59. PMID: 20947207.
Article6. Lee SY, Khang YH, Lim HK. Impact of the 2015 middle east respiratory syndrome outbreak on emergency care utilization and mortality in South Korea. Yonsei Med J. 2019; 60(8):796–803. PMID: 31347336.
Article7. Lu TH, Chou YJ, Liou CS. Impact of SARS on healthcare utilization by disease categories: implications for delivery of healthcare services. Health Policy. 2007; 83(2-3):375–381. PMID: 17445942.
Article8. Dong Y, Mo X, Hu Y, Qi X, Jiang F, Jiang Z, et al. Epidemiology of COVID-19 among children in China. Pediatrics. 2020; 145(6):e20200702. PMID: 32179660.
Article9. Choi H, Ok JS, An SY. Evaluation of validity of the Korean triage and Acuity Scale. J Korean Acad Nurs. 2019; 49(1):26–35. PMID: 30837440.
Article10. Lazzerini M, Barbi E, Apicella A, Marchetti F, Cardinale F, Trobia G. Delayed access or provision of care in Italy resulting from fear of COVID-19. Lancet Child Adolesc Health. 2020; 4(5):e10–1. PMID: 32278365.
Article11. Iozzi L, Brambilla I, Foiadelli T, Marseglia GL, Ciprandi G. Paediatric emergency department visits fell by more than 70% during the COVID-19 lockdown in Northern Italy. Acta Paediatr. 2020; 109(10):2137–2138. PMID: 32623774.
Article12. Isba R, Edge R, Jenner R, Broughton E, Francis N, Butler J. Where have all the children gone? Decreases in paediatric emergency department attendances at the start of the COVID-19 pandemic of 2020. Arch Dis Child. 2020; 105(7):704.
Article13. Dann L, Fitzsimons J, Gorman KM, Hourihane J, Okafor I. Disappearing act: COVID-19 and paediatric emergency department attendances. Arch Dis Child. 2020; 105(8):810–811. PMID: 32518141.
Article14. Soo RJ, Chiew CJ, Ma S, Pung R, Lee V. Decreased influenza incidence under COVID-19 control measures, Singapore. Emerg Infect Dis. 2020; 26(8):1933–1935. PMID: 32339092.
Article15. Oh MD, Park WB, Park SW, Choe PG, Bang JH, Song KH, et al. Middle East respiratory syndrome: what we learned from the 2015 outbreak in the Republic of Korea. Korean J Intern Med. 2018; 33(2):233–246. PMID: 29506344.
Article16. Chung HS, Lee DE, Kim JK, Yeo IH, Kim C, Park J, et al. Revised triage and surveillance protocols for temporary emergency department closures in tertiary hospitals as a response to COVID-19 crisis in Daegu Metropolitan City. J Korean Med Sci. 2020; 35(19):e189. PMID: 32419401.
Article17. Ferrero F, Ossorio MF, Torres FA, Debaisi G. Impact of the COVID-19 pandemic in the paediatric emergency department attendances in Argentina. Arch Dis Child. Forthcoming 2020. DOI: 10.1136/archdischild-2020-319833.
Article18. Roland D, Harwood R, Bishop N, Hargreaves D, Patel S, Sinha I. Children's emergency presentations during the COVID-19 pandemic. Lancet Child Adolesc Health. 2020; 4(8):e32–3. PMID: 32598871.
Article19. Scaramuzza A, Tagliaferri F, Bonetti L, Soliani M, Morotti F, Bellone S, et al. Changing admission patterns in paediatric emergency departments during the COVID-19 pandemic. Arch Dis Child. 2020; 105(7):704–706.
Article20. Shih FY, Ma MH, Chen SC, Wang HP, Fang CC, Shyu RS, et al. ED overcrowding in Taiwan: facts and strategies. Am J Emerg Med. 1999; 17(2):198–202. PMID: 10102327.
Article21. Andrulis DP, Kellermann A, Hintz EA, Hackman BB, Weslowski VB. Emergency departments and crowding in United States teaching hospitals. Ann Emerg Med. 1991; 20(9):980–986. PMID: 1877784.
Article22. Derlet RW, Richards JR. Overcrowding in the nation's emergency departments: complex causes and disturbing effects. Ann Emerg Med. 2000; 35(1):63–68. PMID: 10613941.
Article23. Richardson DB. Increase in patient mortality at 10 days associated with emergency department overcrowding. Med J Aust. 2006; 184(5):213–216. PMID: 16515430.24. Stang AS, Crotts J, Johnson DW, Hartling L, Guttmann A. Crowding measures associated with the quality of emergency department care: a systematic review. Acad Emerg Med. 2015; 22(6):643–656. PMID: 25996053.
Article25. Carter EJ, Pouch SM, Larson EL. The relationship between emergency department crowding and patient outcomes: a systematic review. J Nurs Scholarsh. 2014; 46(2):106–115. PMID: 24354886.
Article26. Pines JM, Hollander JE, Localio AR, Metlay JP. The association between emergency department crowding and hospital performance on antibiotic timing for pneumonia and percutaneous intervention for myocardial infarction. Acad Emerg Med. 2006; 13(8):873–878. PMID: 16766743.
Article27. Cho SY, Kang JM, Ha YE, Park GE, Lee JY, Ko JH, et al. MERS-CoV outbreak following a single patient exposure in an emergency room in South Korea: an epidemiological outbreak study. Lancet. 2016; 388(10048):994–1001. PMID: 27402381.
Article28. Rondeau KV, Francescutti LH. Emergency department overcrowding: the impact of resource scarcity on physician job satisfaction. J Healthc Manag. 2005; 50(5):327–340. PMID: 16268411.
Article29. Paek SH, Kim DK, Lee JH, Kwak YH. The impact of middle east respiratory syndrome outbreak on trends in emergency department utilization patterns. J Korean Med Sci. 2017; 32(10):1576–1580. PMID: 28875599.
Article30. Hartford EA, Keilman A, Yoshida H, Migita R, Chang T, Enriquez B, et al. Pediatric emergency department responses to COVID-19: transitioning from surge preparation to regional support. Disaster Med Public Health Prep. Forthcoming 2020. DOI: 10.1017/dmp.2020.197.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A potential impact of the donning and doffing policy on emergency department length of stay during the coronavirus disease 2019 pandemic
- Utilization Patterns of Pediatric Emergency Room
- Changes in emergency department utilization by neonates during the coronavirus disease 2019 pandemic: a single-center study in Korea
- The proposed algorithm for emergency endoscopy during the coronavirus disease 2019 outbreak
- Erratum: Correction of Text in the Article “Pediatric Emergency Department Utilization and Coronavirus Disease in Daegu, Korea”