Korean J Transplant.
2020 Dec;34(4):219-230. 10.4285/kjt.20.0040.
Causes of donation failure and improvement measures analyzed based on data from domestic deceased donors in 2019
- Affiliations
-
- 1Korea Organ Donation Agency, Seoul, Korea
- KMID: 2510254
- DOI: http://doi.org/10.4285/kjt.20.0040
Abstract
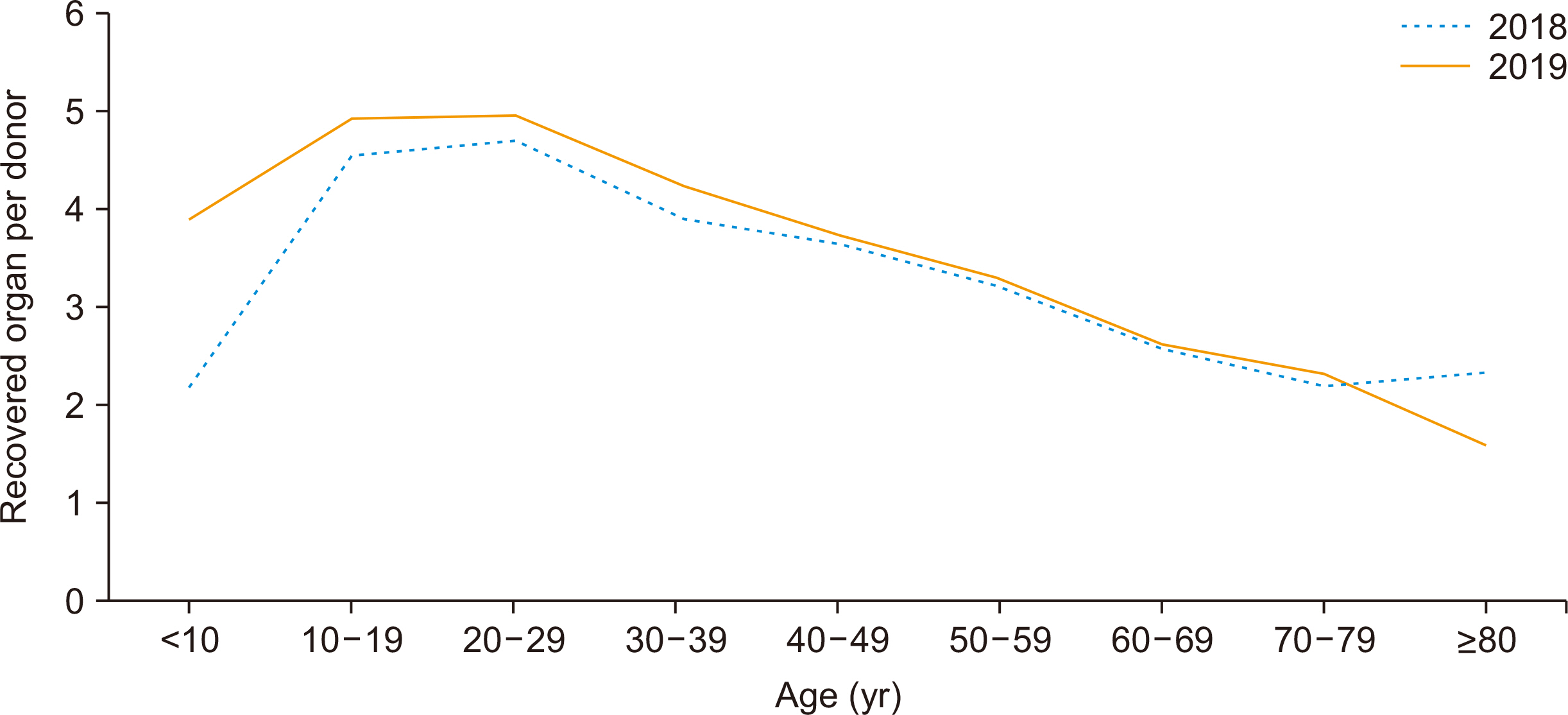
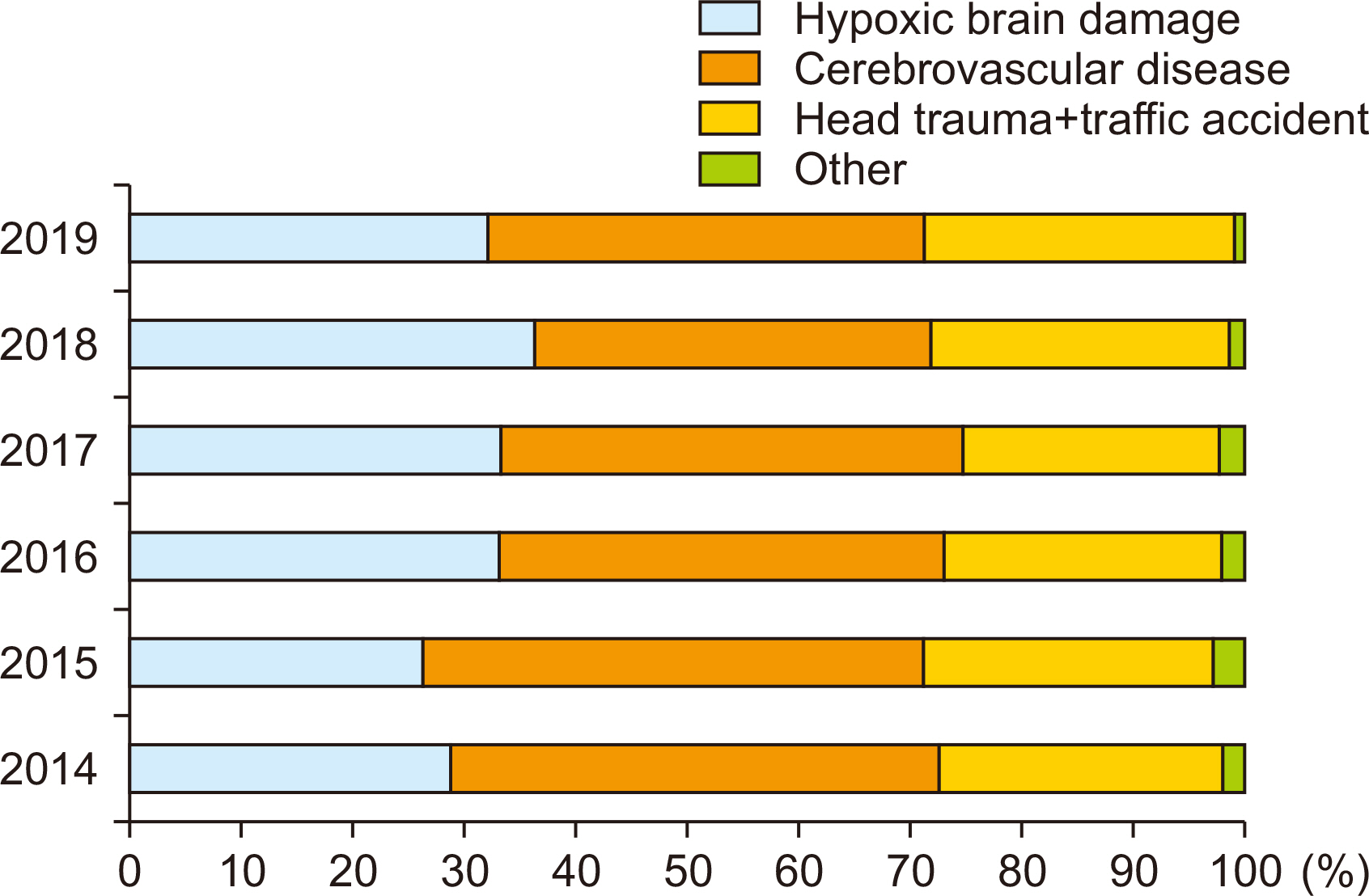
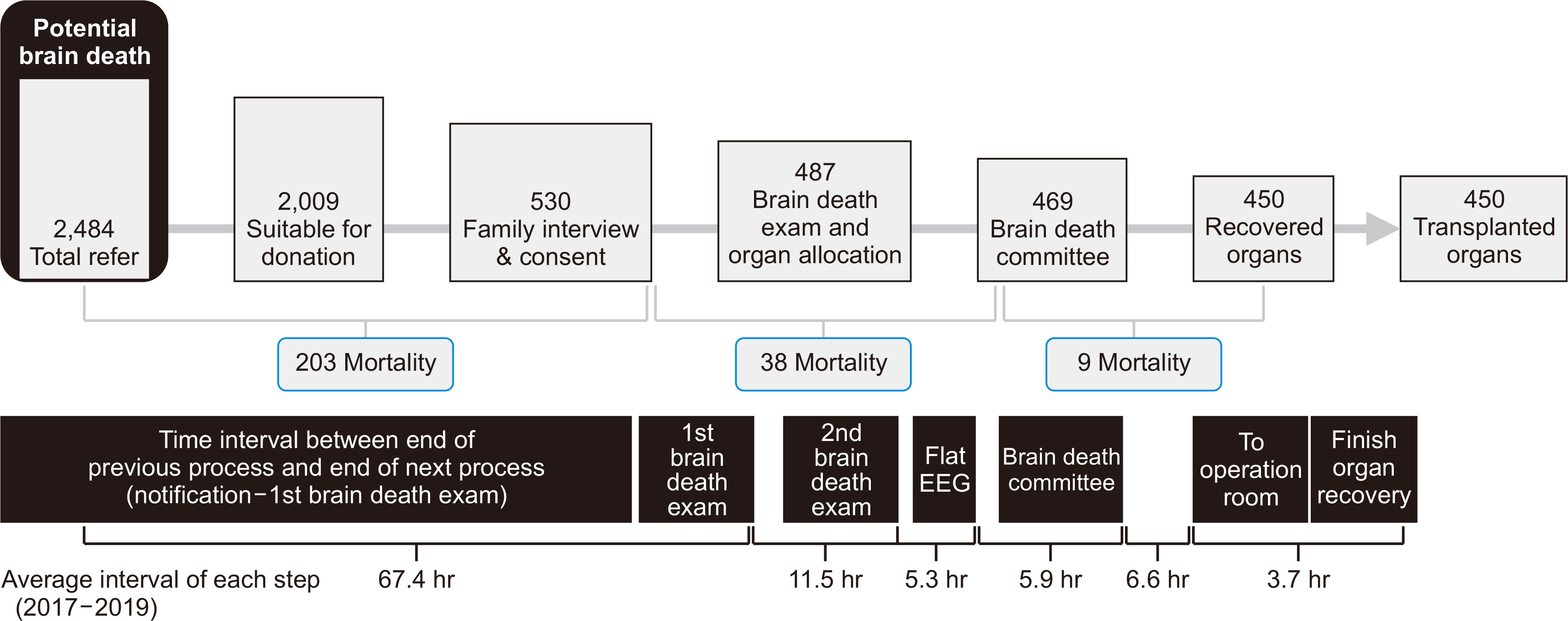
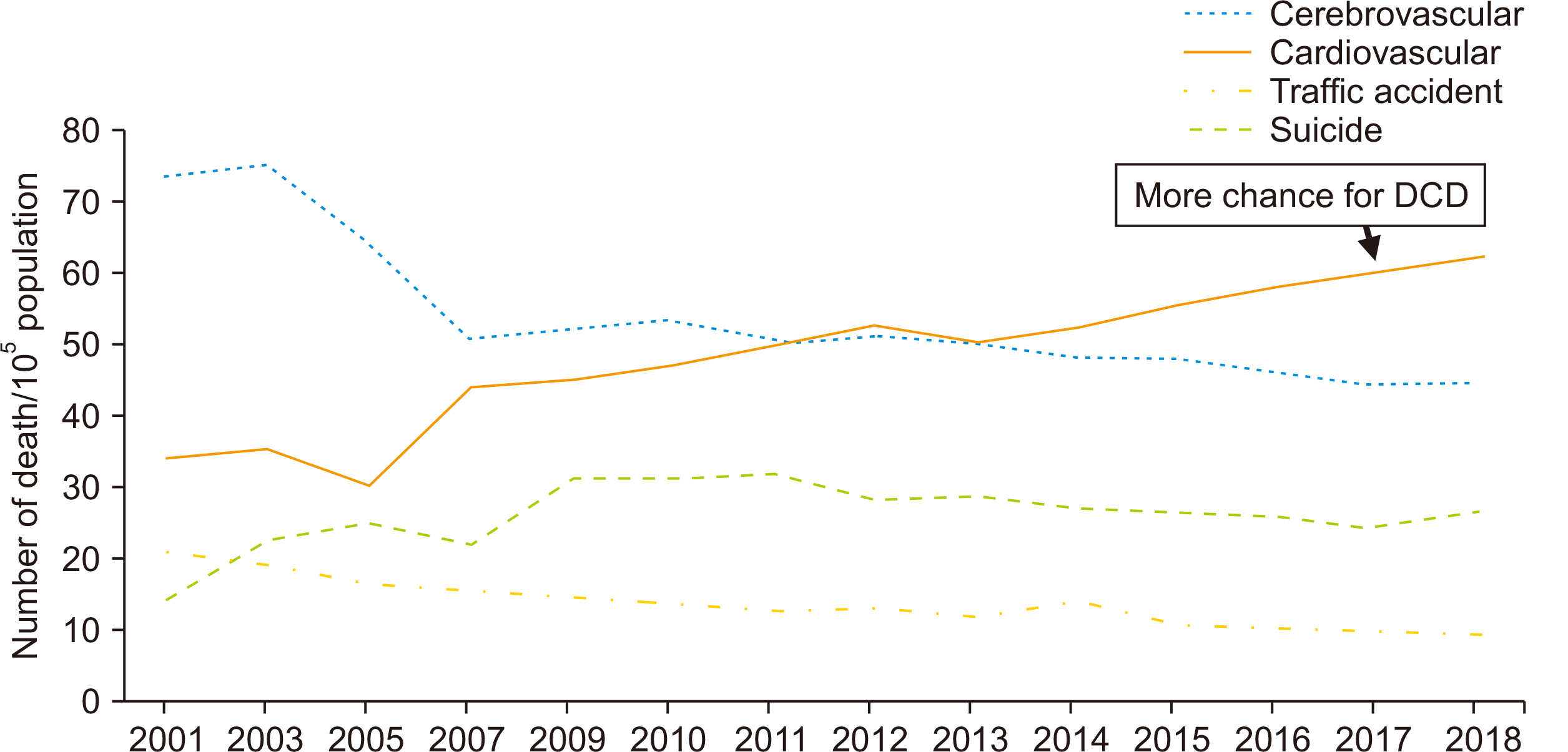
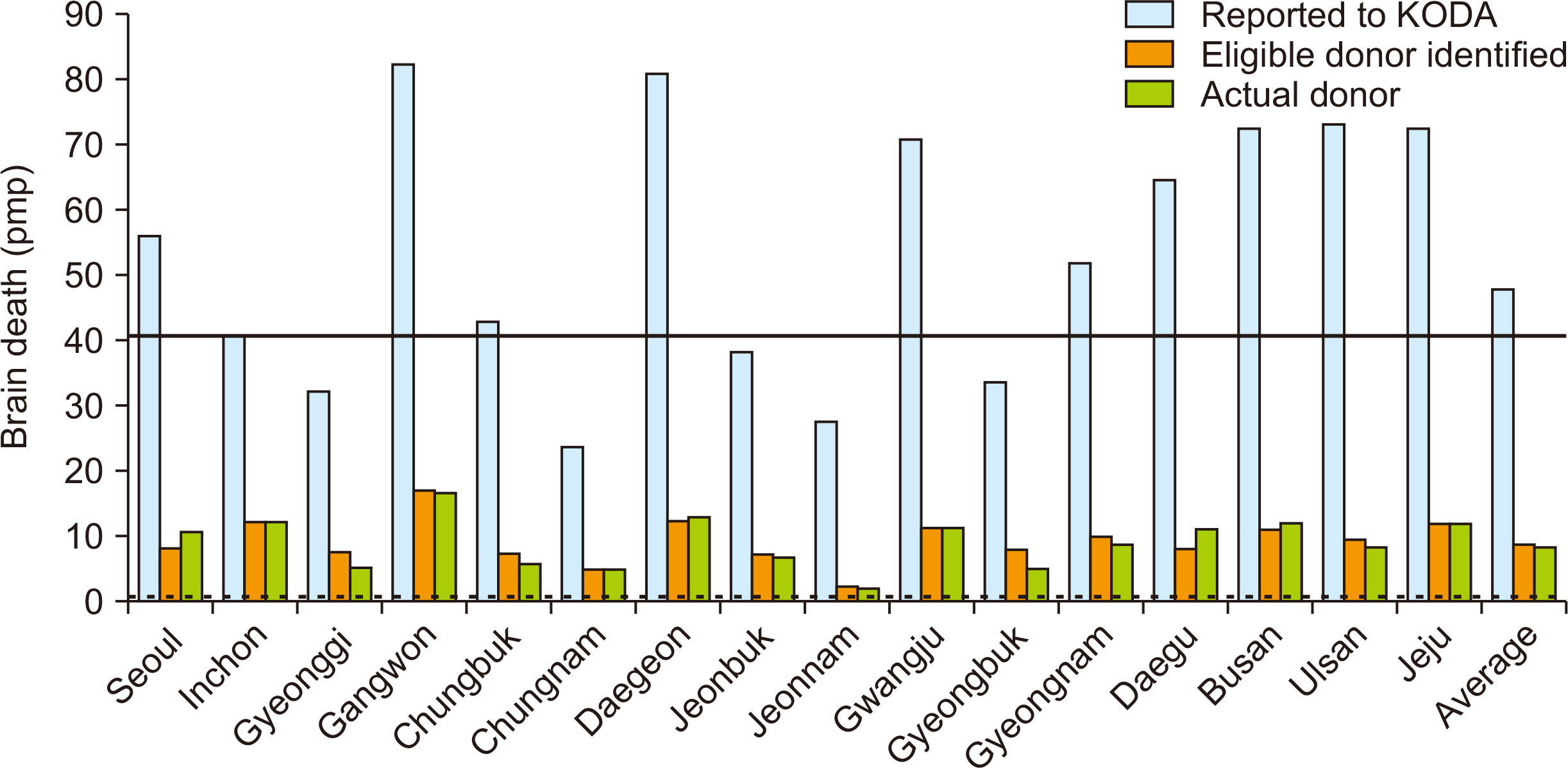
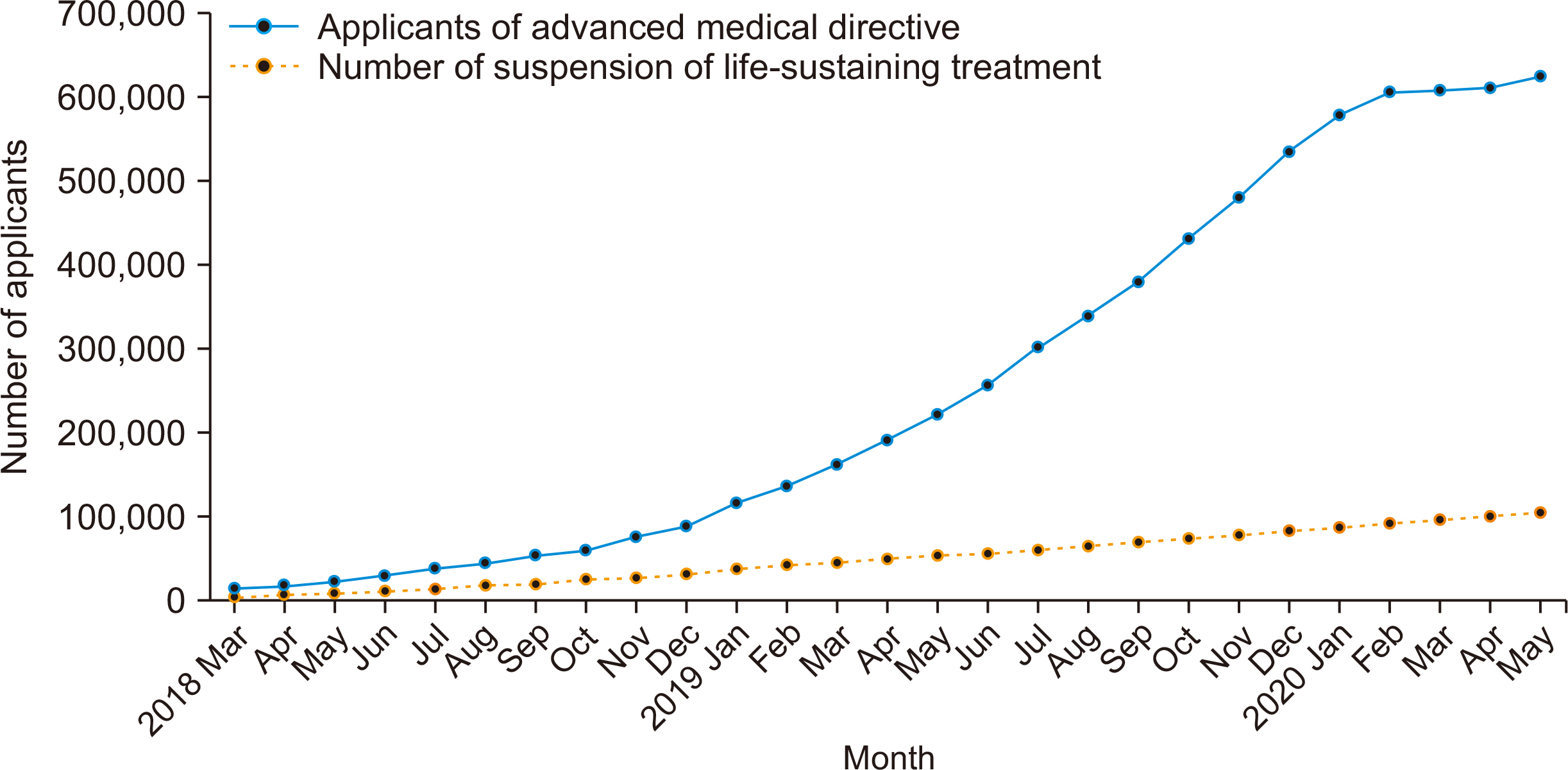
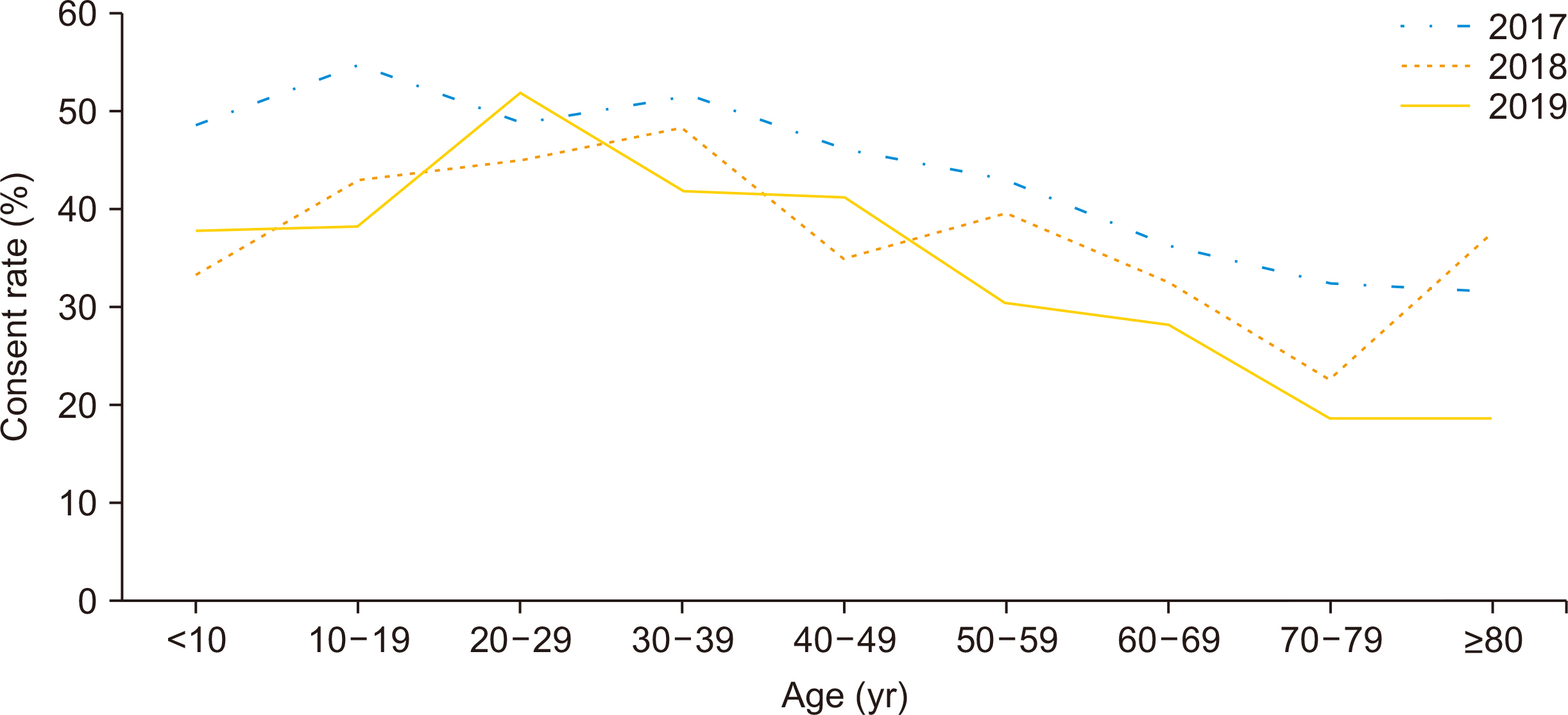
- In 2019, 1,630 organs were recovered from 450 brain death donors nationwide and were transplanted into 1,612 transplant recipients. However, considering that the number of potential brain-dead linked to the Korea Organ Donation Agency (KODA) information center was 2,484, only 18.1% of the linked brain-dead donated successfully. Of the 1,606 people who were available for family interviews, 67.0% refused to donate, so their cause analysis and countermeasures are needed. In particular, 203 reported cases died during the early period of donor evaluation, so we need a special concern on these cases. After consent, 67 cases failed to donate due to death or poor organ condition, and this raises the question of the possibility of shortening brain death management time. The average time interval from the first investigation to the completion of the second investigation (11.5 hours), until obtaining a flat electroencephalogram (5.3 hours) and conclusion of the brain death committee is 5.9 hours. Reducing unnecessary brain death management time is expected to improve the quality of organs and increase the number of organs to be recovered. Therefore, efforts to accurately identify and report potential brain death, and efforts to reduce the time spent in confirming brain death together with improving awareness of organ donation in people across the country are necessary to increase the number of deceased donors even in the current brain death management system. Implementation of donation after circulatory death for mortality case during the donor management is also urgent.
Keyword
Figure
Cited by 1 articles
-
The impact of Model for End-Stage Liver Disease score on deceased donor liver transplant outcomes in low volume liver transplantation center: a retrospective and single-center study
Doo-Ho Lee, Yeon Ho Park, Seok Won Choi, Kug Hyun Nam, Sang Tae Choi, Doojin Kim
Ann Surg Treat Res. 2021;101(6):360-367. doi: 10.4174/astr.2021.101.6.360.
Reference
-
1. Korea Organ Donation Agency. 2019. KODA annual report 2019. Korea Organ Donation Agency;Seoul:2. Klassen DK, Edwards LB, Stewart DE, Glazier AK, Orlowski JP, Berg CL. 2016; The OPTN deceased donor potential study: implications for policy and practice. Am J Transplant. 16:1707–14. DOI: 10.1111/ajt.13731. PMID: 26813036.
Article3. Statistics Korea. 2019. Changes in death rates by major causes of death from report on the causes of death statistics 2019. Statistics Korea;Daejeon:4. International registry in organ donation and transplantation. Preliminary numbers 2018: IRODat international registry in organ donation and transplantation [Internet]. International registry in organ donation and transplantation;Barcelona: Available from: www.irodat.org. cited 2020 Oct 20.5. Sandroni C, D'Arrigo S, Callaway CW, Cariou A, Dragancea I, Taccone FS, et al. 2016; The rate of brain death and organ donation in patients resuscitated from cardiac arrest: a systematic review and meta-analysis. Intensive Care Med. 42:1661–71. DOI: 10.1007/s00134-016-4549-3. PMID: 27699457. PMCID: PMC5069310.
Article6. 2002. National Agency for Management of Life-Sustaining Treatment website [Internet]. National Agency for Management of Life-Sustaining Treatment;Seoul: Available from: https://www.lst.go.kr. cited 2020 Dec 5.7. Verheijde JL, Rady MY, McGregor JL. 2007; The United States Revised Uniform Anatomical Gift Act (2006): New challenges to balancing patient rights and physician responsibilities. Philos Ethics Humanit Med. 2:19. DOI: 10.1186/1747-5341-2-19. PMID: 17850664. PMCID: PMC2001294.
Article8. Siminoff LA, Gordon N, Hewlett J, Arnold RM. 2001; Factors influencing families' consent for donation of solid organs for transplantation. JAMA. 286:71–7. DOI: 10.1001/jama.286.1.71. PMID: 11434829.
Article9. Haliko S, Arnold R. 2002. Fast facts and concepts #79: discussing organ donation with families [Internet]. Palliative Care Network of Wisconsin;Available from: https://www.mypcnow.org/fast-fact/discussing-organ-donation-with-families/. cited 2020 Oct 10.10. Shemie SD, Baker AJ, Knoll G, Wall W, Rocker G, Howes D, et al. 2006; National recommendations for donation after cardiocirculatory death in Canada: donation after cardiocirculatory death in Canada. CMAJ. 175:S1. DOI: 10.1503/cmaj.060895. PMID: 17124739. PMCID: PMC1635157.11. Bernat JL, D'Alessandro AM, Port FK, Bleck TP, Heard SO, Medina J, et al. 2006; Report of a National Conference on Donation after cardiac death. Am J Transplant. 6:281–91. DOI: 10.1111/j.1600-6143.2005.01194.x. PMID: 16426312.
Article12. Sokohl K. 2002; First person consent: OPOs across the country are adapting to the change. UNOS Update. 1. 3. PMID: 15460622.13. Callison K, Levin A. 2016; Donor registries, first-person consent legislation, and the supply of deceased organ donors. J Health Econ. 49:70–5. DOI: 10.1016/j.jhealeco.2016.06.009. PMID: 27388535.
Article14. Blood and Transplant. 2020. Tell your family and friends: take time to talk about organ donation [Internet]. Blood and Transplant;Bristol: Available from: www.organdonation.nhs.uk/. cited 2020 Oct 10.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Repeat Blood Donors and Iron Deficiency Anemia
- Trends in Deceased Organ Donation and Utilization in Korea: 2000-2009
- Determination of factors influencing family decision upon organ or tissue donation request in potential deceased organ donors in Malaysia: a 22-years national audit
- Assessment of hospital deceased organ donation potential at St. Luke’s Medical Center–Quezon City
- Meaningful Correlation between the donor registration rate and the number of organ donors by region