J Korean Assoc Oral Maxillofac Surg.
2020 Dec;46(6):379-384. 10.5125/jkaoms.2020.46.6.379.
Diagnostic analysis of vertical orbital dystopia and canthal tilt for surgical correction
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, Seoul St. Mary’s Hospital, Seoul, Korea
- 2Department of Oral and Maxillofacial Surgery, Chung-Ang University Hospital, Seoul, Korea
- 3Department of Oral and Maxillofacial Surgery, Dental Research Institute, School of Dentistry, Seoul National University, Seoul, Korea
- KMID: 2510007
- DOI: http://doi.org/10.5125/jkaoms.2020.46.6.379
Abstract
Objectives
We sought to identify a clinically useful method of analyzing orbital dystopia to aid in diagnosis and treatment planning and to quantify vertical discrepancies in eye level and variations in canthal tilt in Koreans.
Patients and Methods
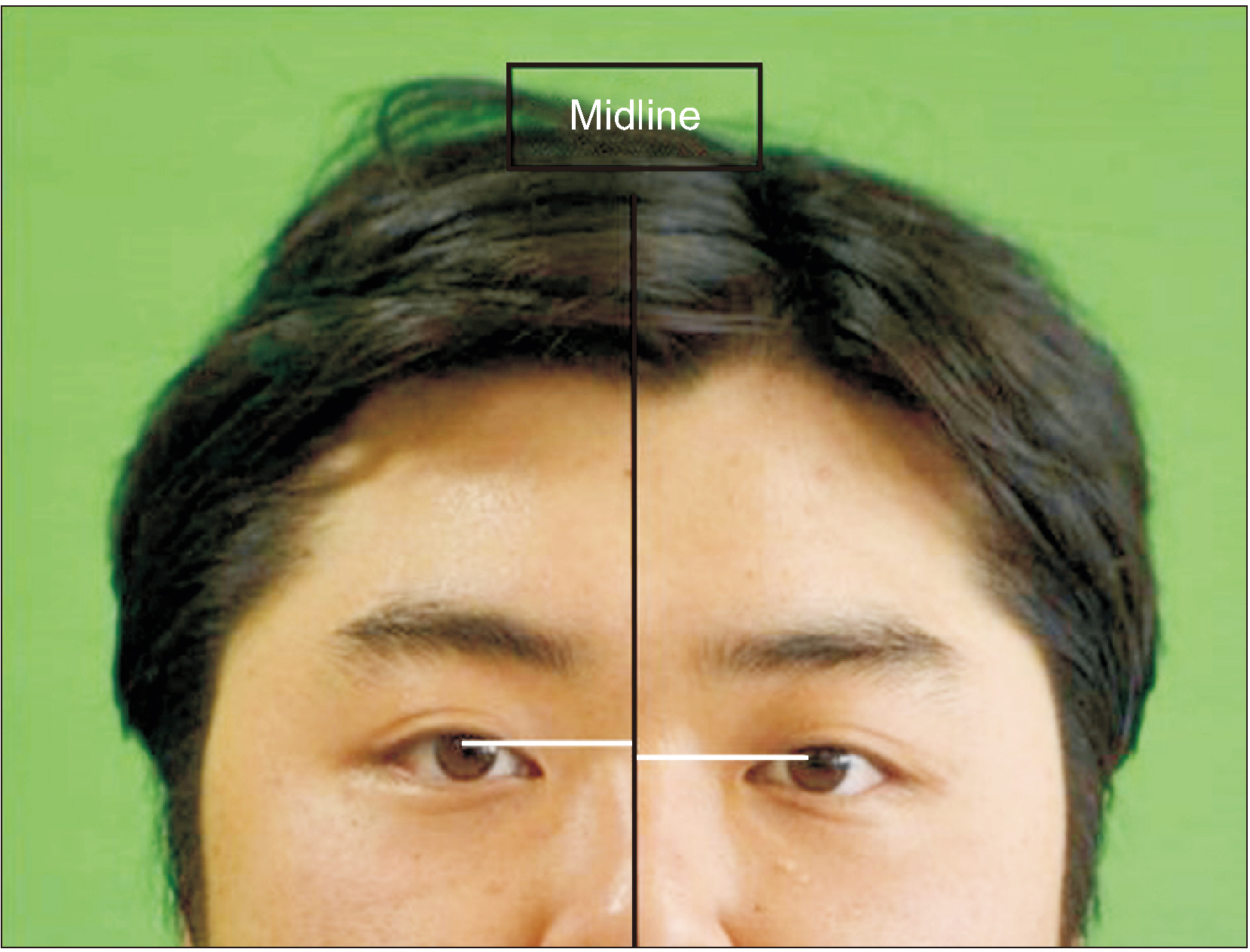
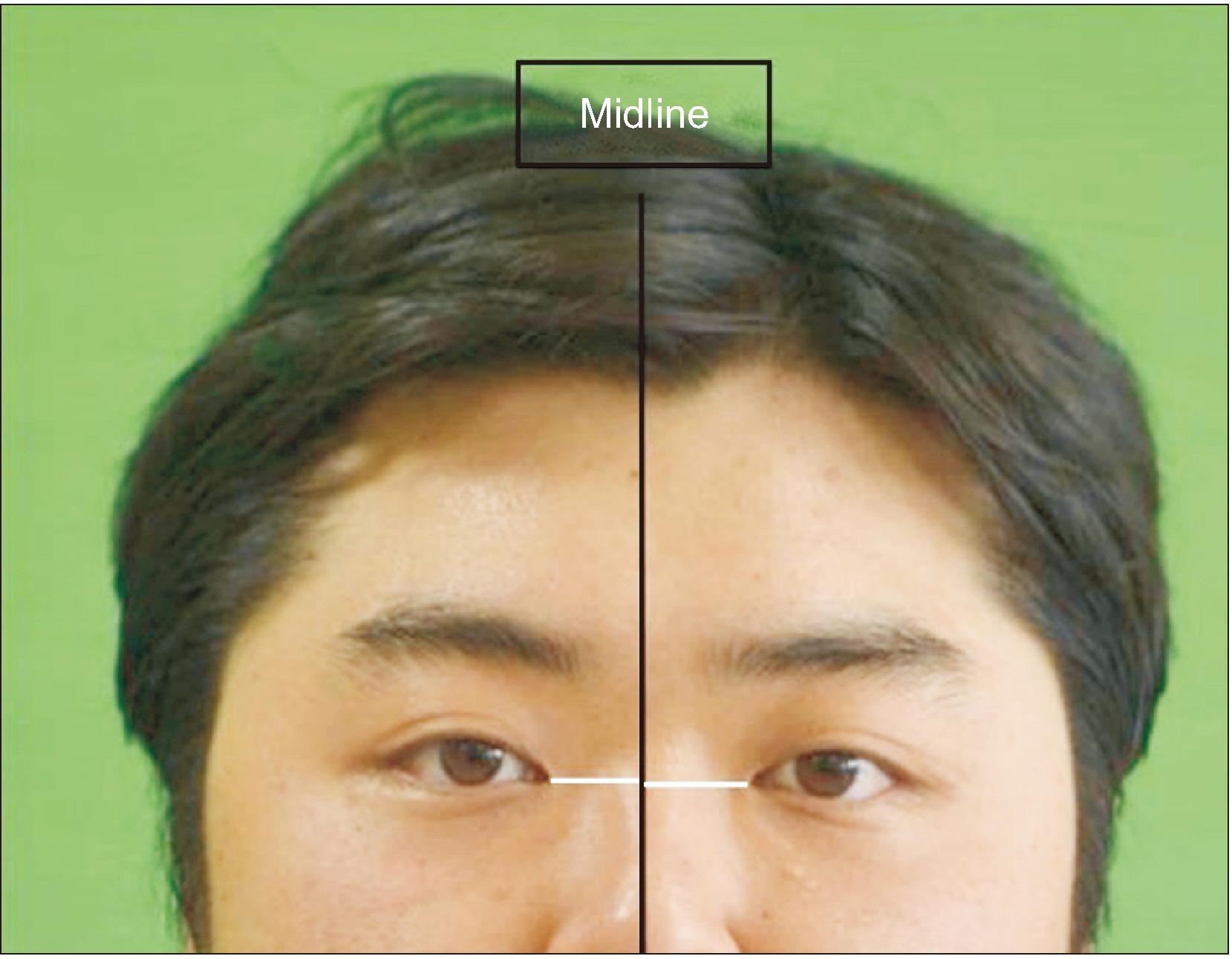
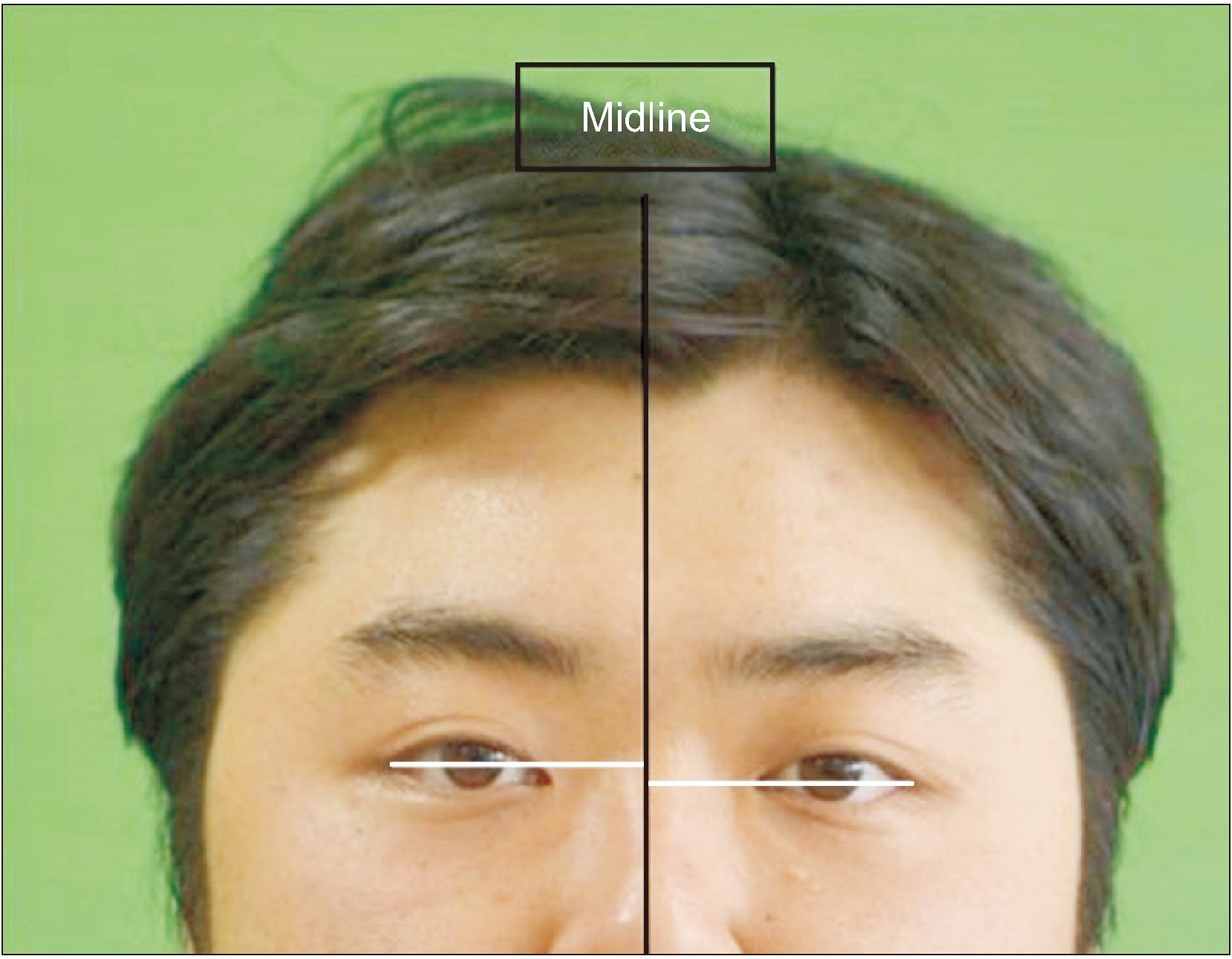
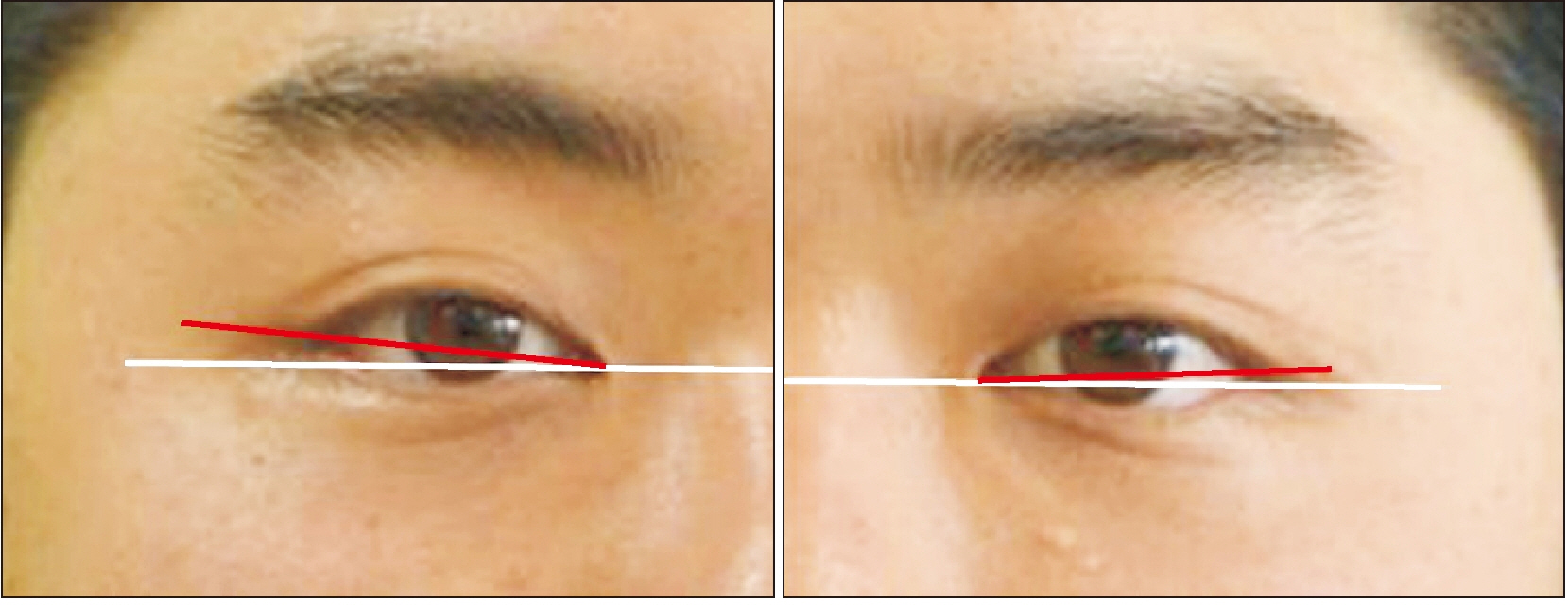
In 76 Korean patients with a mean age of 23.12 years, mean differences in the level of the pupils, lateral canthi, medial canthi, and canthal tilt were measured. The difference in pupil level was calculated from the perpendicular lines drawn from the midpupil area of each eye to the midline of the face to determine the amount of skeletal discrepancy of the eye. Soft tissue discrepancies were determined according to the vertical difference between the lines drawn from the lateral or medial canthus of each eye perpendicular to the midline of the face. The canthal tilt was determined from the inclination of a line connecting the lateral and medial canthi, then classified as class I, II, or III.
Results
Mean differences in pupil level, medial canthi, and lateral canthi were 1.57±1.10 mm, 1.14±1.07 mm, and 2.03±1.64 mm, respectively. The mean degree of canthal tilt were 8.45°±3.53° for the right side and 8.42°±3.81° for the left side. No study participants presented with class III canthal tilt. The mean canthal tilt values for those with class I tilt were 3.21°±1.68° for the right side and 3.18°±1.63° for the left side, while, for those who had class II tilt, the values were 9.60°±3.66° for the right side and 9.54°±2.99° for the left side.
Conclusion
The presented diagnostic method of orbital dystopia can be used to effectively establish a treatment plan that takes into consideration the patient’s skeletal and soft-tissue discrepancies.
Keyword
Figure
Reference
-
References
1. Choi KY. 2015; Analysis of facial asymmetry. Arch Craniofac Surg. 16:1–10. https://doi.org/10.7181/acfs.2015.16.1.1 . DOI: 10.7181/acfs.2015.16.1.1. PMID: 28913211. PMCID: PMC5556787.
Article2. Song WC, Koh KS, Kim SH, Hu KS, Kim HJ, Park JC, et al. 2007; Horizontal angular asymmetry of the face in Korean young adults with reference to the eye and mouth. J Oral Maxillofac Surg. 65:2164–8. https://doi.org/10.1016/j.joms.2006.11.018 . DOI: 10.1016/j.joms.2006.11.018. PMID: 17954309.
Article3. Hwang HS, Youn IS, Lee KH, Lim HJ. 2007; Classification of facial asymmetry by cluster analysis. Am J Orthod Dentofacial Orthop. 132:279.e1–6. https://doi.org/10.1016/j.ajodo.2007.01.017 . DOI: 10.1016/j.ajodo.2007.01.017. PMID: 17826592.
Article4. Altug-Atac AT, Grayson BH, McCarthy JG. 2008; Comparison of skeletal and soft-tissue changes following unilateral mandibular distraction osteogenesis. Plast Reconstr Surg. 121:1751–9. https://doi.org/10.1097/PRS.0b013e31816aa003 . DOI: 10.1097/PRS.0b013e31816aa003. PMID: 18454000.
Article5. Yamashita Y, Nakamura Y, Shimada T, Nomura Y, Hirashita A. 2009; Asymmetry of the lips of orthognathic surgery patients. Am J Orthod Dentofacial Orthop. 136:559–63. https://doi.org/10.1016/j.ajodo.2007.10.057 . DOI: 10.1016/j.ajodo.2007.10.057. PMID: 19815159.
Article6. Yu CC, Bergeron L, Lin CH, Chu YM, Chen YR. 2009; Single-splint technique in orthognathic surgery: intraoperative checkpoints to control facial symmetry. Plast Reconstr Surg. 124:879–86. https://doi.org/10.1097/PRS.0b013e3181b03842 . DOI: 10.1097/PRS.0b013e3181b03842. PMID: 19730307.
Article7. Edgerton MT, Jane JA. 1981; Vertical orbital dystopia--surgical correction. Plast Reconstr Surg. 67:121–38. PMID: 7465660.
Article8. Tan ST, Mulliken JB. 1997; Hypertelorism: nosologic analysis of 90 patients. Plast Reconstr Surg. 99:317–27. https://doi.org/10.1097/00006534-199702000-00004 . DOI: 10.1097/00006534-199702000-00004. PMID: 9030136.
Article9. Shakir S, Hoppe IC, Taylor JA. 2019; State-of-the-art hypertelorism management. Clin Plast Surg. 46:185–95. https://doi.org/10.1016/j.cps.2018.11.004 . DOI: 10.1016/j.cps.2018.11.004. PMID: 30851750.
Article10. Laure B, Batut C, Benouhagrem A, Joly A, Travers N, Listrat A, et al. 2019; Addressing hypertelorism: indications and techniques. Neurochirurgie. 65:286–94. https://doi.org/10.1016/j.neuchi.2019.09.007 . DOI: 10.1016/j.neuchi.2019.09.007. PMID: 31557491.
Article11. Batut C, Joly A, Travers N, Guichard B, Paré A, Laure B. 2019; Surgical treatment of orbital hypertelorism: historical evolution and development prospects. J Craniomaxillofac Surg. 47:1712–9. https://doi.org/10.1016/j.jcms.2019.07.002 . DOI: 10.1016/j.jcms.2019.07.002. PMID: 31519384.
Article12. Winters R. 2016; Tessier clefts and hypertelorism. Facial Plast Surg Clin North Am. 24:545–58. https://doi.org/10.1016/j.fsc.2016.06.013 . DOI: 10.1016/j.fsc.2016.06.013. PMID: 27712820.
Article13. Engel M, Hoffmann J, Castrillon-Oberndorfer G, Freudlsperger C. 2015; The value of three-dimensional printing modelling for surgical correction of orbital hypertelorism. Oral Maxillofac Surg. 19:91–5. https://doi.org/10.1007/s10006-014-0466-1 . DOI: 10.1007/s10006-014-0466-1. PMID: 25249178.
Article14. Liu DL, Shan L, Yuan Q, Huang JJ. 2011; Refinement of the correction of orbital hypertelorism. J Craniofac Surg. 22:217–9. https://doi.org/10.1097/SCS.0b013e3181f7604f . DOI: 10.1097/SCS.0b013e3181f7604f. PMID: 21233750.
Article15. Tan ST, Ashworth G, Czypionka S, Poole MD, Briggs M. 1996; Vertical orbital dystopia. Plast Reconstr Surg. 97:1349–61. https://doi.org/10.1097/00006534-199606000-00004 . PMID: 7465660.
Article16. Poole MD, Briggs M. 1990; The cranio-facio-cervical scoliosis complex. Br J Plast Surg. 43:670–5. https://doi.org/10.1016/0007-1226(90)90187-5 . DOI: 10.1016/0007-1226(90)90187-5. PMID: 2257416.
Article17. Kim EJ, Ki EJ, Cheon HM, Choi EJ, Kwon KH. 2013; 3-Dimensional analysis for class III malocclusion patients with facial asymmetry. J Korean Assoc Oral Maxillofac Surg. 39:168–74. https://doi.org/10.5125/jkaoms.2013.39.4.168 . DOI: 10.5125/jkaoms.2013.39.4.168. PMID: 24471038. PMCID: PMC3858129.
Article18. Cook JT. 1980; Asymmetry of the cranio-facial skeleton. Br J Orthod. 7:33–8. https://doi.org/10.1179/bjo.7.1.33 . DOI: 10.1179/bjo.7.1.33. PMID: 6932963.
Article19. Moore FO, Thornton BP, Zabel DD, Vasconez HC. 2004; Autogenous orbital reconstruction in a child with congenital abnormalities of the orbital roof and vertical orbital dystopia. J Craniofac Surg. 15:930–3. https://doi.org/10.1097/00001665-200411000-00008 . DOI: 10.1097/00001665-200411000-00008. PMID: 15547377.
Article20. Tessier P. Tessier P, Rougier J, Wolfe SA, editors. 1981. Congenital orbital dystopias. Plastic surgery of the orbit and eyelids. Masson Publishing;New York: p. 191–9.21. De Ponte FS, Fadda T, Rinna C, Brunelli A, Iannetti G. 1997; Early and late surgical treatment of orbital dystopia in craniofacial malformation. J Craniofac Surg. 8:17–22. https://doi.org/10.1097/00001665-199701000-00008 . DOI: 10.1097/00001665-199701000-00008. PMID: 10332293.
Article22. Rhee SC, Woo KS, Kwon B. 2012; Biometric study of eyelid shape and dimensions of different races with references to beauty. Aesthetic Plast Surg. 36:1236–45. https://doi.org/10.1007/s00266-012-9937-7 . DOI: 10.1007/s00266-012-9937-7. PMID: 22810555.
Article23. Farkas LG. 1994. Anthropometry of the head and face. 2nd ed. Raven Press;New York: p. 101–11.24. Lam BL, Lam S, Walls RC. 1995; Prevalence of palpebral fissure asymmetry in white persons. Am J Ophthalmol. 120:518–22. https://doi.org/10.1016/s0002-9394(14)72667-4 . DOI: 10.1016/s0002-9394(14)72667-4. PMID: 7573311.
Article25. Doganay F, Dadaci Z, Topcu-Yilmaz P, Doganay Aydin H. 2017; The association between ocular dominance and physiological palpebral fissure asymmetry. Laterality. 22:412–8. https://doi.org/10.1080/1357650X.2016.1209212 . DOI: 10.1080/1357650X.2016.1209212. PMID: 27461553.
Article26. Song WC, Kim SJ, Kim SH, Hu KS, Kim HJ, Koh KS. 2007; Asymmetry of the palpebral fissure and upper eyelid crease in Koreans. J Plast Reconstr Aesthet Surg. 60:251–5. https://doi.org/10.1016/j.bjps.2006.04.027 . DOI: 10.1016/j.bjps.2006.04.027. PMID: 17293281.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Orbital dystopia: assessing surgical outcome
- Treatment of Fibrous Dysplasia of the Fronto-Orbital Area with Radical Resection and Autogenous Reconstruction Using Split Calvarial Bone Graft: A Case Report
- Endoscopic treatment of blowout fracture by lateral canthal incision
- The Direct Medial Canthal Approach in the Repair of Blowout Fracture of the Medial Orbital Wall
- Removal of Silicon-associated Intraorbital Cyst with Gingival Sulcus Incision