J Neurocrit Care.
2020 Dec;13(2):115-118. 10.18700/jnc.200026.
Endovascular treatment for pseudoaneurysm after carotid blowout syndrome
- Affiliations
-
- 1Division of Rheumatology, Department of Internal Medicine, Wonkwang University College of Medicine, Iksan, Republic of Korea
- 2Department of Surgery, Keimyung University School of Medicine, Daegu, Republic of Korea
- 3Department of Neurology, Keimyung University School of Medicine, Daegu, Republic of Korea
- KMID: 2509942
- DOI: http://doi.org/10.18700/jnc.200026
Abstract
- Background
Pseudoaneurysms of the carotid artery are rare and can be both a cause and consequence of carotid blowout syndrome (CBS) in patients with head and neck cancer. Surgical or endovascular treatment approaches may be useful for managing this condition.
Case Report
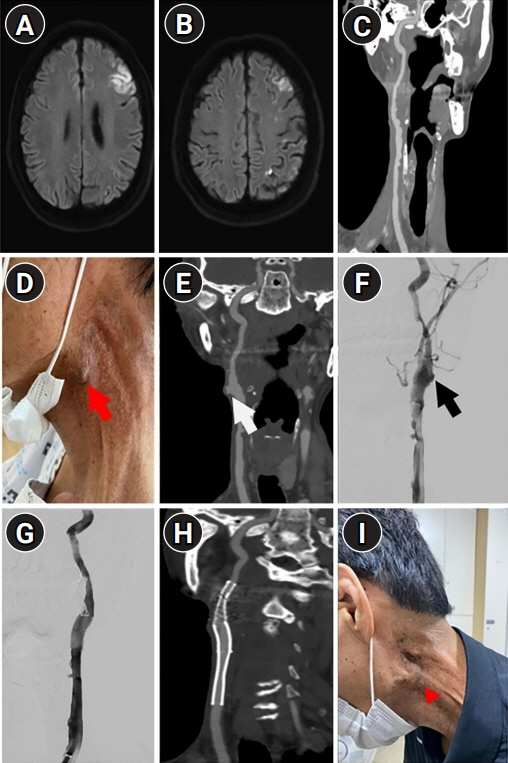
A 55-year-old man presented with a pulsatile mass surrounding the carotid bifurcation in the neck. He reported a history of CBS that occurred as a surgical complication while removing a benign neck cyst. Additionally, he reported a history of laryngeal cancer that underwent complete remission after surgery and radiotherapy. The mass was diagnosed as a pseudoaneurysm. Surgical treatment proved challenging owing to the patient’s history of neck surgery and radiotherapy; therefore, stent-graft deployment was performed and the absence of pulsations was checked through the neck mass.
Conclusion
Endovascular treatment may be a useful therapeutic strategy in cases of post-CBS pseudoaneurysm in patients undergoing surgery and/or radiotherapy for head and neck cancer.
Keyword
Figure
Reference
-
1. Faggioli GL, Freyrie A, Stella A, Pedrini L, Gargiulo M, Tarantini S, et al. Extracranial internal carotid artery aneurysms: results of a surgical series with long-term follow-up. J Vasc Surg. 1996; 23:587–94.
Article2. Bellosta R, Sesana M, Baglini R, Luzzani L, Talarico M, Sarcina A. Endovascular treatment of a symptomatic carotid artery aneurysm with a stent graft. Vasc Endovascular Surg. 2008; 42:276–8.
Article3. Li Z, Chang G, Yao C, Guo L, Liu Y, Wang M, et al. Endovascular stenting of extracranial carotid artery aneurysm: a systematic review. Eur J Vasc Endovasc Surg. 2011; 42:419–26.
Article4. Citardi MJ, Chaloupka JC, Son YH, Ariyan S, Sasaki CT. Management of carotid artery rupture by monitored endovascular therapeutic occlusion (1988-1994). Laryngoscope. 1995; 105:1086–92.
Article5. Chaloupka JC, Putman CM, Citardi MJ, Ross DA, Sasaki CT. Endovascular therapy for the carotid blowout syndrome in head and neck surgical patients: diagnostic and managerial considerations. AJNR Am J Neuroradiol. 1996; 17:843–52.6. Lee CW, Yang CY, Chen YF, Huang A, Wang YH, Liu HM. CT angiography findings in carotid blowout syndrome and its role as a predictor of 1-year survival. AJNR Am J Neuroradiol. 2014; 35:562–7.
Article7. Troutman DA, Mohan CR, Samhouri FA, Sohn RL. Endovascular repair of carotid artery pseudoaneurysm after carotid endarterectomy with self-expanding covered stents-a long-term follow-up. Ann Vasc Surg. 2010; 24:954. e13-6.
Article8. Attigah N, Külkens S, Zausig N, Hansmann J, Ringleb P, Hakimi M, et al. Surgical therapy of extracranial carotid artery aneurysms: long-term results over a 24-year period. Eur J Vasc Endovasc Surg. 2009; 37:127–33.
Article9. Pearson SE, Choi SS. Pseudoaneurysm of the internal carotid artery: a case report and review of the literature. Arch Otolaryngol Head Neck Surg. 2005; 131:454–6.10. Grossi RJ, Onofrey D, Tvetenstrand C, Blumenthal J. Mycotic carotid aneurysm. J Vasc Surg. 1987; 6:81–3.
Article11. Chaloupka JC, Roth TC, Putman CM, Mitra S, Ross DA, Lowlicht RA, et al. Recurrent carotid blowout syndrome: diagnostic and therapeutic challenges in a newly recognized subgroup of patients. AJNR Am J Neuroradiol. 1999; 20:1069–77.12. Lesley WS, Chaloupka JC, Weigele JB, Mangla S, Dogar MA. Preliminary experience with endovascular reconstruction for the management of carotid blowout syndrome. AJNR Am J Neuroradiol. 2003; 24:975–81.13. Bond KM, Brinjikji W, Murad MH, Cloft HJ, Lanzino G. Endovascular treatment of carotid blowout syndrome. J Vasc Surg. 2017; 65:883–8.
Article14. Chang FC, Lirng JF, Luo CB, Guo WY, Teng MM, Tai SK, et al. Carotid blowout syndrome in patients with head-and-neck cancers: reconstructive management by self-expandable stent-grafts. AJNR Am J Neuroradiol. 2007; 28:181–8.15. Tielliu IF, Verhoeven EL, Zeebregts CJ, Prins TR, Span MM, van den Dungen JJ. Endovascular treatment of popliteal artery aneurysms: results of a prospective cohort study. J Vasc Surg. 2005; 41:561–7.
Article16. Chang FC, Lirng JF, Luo CB, Wu HM, Guo WY, Teng MM, et al. A self-expandable stent overlapped with a stent-graft as a cause of endoleak in a patient with carotid blowout syndrome. Clin Radiol. 2008; 63:948–51.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Conjoined Stent Technique for Radiation Induced Long Segment Carotid Stenosis and Pseudoaneurysm
- Cerebral hyperperfusion syndrome after endovascular stent graft reconstruction for postirradiated carotid blowout syndrome: a case report
- Transcarotid Mechanical Thrombectomy for Embolic Intracranial Large Vessel Occlusion after Endovascular Deconstructice Embolization for Carotid Blowout Syndrome
- Traumatic Pseudoaneurysm of the External and Internal Carotid Artery Presenting as Epistaxis: Case Report
- A Rare and Dangerous Combination of COVID-19, Lemierre Syndrome, and Carotid Pseudoaneurysm: A Case Report