J Neurocrit Care.
2020 Dec;13(2):109-114. 10.18700/jnc.200021.
Bupropion overdose as a clinically significant confounder of the neurological examination
- Affiliations
-
- 1Division of Neurocritical Care, Departments of Neurology and Neurosurgery, The University of Texas Southwestern Medical Center, Dallas, TX, USA
- KMID: 2509941
- DOI: http://doi.org/10.18700/jnc.200021
Abstract
- Background
Bupropion is a selective dopamine and norepinephrine reuptake inhibitor utilized in the treatment of multiple neuropsychiatric conditions. It has been implicated as a brain death mimic due to its association with a comatose examination.
Case Report
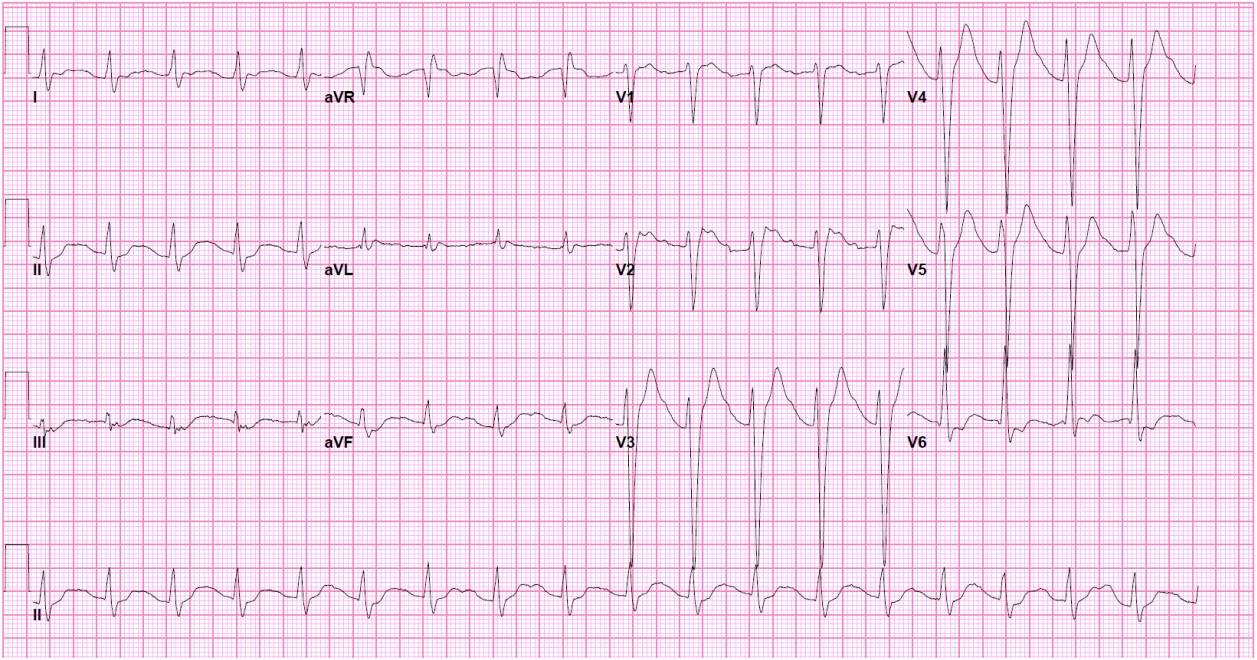
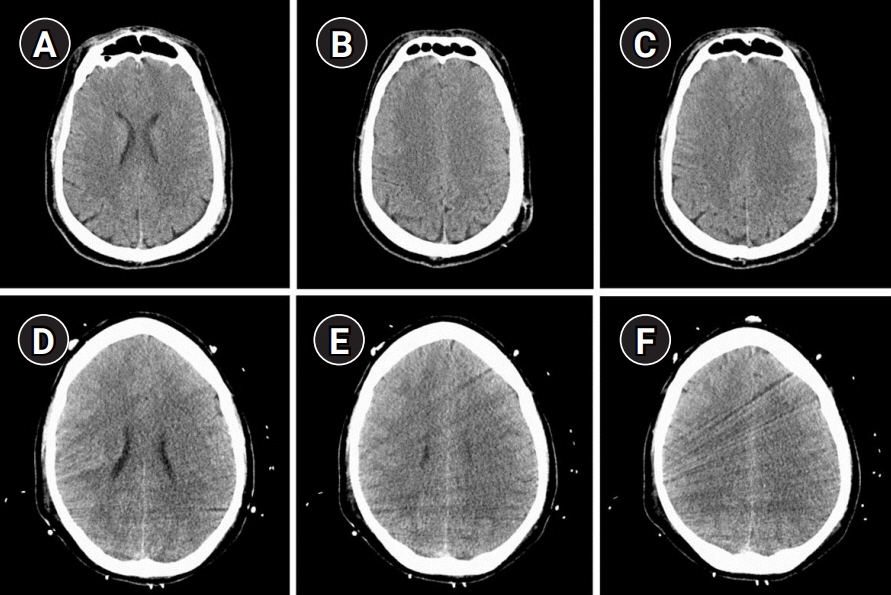
A 31-year-old man with depression and anxiety ingested bupropion as part of a multi-drug overdose in a suicide attempt. During his hospital course, he suffered two cardiopulmonary arrests approximately 24 hours after ingestion. Neurological examination was excessively poor relative to imaging studies and was notable for absent brainstem reflexes. He was treated with targeted temperature management and lipid emulsion therapy with rapid improvement. He was eventually discharged after making a complete neurological recovery.
Conclusion
Bupropion is a unique clinical confounder and may be associated with a disproportionately poor neurological examination in the setting of intoxication. Many factors should be considered in the approach to evaluation, treatment, and prognostication of these patients.
Figure
Reference
-
1. Stahl SM, Pradko JF, Haight BR, Modell JG, Rockett CB, Learned-Coughlin S. A review of the neuropharmacology of bupropion, a dual norepinephrine and dopamine reuptake inhibitor. Prim Care Companion J Clin Psychiatry. 2004; 6:159–66.
Article2. Herrman NW, Kalisieski MJ, Fung C. Bupropion overdose complicated by cardiogenic shock requiring vasopressor support and lipid emulsion therapy. J Emerg Med. 2020; 58:e47–50.
Article3. Levy E, Kim J, Dicker R. Bupropion overdose in adolescents: three cases illuminating presentations and sequelae: a case series and review. J Clin Pharmacol Toxicol. 2018; 2:1–3.4. Jepsen F, Matthews J, Andrews FJ. Sustained release bupropion overdose: an important cause of prolonged symptoms after an overdose. Emerg Med J. 2003; 20:560–1.
Article5. Stranges D, Lucerna A, Espinosa J, Malik N, Mongeau M, Schiers K, et al. A Lazarus effect: a case report of bupropion overdose mimicking brain death. World J Emerg Med. 2018; 9:67–9.
Article6. Farias-Moeller R, Carpenter JL. Coma with absent brainstem reflexes and burst suppression after bupropion overdose in a child. Neurocrit Care. 2017; 26:119–21.
Article7. Mundi JP, Betancourt J, Ezziddin O, Tremayne B, Majic T, Mosenifar Z. Dilated and unreactive pupils and burst-suppression on electroencephalography due to buproprion overdose. J Intensive Care Med. 2012; 27:384–8.
Article8. Larsen RS, Waters J. Neuromodulatory correlates of pupil dilation. Front Neural Circuits. 2018; 12:21.
Article9. Berling I, Isbister GK. Mirtazapine overdose is unlikely to cause major toxicity. Clin Toxicol (Phila). 2014; 52:20–4.
Article10. Lee-Kelland R, Zehra S, Mappa P. Fluoxetine overdose in a teenager resulting in serotonin syndrome, seizure and delayed onset rhabdomyolysis. BMJ Case Rep. 2018; 2018:bcr2018225529.
Article11. Spiller HA, Strauch J, Essing-Spiller SJ, Burns G. Thirteen years of oxcarbazepine exposures reported to US poison centers: 2000 to 2012. Hum Exp Toxicol. 2016; 35:1055–9.12. Cantrell FL, Mena O, Gary RD, McIntyre IM. An acute gabapentin fatality: a case report with postmortem concentrations. Int J Legal Med. 2015; 129:771–5.
Article13. Spiehler VR, Fukumoto RI. Another fatal case involving hydroxyzine. J Anal Toxicol. 1984; 8:242–3.
Article14. Wijdicks EF, Varelas PN, Gronseth GS, Greer DM; American Academy of Neurology. Evidence-based guideline update: determining brain death in adults: report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2010; 74:1911–8.
Article