Anat Cell Biol.
2020 Dec;53(4):393-397. 10.5115/acb.20.041.
Intraluminal anatomy of the transverse sinus: implications for endovascular therapy
- Affiliations
-
- 1Department of Neurosurgery, Hospital Santo Tomas, Panamá, Panama
- 2Aiken Regional Medical Centers, Aiken, SC,USA
- 3Department of Neurosurgery, Tulane Center for Clinical Neurosciences, Tulane University School of Medicine, New Orleans, LA, USA
- 4Division of Gross and Clinical Anatomy, Department of Anatomy, Kurume University School of Medicine, Kurume, Japan
- 5Department of Anatomical Sciences, St. George’s University, St. George’s, Grenada
- 6Department of Neurosurgery and Ochsner Neuroscience Institute, Ochsner Health System, New Orleans, LA, USA
- 7Department of Structural and Cellular Biology, Tulane University School of Medicine, New Orleans, LA, USA
- KMID: 2509683
- DOI: http://doi.org/10.5115/acb.20.041
Abstract
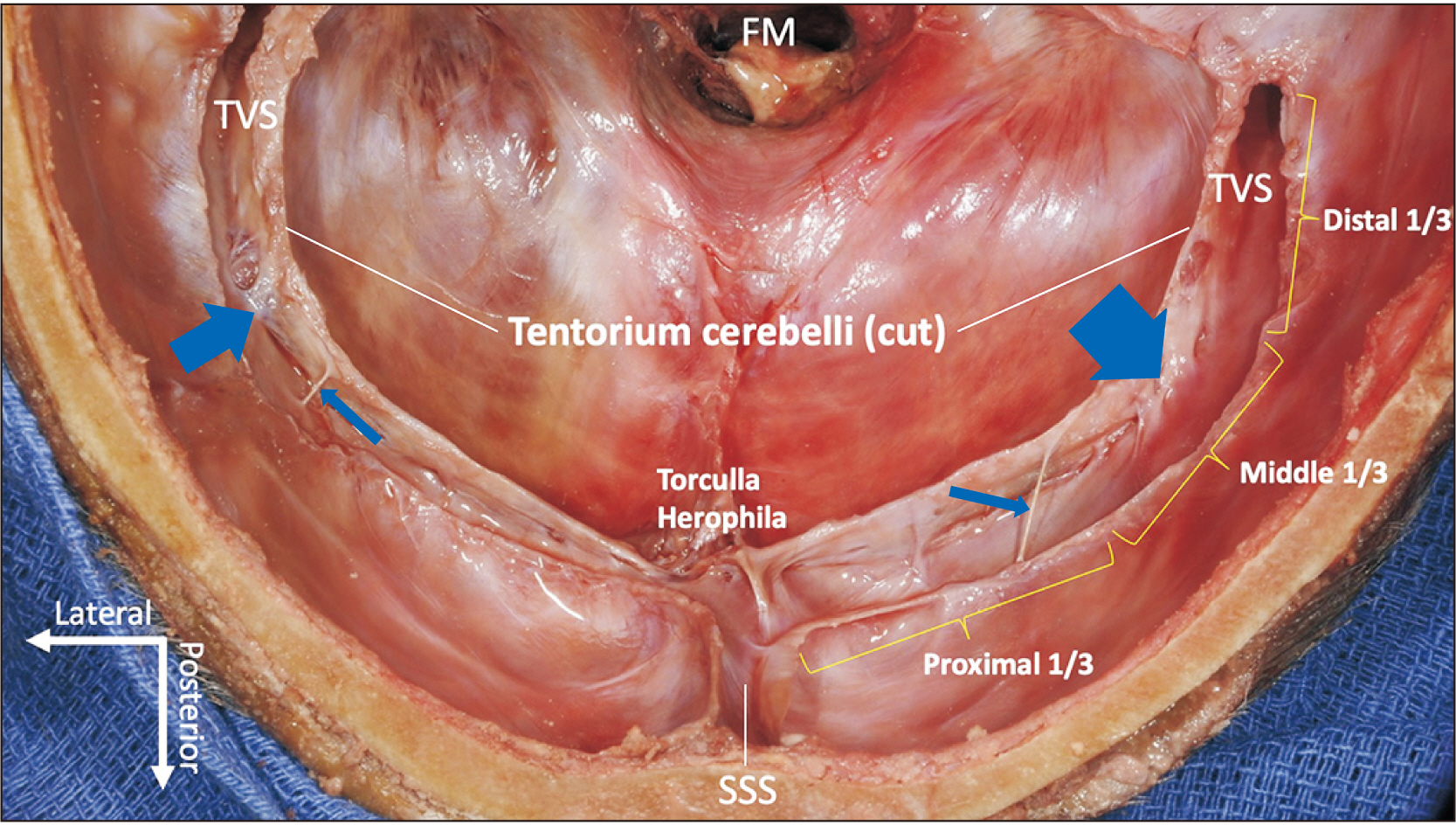
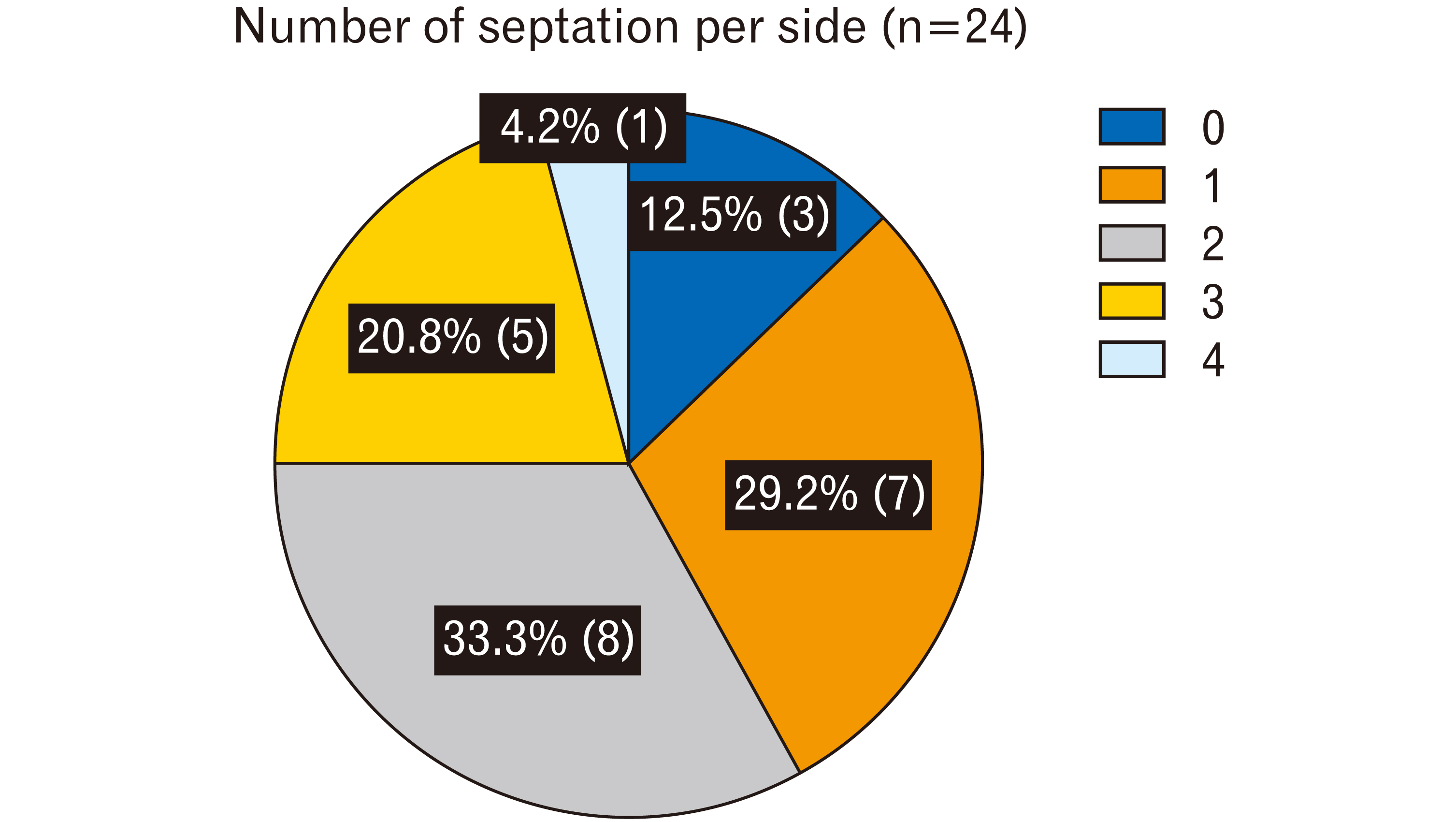
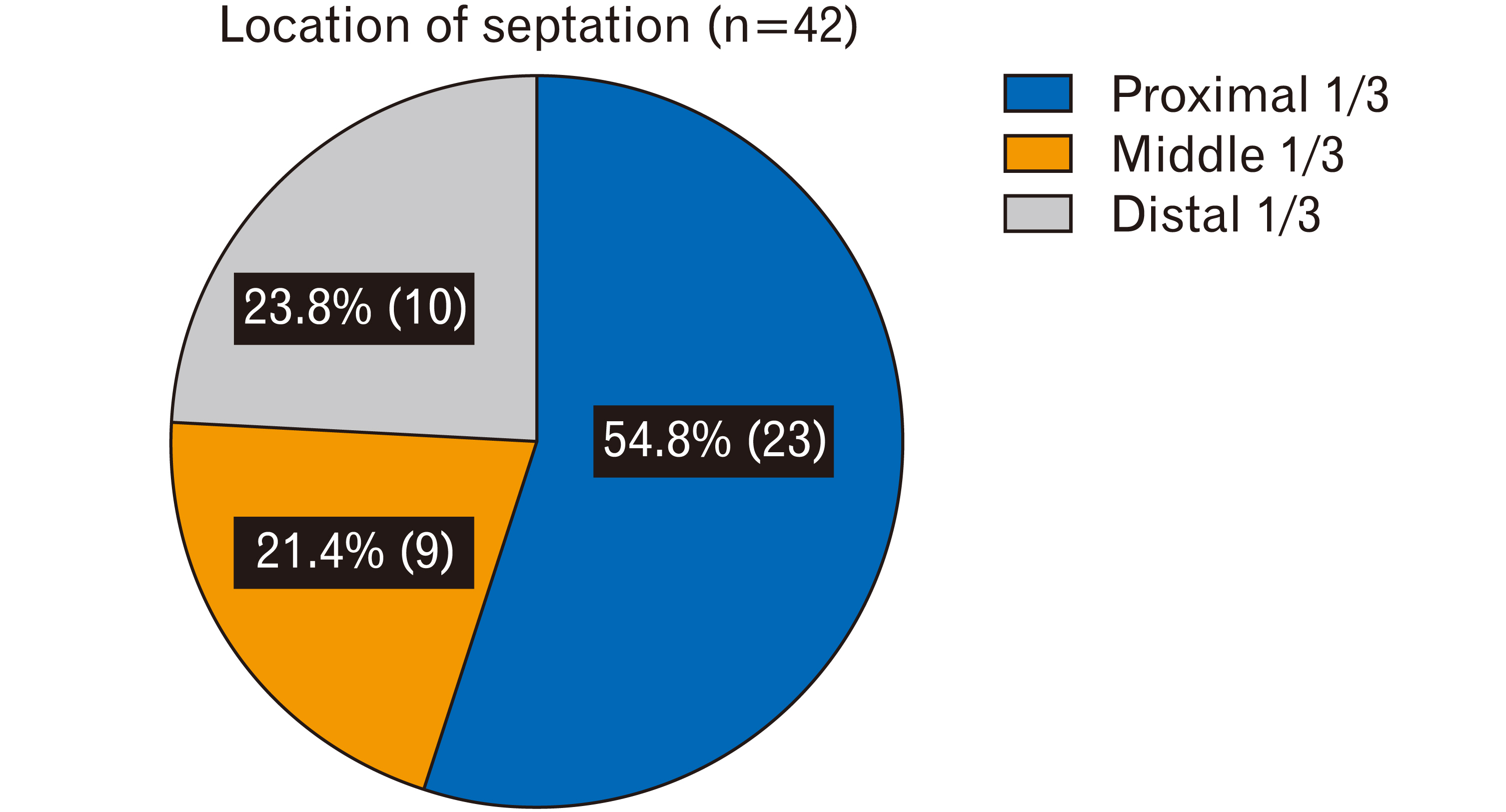
- Trabeculae or septations in the transverse sinus can have potentially life-threatening clinical significance. The current study demonstrates trabecula/septum patterning within the transverse sinus with measurements and distribution data supplemented by imaging, and describes the possible etiology of idiopathic intracranial hypertension and turbulent blood flow in the transverse sinus. Twenty-four sides from 12 cadaveric heads, all fresh-frozen, were used (five males, seven females; age at death 65–91 years, mean 79.1 years). The length and diameter of the transverse sinus were measured along with the number and locations of septations/trabeculae and their tensile strength. The mean length of the transverse sinus was 68.43 mm on the right side and 74.31 mm on the left. A total of 42 septations were found in the 24 transverse sinuses. The number of septations per side ranged from zero to four with a mean of 1.75. The septations were located in the proximal 1/3 in 54.8% (23/42), the middle 1/3 in 21.4% (9/42), and the distal 1/3 in 23.8% (10/42). The work presented here furthers our understanding of transverse sinus anatomy, including its detailed internal architecture. The measurements can provide a technical guide for neurosurgeons and influence instrument selection when a large thrombus forms or anchors in one of these trabeculae or septa and necessitates treatment.
Figure
Cited by 1 articles
-
Trabeculae in the basilar venous plexus: anatomical and histological study with application to intravascular procedures
Viktoriya S. Grayson, Mitchell Couldwell, Arada Chaiyamoon, Juan J. Cardona, Francisco Reina, Ana Carrera, Erin P. McCormack, Kendrick Johnson, Sassan Keshavarzi, Joe Iwanaga, Aaron S. Dumont, R. Shane Tubbs
Anat Cell Biol. 2023;56(4):435-440. doi: 10.5115/acb.23.171.
Reference
-
References
1. Standring S. 2008. Gray's anatomy: the anatomical basis of clinical practice. 40th ed. Churchill Livingstone/Elsevier;Edinburgh:2. Curé JK, Van Tassel P, Smith MT. 1994; Normal and variant anatomy of the dural venous sinuses. Semin Ultrasound CT MR. 15:499–519. DOI: 10.1016/S0887-2171(05)80019-8. PMID: 7880564.
Article3. Strydom MA, Briers N, Bosman MC, Steyn S. 2010; The anatomical basis of venographic filling defects of the transverse sinus. Clin Anat. 23:153–9. DOI: 10.1002/ca.20911. PMID: 20014389.
Article4. Subramaniam RM, Tress BM, King JO, Eizenberg N, Mitchell PJ. 2004; Transverse sinus septum: a new aetiology of idiopathic intracranial hypertension? Australas Radiol. 48:114–6. DOI: 10.1111/j.1440-1673.2004.01269.x. PMID: 15230741.
Article5. Tomaszewski KA, Henry BM, Kumar Ramakrishnan P, Roy J, Vikse J, Loukas M, Tubbs RS, Walocha JA. 2017; Development of the Anatomical Quality Assurance (AQUA) checklist: guidelines for reporting original anatomical studies. Clin Anat. 30:14–20. DOI: 10.1002/ca.22800. PMID: 27801507.
Article6. Lake S, Altafulla JJ, Iwanaga J, Oskouian RJ, Loukas M, Tubbs RS. 2018; A cadaveric case of a circular torcular Herophili. Cureus. 10:e3099. DOI: 10.7759/cureus.3099. PMID: 30338175. PMCID: PMC6173274.
Article7. Ahmed MS, Imtiaz S, Shazlee MK, Ali M, Iqbal J, Usman R. 2018; Normal variations in cerebral venous anatomy and their potential pitfalls on 2D TOF MRV examination: results from a private tertiary care hospital in Karachi. J Pak Med Assoc. 68:1009–13. PMID: 30317292.8. Chandra A, Li WA, Stone CR, Geng X, Ding Y. 2017; The cerebral circulation and cerebrovascular disease I: anatomy. Brain Circ. 3:45–56. DOI: 10.4103/bc.bc_10_17. PMID: 30276305. PMCID: PMC6126264.9. Schaller B. 2004; Physiology of cerebral venous blood flow: from experimental data in animals to normal function in humans. Brain Res Brain Res Rev. 46:243–60. DOI: 10.1016/j.brainresrev.2004.04.005. PMID: 15571768.
Article10. Valdueza JM, von Münster T, Hoffman O, Schreiber S, Einhäupl KM. 2000; Postural dependency of the cerebral venous outflow. Lancet. 355:200–1. DOI: 10.1016/S0140-6736(99)04804-7. PMID: 10675123.11. Donnelly J, Budohoski KP, Smielewski P, Czosnyka M. 2016; Regulation of the cerebral circulation: bedside assessment and clinical implications. Crit Care. 20:129. DOI: 10.1186/s13054-016-1293-6. PMID: 27145751. PMCID: PMC4857376.
Article12. Alper F, Kantarci M, Dane S, Gumustekin K, Onbas O, Durur I. 2004; Importance of anatomical asymmetries of transverse sinuses: an MR venographic study. Cerebrovasc Dis. 18:236–9. DOI: 10.1159/000079960. PMID: 15273441.
Article13. Fofi L, Giugni E, Vadalà R, Vanacore N, Aurilia C, Egeo G, Pierallini A, Barbanti P. 2012; Cerebral transverse sinus morphology as detected by MR venography in patients with chronic migraine. Headache. 52:1254–61. DOI: 10.1111/j.1526-4610.2012.02154.x. PMID: 22553914.
Article14. Han K, Chao AC, Chang FC, Hsu HY, Chung CP, Sheng WY, Chan L, Wu J, Hu HH. 2016; Diagnosis of transverse sinus hypoplasia in magnetic resonance venography: new insights based on magnetic resonance imaging in combined dataset of venous outflow impairment case-control studies: post hoc case-control study. Medicine (Baltimore). 95:e2862. DOI: 10.1097/MD.0000000000002862. PMID: 26962781. PMCID: PMC4998862.15. Balik V, Uberall I, Sulla I, Ehrmann J, Kato Y, Sulla IJ, Takizawa K. 2019; Variability in wall thickness and related structures of major dural sinuses in posterior cranial fossa: a microscopic anatomical study and clinical implications. Oper Neurosurg (Hagerstown). 17:88–96. DOI: 10.1093/ons/opy287. PMID: 30395343.
Article16. DE Simone R, Ranieri A, Bonavita V. 2017; Starling resistors, autoregulation of cerebral perfusion and the pathogenesis of idiopathic intracranial hypertension. Panminerva Med. 59:76–89. DOI: 10.23736/S0031-0808.16.03248-1. PMID: 27598891.17. Shim EB, Heldt T. 2018; Fluid-structure interaction in the cerebral venous transverse sinus. Conf Proc IEEE Eng Med Biol Soc. 2018:4544–7. DOI: 10.1109/EMBC.2018.8513150. PMID: 30441362.
Article18. Boddu SR, Gobin P, Oliveira C, Dinkin M, Patsalides A. 2018; Anatomic measurements of cerebral venous sinuses in idiopathic intracranial hypertension patients. PLoS One. 13:e0196275. DOI: 10.1371/journal.pone.0196275. PMID: 29856739. PMCID: PMC5983447.
Article19. Cappuzzo JM, Hess RM, Morrison JF, Davies JM, Snyder KV, Levy EI, Siddiqui AH. 2018; Transverse venous stenting for the treatment of idiopathic intracranial hypertension, or pseudotumor cerebri. Neurosurg Focus. 45:E11. DOI: 10.3171/2018.5.FOCUS18102. PMID: 29961386.
Article20. Miyachi S, Hiramatsu R, Ohnishi H, Takahashi K, Kuroiwa T. 2018; Endovascular treatment of idiopathic intracranial hypertension with stenting of the transverse sinus stenosis. Neurointervention. 13:138–43. DOI: 10.5469/neuroint.2018.00990. PMID: 30196687. PMCID: PMC6132029.
Article21. Patsalides A, Oliveira C, Wilcox J, Brown K, Grover K, Gobin YP, Dinkin MJ. 2019; Venous sinus stenting lowers the intracranial pressure in patients with idiopathic intracranial hypertension. J Neurointerv Surg. 11:175–78. DOI: 10.1136/neurintsurg-2018-014032. PMID: 29871989. PMCID: PMC6582809.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Contralateral Transverse Sinus Occlusion After Treatment of Transverse-Sigmoid Sinus Dural Arteriovenous Fistula: A Case Report
- Persistent fetal superficial middle cerebral vein: an anatomical study
- Effect of Transverse Sinus Stenting on Diffuse Leukoencephalopathy with Idiopathic Intracranial Hypertension
- The Role of Transverse Arch in Foot Stiffness and Its Clinical Implications
- Anatomical Variations of Cerebral MR Venography: Is Gender Matter?