Recent Decrease in Organ Donation from Brain-Dead Potential Organ Donors in Korea and Possible Causes
- Affiliations
-
- 1Department of Critical Care Medicine and Neurology, Ewha Womans University Seoul Hospital, Seoul, Korea.
- 2Department of Medical Education, Ewha Womans University School of Medicine, Seoul, Korea.
- KMID: 2509601
- DOI: http://doi.org/10.3346/jkms.2020.35.e94
Abstract
- Background
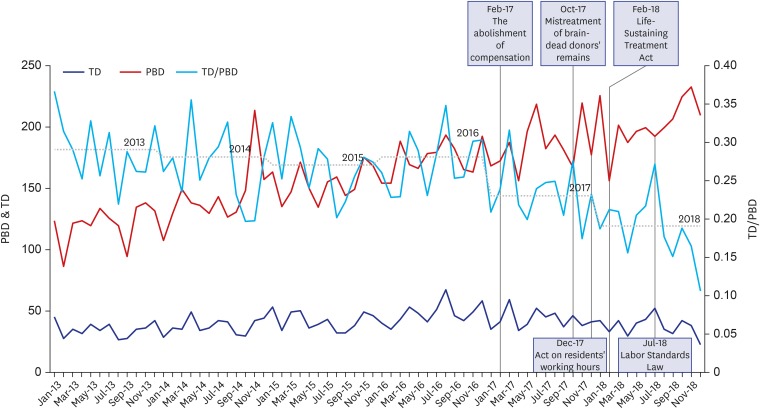
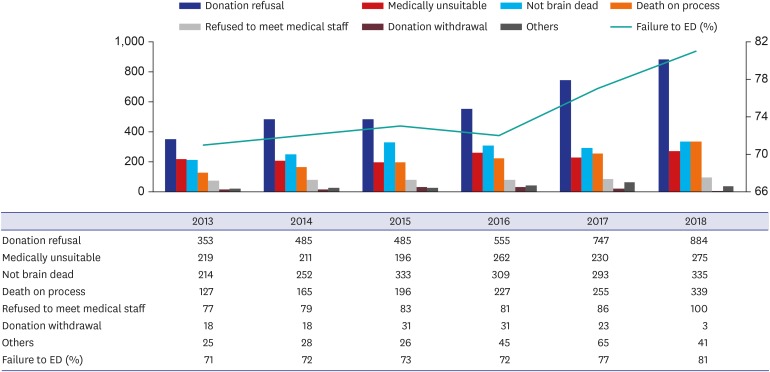
In 1999, the Organ Transplantation Act legalized organ donation from brain-dead patients. As a result of the government's continued efforts, the number of brain-dead donors steadily increased from 2002 through 2016. However, the number has declined since 2017. This paper examined the possible reasons behind the decline in brain-dead organ donation.
Methods
This investigation was an analysis of published data from the Korea Organ Donation Agency annual reports from 2013 to 2018.
Results
The number of brain-dead organ donors in Korea rose steadily until 2016, declined in 2017 for the first time since 2002, and then dropped sharply in 2018. Although the number of brain-dead potential organ donors increased between 2017 and 2018, the number of eligible donors decreased, suggesting that patient families rejected the brain-death determination process and brain-dead organ donation. Statistics gathered during identification of brain-dead potential donors and actual donations confirm that rejection or withdrawal of consent by the family has increased. During the same period when donation from brain- dead patients decreased, five events occurred: 1) compensation for donor families was abolished; 2) an incident of mistreatment of a brain-dead donor's remains occurred; 3) the Life-Sustaining Treatment Act was enacted, providing a legal procedure whereby families of brain-dead patients could forgo life-sustaining treatment; 4) residents' work week was limited to 80 hours; and 5) the Labor Standards Law was amended.
Conclusion
Fewer eligible donors in spite of an increase in brain-dead potential organ donors suggests that reduction in these donations resulted mainly from factors associated with family consent. Among such factors, implementation of the Life-sustaining Treatment Act appears to be most important. Abolition of family compensation and the incident in which a brain-dead donor's remains were mistreated may also have influenced family consent.
Keyword
Figure
Cited by 3 articles
-
Analysis of Factors Affecting Emergency Physicians’ Attitudes toward Deceased Organ & Tissue Donation
Dong Eun Lee, Hyun Kim, Kwi Hwa Park, Song Yi Park, Seung Min Park, Yong Hun Jung, Wonjoon Jeong, Kyung Hye Park
J Korean Med Sci. 2021;36(49):e329. doi: 10.3346/jkms.2021.36.e329.Exploring the experiences and perspectives of emergency physicians on brain death organ tissue donation after the Life-Sustaining Treatment Decision Act
Song Yi Park, Hyun Kim, Kwi Hwa Park, Seung Min Park, Dong Eun Lee, Yong Hun Jung, Wonjoon Jeong, Kyung Hye Park
Korean J Transplant. 2022;36(1):29-36. doi: 10.4285/kjt.22.0005.Recent Trends in the Withdrawal of Life-Sustaining Treatment in Patients with Acute Cerebrovascular Disease : 2017–2021
Seung Hwan Kim, Ji Hwan Jang, Young Zoon Kim, Kyu Hong Kim, Taek Min Nam
J Korean Neurosurg Soc. 2024;67(1):73-83. doi: 10.3340/jkns.2023.0074.
Reference
-
1. Korea Ministry of Government Legislation. Internal organs, etc. Transplant act. Updated 2018. Accessed September 23, 2019. http://www.law.go.kr/engLsSc.do?tabMenuId=tab45&query=%EC%9E%A5%EA%B8%B0%EB%93%B1#.2. Korean Organ Donation Agency. Annual Report. Seoul: Korean Organ Donation Agency;2012.3. Korean Organ Donation Agency. Annual Report. Seoul: Korean Organ Donation Agency;2018.4. Korean Organ Donation Agency. KODA donation flow. Accessed September 23, 2019. https://www.koda1458.kr/organ/brain_deth.do.5. Jeon MG, Lee JS. The problems of law on transplantation of internal organs etc and plan to improve. Natl Law Study. 2012; 8(2):121–141.6. Yoo JM, Hong MC, Lee MS. Changes in the governance of organ sharing in Korea: Possibility of cooperative governance. J Gov Stud. 2017; 12(3):169–196.7. Song YM. The recent global trends over the method of expression of will in organ donation. Bio Med Law. 2018; 19:67–92.
Article8. Yi JK. Die Zustimmungsproblemtik bei der Organspende. Bio Med Law. 2017; 17:167–184.
Article9. Korea Ministry of Government Legislation. Act on decisions on life-sustaining treatment for patients in hospice and palliative care or at the end of life. Updated 2018. Accessed September 23, 2019. http://www.law.go.kr/engLsSc.do?tabMenuId=tab45&query=%EC%97%B0%EB%AA%85%EC%9D%98%EB%A3%8C#.10. Park JT. Court decisions and legal considerations about the withdrawal of the life-prolonging medical care. J Korean Med Assoc. 2019; 62(7):358–368.
Article11. Ministry of Health and Welfare. Pilot Project on Life-Sustaining Treatment Implemented from October 23rd to Next Year January 15th. Updated 2017. Accessed September 23, 2019. https://www.mohw.go.kr/react/al/sal0301vw.jsp?PAR_MENU_ID=04&MENU_ID=0403&CONT_SEQ=342502.12. Kim MI, Oh J, Cho WH, Kim DS, Jung CW, You YD, et al. Causes of failure during the management process from identification of brain-dead potential organ donors to actual donation in Korea: a 5-year data analysis (2012–2016). J Korean Med Sci. 2018; 33(50):e326. PMID: 30534034.
Article13. Cho WH. Status of organ donation and solution of organ shortage in Korea. J Korean Soc Transplant. 2018; 32(3):38–48.
Article14. Lee JM, Lee YJ, Kyung KD, Im YC, Oh CK, Ahn JH, et al. Clinical analysis of 10 years brain death donors in single center after Korean network for organ sharing. J Korean Soc Transplant. 2010; 24(3):196–203.
Article15. Ministry of Health and Welfare. Answer to Request of Information Disclosure about Brain Death Organ Donation Statistics, Request No. 1AA-1912-462123 (December 21, 2019). Sejong: Ministry of Health and Welfare;2019.16. Veatch RM, Ross LF. Transplantation Ethics. Washington, D.C.: Georgetown University Press;2015.17. Lee EW, Jang HY, Han SY, Han KH, Oh SW, Roh YN. Influencing factors affecting successful organ donation and families' consent to donate after brain death. J Korean Soc Transplant. 2017; 31(1):43–48.18. Steering Committee of the Istanbul Summit. Organ trafficking and transplant tourism and commercialism: the Declaration of Istanbul. Lancet. 2008; 372(9632):5–6. PMID: 18603141.19. Kim MG, Jeong JC, Cho EJ, Huh KH, Yang JS, Byeon NI, et al. Operational and regulatory system requirements for pursuing self-sufficiency in deceased donor organ transplantation program in Korea. J Korean Soc Transplant. 2010; 24(3):147–158.
Article20. Korea Centers for Disease Control & Prevention. Standard Manual for Respectful Treatment on Donor Transfer. Cheongju: Korea Centers for Disease Control & Prevention;2019.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Management of brain-dead donors in Korea
- Causes of Failure during the Management Process from Identification of Brain-Dead Potential Organ Donors to Actual Donation in Korea: a 5-Year Data Analysis (2012–2016)
- Medical Management of Brain-Dead Organ Donors
- Assessment of hospital deceased organ donation potential at St. Luke’s Medical Center–Quezon City
- Organ donation from donors with viral hepatitis in South Korea: a 2013–2017 nationwide data analysis