J Cardiovasc Imaging.
2020 Apr;28(2):137-149. 10.4250/jcvi.2019.0111.
Left Ventricular Global Longitudinal Strain as a Predictor for Left Ventricular Reverse Remodeling in Dilated Cardiomyopathy
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Republic of Korea
- 2Cardiovascular Center, Yongin Severance Hospital, Yongin, Republic of Korea
- 3Division of Cardiology, Sanggye-Paik Hospital, Inje University, Seoul, Korea
- KMID: 2509455
- DOI: http://doi.org/10.4250/jcvi.2019.0111
Abstract
- BACKGROUND
A considerable number of patients with dilated cardiomyopathy (DCM) experience left ventricular reverse remodeling (LVRR). LV global longitudinal strain (LV GLS) offers sensitive and reproducible measurement of myocardial dysfunction. The authors sought to evaluate whether LV GLS at the time of diagnosis may predict LVRR in DCM patients with sinus rhythm and investigate its prognostic role in long-term follow-up in this population.
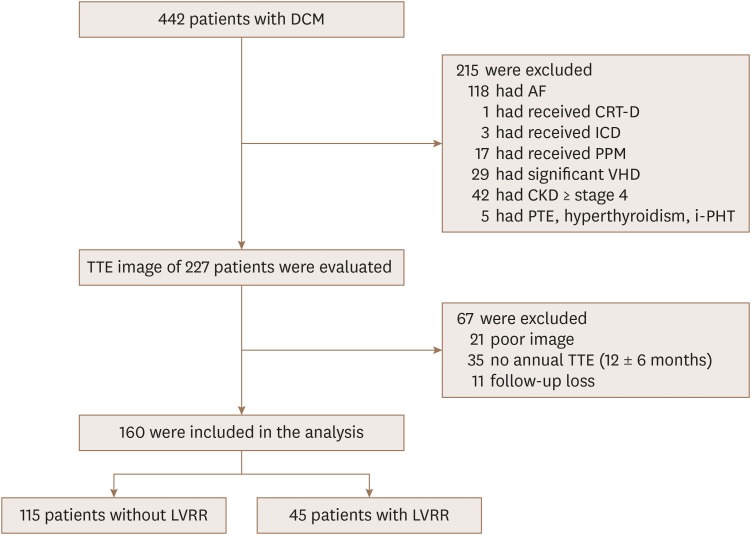
METHODS
We enrolled 160 DCM patients with sinus rhythm who had been initially diagnosed, evaluated, and followed at our institute. We analyzed their medical records and echocardiographic data.
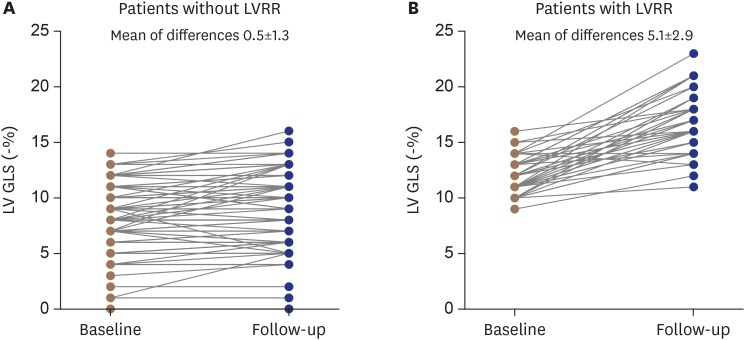
RESULTS
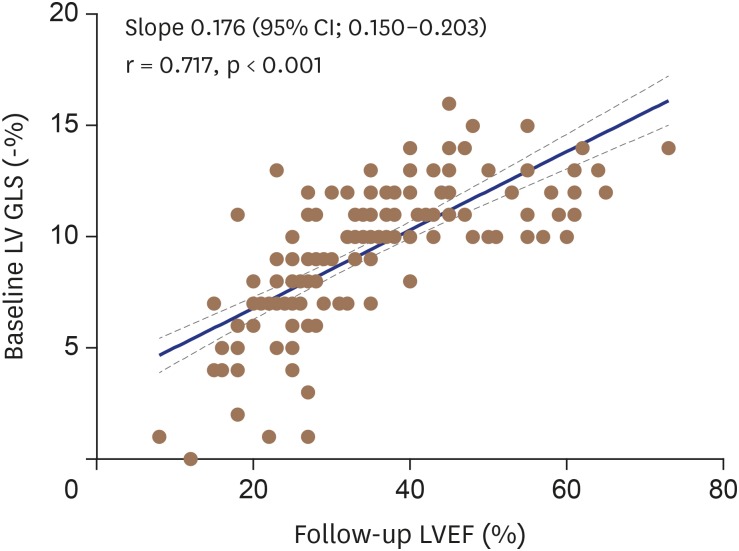
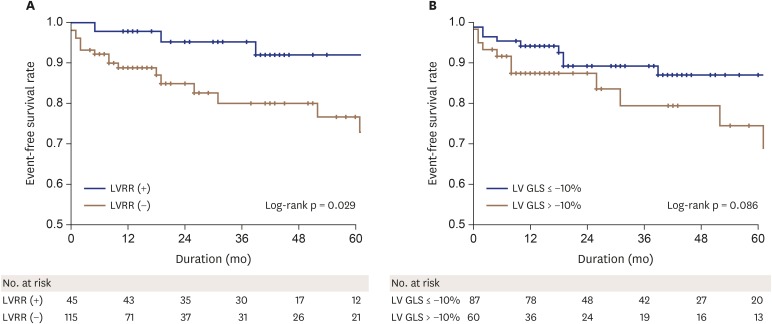
During the mean follow-up duration of 37.3 ± 21.7 months, LVRR occurred in 28% of patients (n = 45). The initial LV ejection fraction (LVEF) of patients who recovered LV function was 26.1 ± 7.9%, which was not significantly different from the value of 27.1 ± 7.4% (p = 0.49) in those who did not recover. There was a moderate and highly significant correlation between baseline LV GLS (−%) and follow-up LVEF (r = 0.717; p < 0.001). Using multivariate Cox analysis, LV GLS (hazard ratio: 1.474, 95% confidence interval: 1.170-1.856; p = 0.001) was an independent predictor of LVRR.
CONCLUSIONS
We demonstrated that LV GLS was an independent predictor for LVRR and the optimal cut-off point of LV GLS for LVRR was −10% in DCM patients with sinus rhythm. There was a significant correlation between baseline LV GLS and follow-up LVEF.
Figure
Reference
-
1. Maron BJ, Towbin JA, Thiene G, et al. Contemporary definitions and classification of the cardiomyopathies: an American Heart Association Scientific Statement from the Council on Clinical Cardiology, Heart Failure and Transplantation Committee; Quality of Care and Outcomes Research and Functional Genomics and Translational Biology Interdisciplinary Working Groups; and Council on Epidemiology and Prevention. Circulation. 2006; 113:1807–1816. PMID: 16567565.2. Merlo M, Pyxaras SA, Pinamonti B, Barbati G, Di Lenarda A, Sinagra G. Prevalence and prognostic significance of left ventricular reverse remodeling in dilated cardiomyopathy receiving tailored medical treatment. J Am Coll Cardiol. 2011; 57:1468–1476. PMID: 21435516.3. Merlo M, Caiffa T, Gobbo M, Adamo L, Sinagra G. Reverse remodeling in dilated cardiomyopathy: Insights and future perspectives. Int J Cardiol Heart Vasc. 2018; 18:52–57. PMID: 29876504.4. Cicoira M, Zanolla L, Latina L, et al. Frequency, prognosis and predictors of improvement of systolic left ventricular function in patients with ‘classical’ clinical diagnosis of idiopathic dilated cardiomyopathy. Eur J Heart Fail. 2001; 3:323–330. PMID: 11378003.5. Smiseth OA, Torp H, Opdahl A, Haugaa KH, Urheim S. Myocardial strain imaging: how useful is it in clinical decision making? Eur Heart J. 2016; 37:1196–1207. PMID: 26508168.6. Adamo L, Perry A, Novak E, Makan M, Lindman BR, Mann DL. Abnormal global longitudinal strain predicts future deterioration of left ventricular function in heart failure patients with a recovered left ventricular ejection fraction. Circ Heart Fail. 2017; 10:e003788. PMID: 28559418.7. Matsumoto K, Tanaka H, Onishi A, et al. Bi-ventricular contractile reserve offers an incremental prognostic value for patients with dilated cardiomyopathy. Eur Heart J Cardiovasc Imaging. 2015; 16:1213–1223. PMID: 25851330.8. Lang RM, Badano LP, Mor-Avi V, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015; 28:1–39.e14. PMID: 25559473.9. Kang DH, Park SJ, Shin SH, et al. Angiotensin receptor neprilysin inhibitor for functional mitral regurgitation. Circulation. 2019; 139:1354–1365. PMID: 30586756.10. Lang RM, Badano LP, Mor-Avi V, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging. 2015; 16:233–270. PMID: 25712077.11. Rudski LG, Lai WW, Afilalo J, et al. Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr. 2010; 23:685–713. quiz 786-8. PMID: 20620859.12. Stevenson LW. Heart failure with better ejection fraction: a modern diagnosis. Circulation. 2014; 129:2364–2367. PMID: 24799514.13. Punnoose LR, Givertz MM, Lewis EF, Pratibhu P, Stevenson LW, Desai AS. Heart failure with recovered ejection fraction: a distinct clinical entity. J Card Fail. 2011; 17:527–532. PMID: 21703523.14. Marwick TH. Measurement of strain and strain rate by echocardiography: ready for prime time? J Am Coll Cardiol. 2006; 47:1313–1327. PMID: 16580516.15. Mirea O, Pagourelias ED, Duchenne J, et al. Intervendor differences in the accuracy of detecting regional functional abnormalities: a report from the EACVI-ASE Strain Standardization Task Force. JACC Cardiovasc Imaging. 2018; 11:25–34. PMID: 28528162.16. Sugimoto T, Dulgheru R, Bernard A, et al. Echocardiographic reference ranges for normal left ventricular 2D strain: results from the EACVI NORRE study. Eur Heart J Cardiovasc Imaging. 2017; 18:833–840. PMID: 28637227.17. Yip G, Abraham T, Belohlavek M, Khandheria BK. Clinical applications of strain rate imaging. J Am Soc Echocardiogr. 2003; 16:1334–1342. PMID: 14652617.18. Ishizu T, Seo Y, Kameda Y, et al. Left ventricular strain and transmural distribution of structural remodeling in hypertensive heart disease. Hypertension. 2014; 63:500–506. PMID: 24396022.19. Park JJ, Park JB, Park JH, Cho GY. Global longitudinal strain to predict mortality in patients with acute heart failure. J Am Coll Cardiol. 2018; 71:1947–1957. PMID: 29724346.20. Pauschinger M, Knopf D, Petschauer S, et al. Dilated cardiomyopathy is associated with significant changes in collagen type I/III ratio. Circulation. 1999; 99:2750–2756. PMID: 10351968.21. Hundley WG, Bluemke DA, Finn JP, et al. ACCF/ACR/AHA/NASCI/SCMR 2010 expert consensus document on cardiovascular magnetic resonance: a report of the American College of Cardiology Foundation Task Force on Expert Consensus Documents. Circulation. 2010; 121:2462–2508. PMID: 20479157.22. Stirrat J, White JA. The prognostic role of late gadolinium enhancement magnetic resonance imaging in patients with cardiomyopathy. Can J Cardiol. 2013; 29:329–336. PMID: 23439019.23. White JA, Patel MR. The role of cardiovascular MRI in heart failure and the cardiomyopathies. Magn Reson Imaging Clin N Am. 2007; 15:541–564. viPMID: 17976591.24. Hoffmann R, Altiok E, Friedman Z, Becker M, Frick M. Myocardial deformation imaging by two-dimensional speckle-tracking echocardiography in comparison to late gadolinium enhancement cardiac magnetic resonance for analysis of myocardial fibrosis in severe aortic stenosis. Am J Cardiol. 2014; 114:1083–1088. PMID: 25212549.25. Pritchett AM, Mahoney DW, Jacobsen SJ, Rodeheffer RJ, Karon BL, Redfield MM. Diastolic dysfunction and left atrial volume: a population-based study. J Am Coll Cardiol. 2005; 45:87–92. PMID: 15629380.26. Dini FL, Cortigiani L, Baldini U, et al. Prognostic value of left atrial enlargement in patients with idiopathic dilated cardiomyopathy and ischemic cardiomyopathy. Am J Cardiol. 2002; 89:518–523. PMID: 11867034.27. Rossi A, Cicoira M, Zanolla L, et al. Determinants and prognostic value of left atrial volume in patients with dilated cardiomyopathy. J Am Coll Cardiol. 2002; 40:1425. PMID: 12392832.28. Lee HH, Lee MK, Lee WH, et al. Atrial fibrillation per se was a major determinant of global left ventricular longitudinal systolic strain. Medicine (Baltimore). 2016; 95:e4038. PMID: 27368031.29. Umana E, Solares CA, Alpert MA. Tachycardia-induced cardiomyopathy. Am J Med. 2003; 114:51–55. PMID: 12543289.30. Seo J, Jung IH, Park JH, et al. The prognostic value of 2D strain in assessment of the right ventricle in patients with dilated cardiomyopathy. Eur Heart J Cardiovasc Imaging. 2019; 20:1043–1050. PMID: 30796431.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Left Ventricular Dysfunction and Dilated Cardiomyopathy in Infants and Children with Wolff-Parkinson-White Syndrome in the Absence of Tachyarrhythmias
- Prognostic Implications of Left Ventricular Global Longitudinal Strain in Dilated Cardiomyopathy
- Hemodynamics and Left Ventricular Cineangiographic Findings in Idiopathic Dilated Cardiomyopathy
- A Study of Left Ventricular Function by Digitized Echocardiograms in Dilated Cardiomyopathy
- Alterations in Left Ventricular Circumferential Motion in Children with Dilated Cardiomyopathy