Korean J Gastroenterol.
2020 Nov;76(5):246-250. 0000-0002-9018-9454.
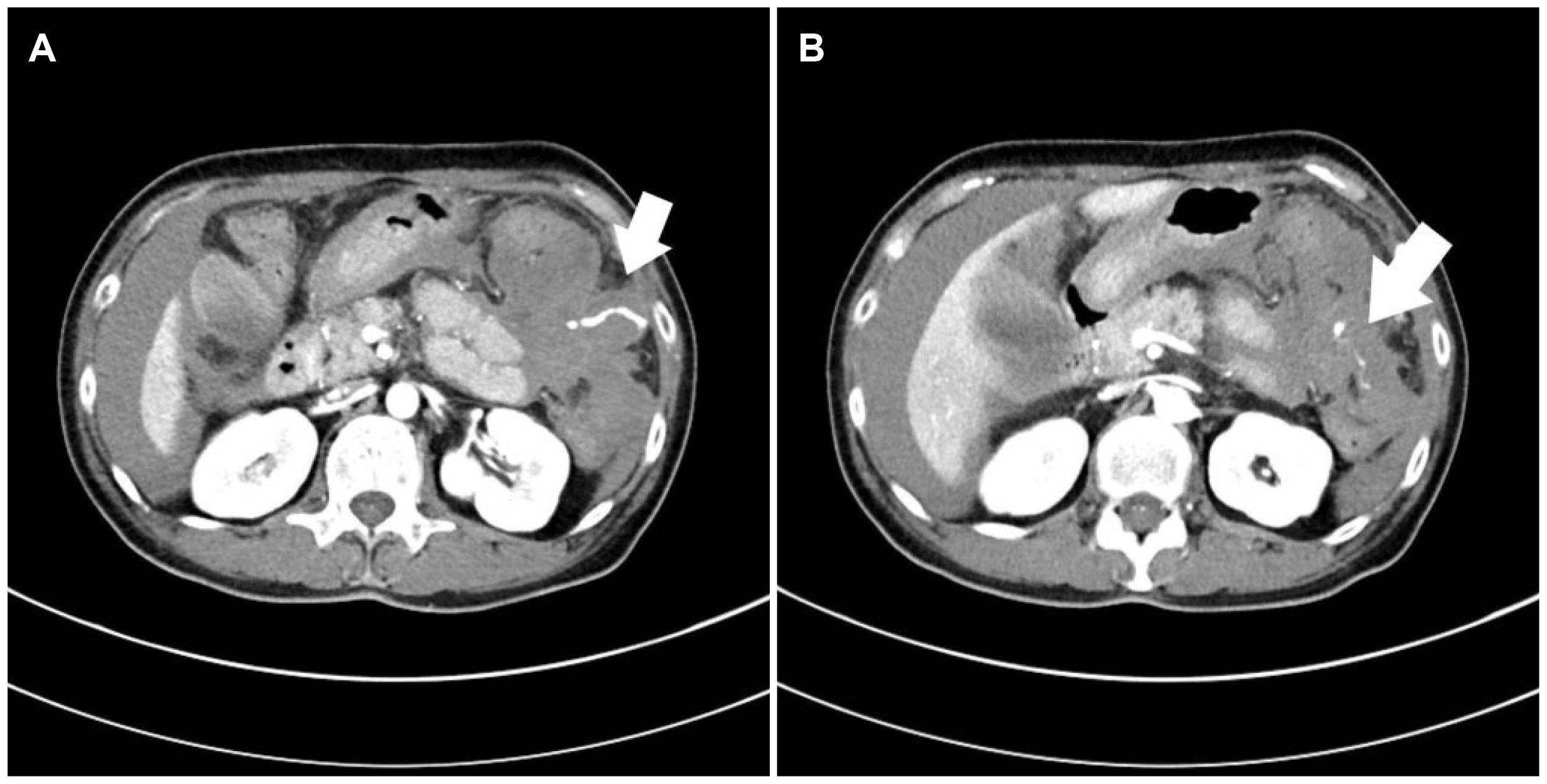
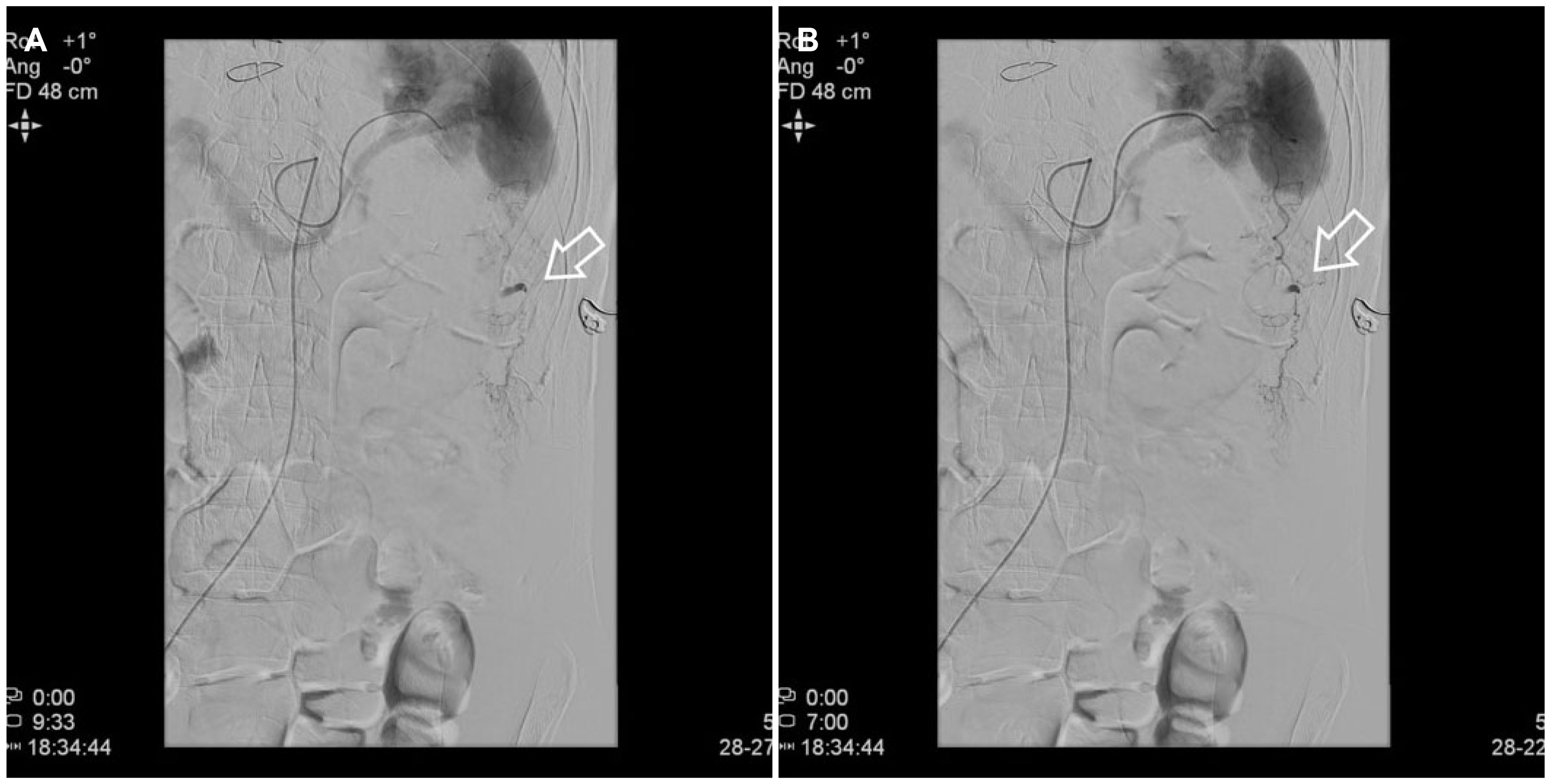
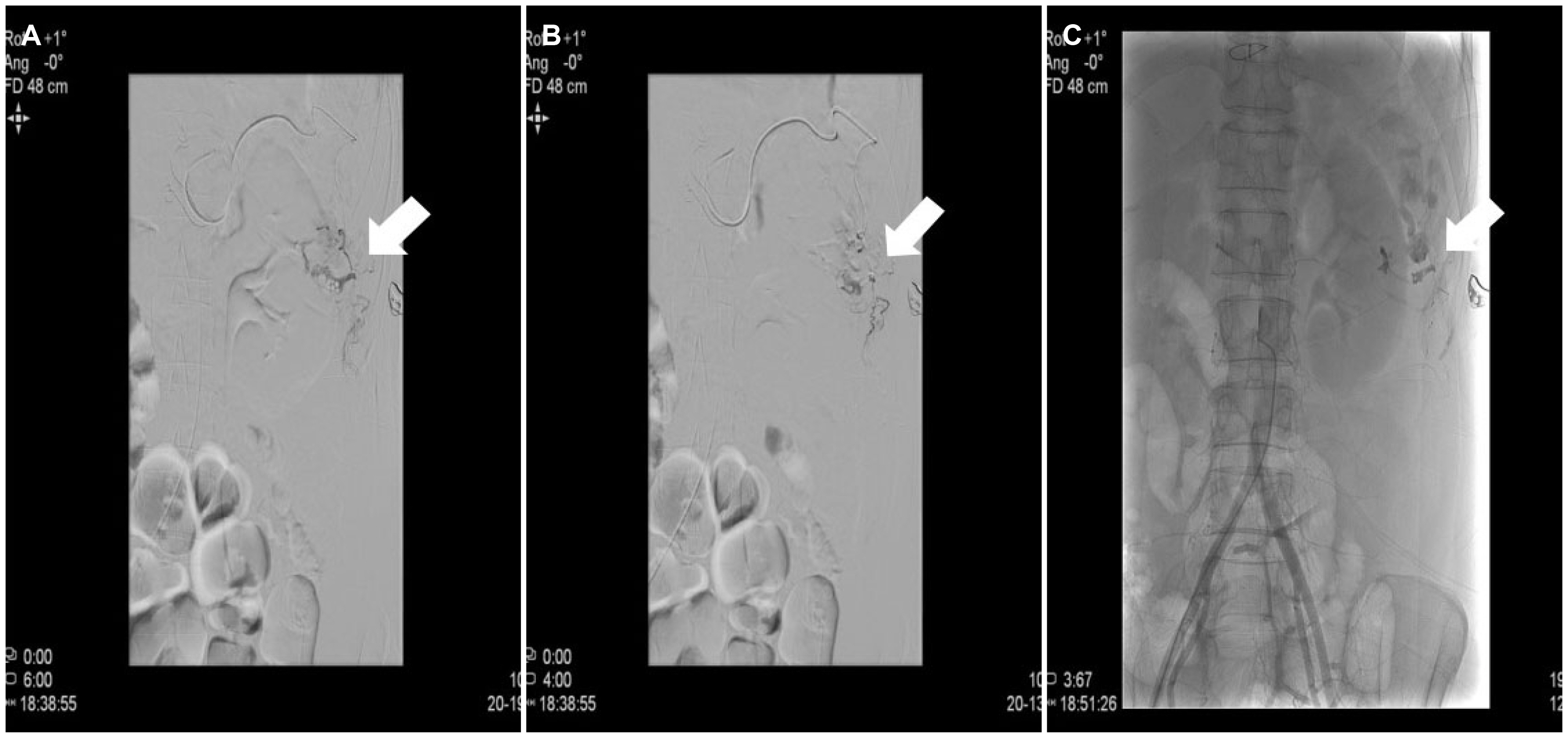
Hemoperitoneum with Splenic Artery Rupture Following Diagnostic Colonoscopy
- Affiliations
-
- 1Division of Gastroenterology, Department of Internal Medicine, Dong-A University Hospital, Busan, Korea
- KMID: 2508874
- DOI: http://doi.org/0000-0002-9018-9454
Abstract
- Colonoscopy is a safe and extremely popular diagnostic and therapeutic procedure. The most common complications are bleeding and perforation. Hemoperitoneum is a rare complication after a colonoscopy and is usually associated with splenic injury or solid organ pathology. This is potentially serious and can be life threatening. With the increasing number of colonoscopies performed, there has also been an increasing trend in reports of rare complications, such as pneumothorax, pneumomediastinum, appendicitis, small bowel perforation, septicemia, mesenteric tear, retroperitoneal abscess, and hemoperitoneum. This paper reports a unique case of hemoperitoneum after a recent colonoscopy without a splenic rupture or intra-abdominal abnormality, or external trauma. Most hemoperitoneum occurs within 48 hours after the inciting colonoscopy. In the present case, however, hemoperitoneum appeared 10 days after the colonoscopy. This case emphasizes that physicians should consider hemoperitoneum in a differential diagnosis of abdominal pain in patients after colonoscopy.
Keyword
Figure
Reference
-
1. Zhang AN, Sherigar JM, Guss D, Mohanty SR. 2018; A delayed presentation of splenic laceration and hemoperitoneum following an elective colonoscopy: a rare complication with uncertain risk factors. SAGE Open Med Case Rep. 6:2050313X18791069. DOI: 10.1177/2050313X18791069. PMID: 30083323. PMCID: PMC6066810.
Article2. Church J. 2013; Complications of colonoscopy. Gastroenterol Clin North Am. 42:639–57. DOI: 10.1016/j.gtc.2013.05.003. PMID: 23931864.
Article3. Ha JF, Minchin D. 2009; Splenic injury in colonoscopy: a review. Int J Surg. 7:424–427. DOI: 10.1016/j.ijsu.2009.07.010. PMID: 19638324.
Article4. Saad A, Rex DK. 2008; Colonoscopy-induced splenic injury: report of 3 cases and literature review. Dig Dis Sci. 53:892–898. DOI: 10.1007/s10620-007-9963-5. PMID: 17934832.
Article5. Castelli M. 1986; Splenic rupture: an unusual late complication of colonoscopy. CMAJ. 134:916–917. PMID: 3955487. PMCID: PMC1490946.6. Kwon A, Kim CW, Lee KE, et al. 2013; A case of spontaneous hemoperitoneum without spleen injury after a diagnostic colonoscopy. Korean J Med. 85:178–182. DOI: 10.3904/kjm.2013.85.2.178.
Article7. Wherry DC, Zehner H Jr. 1974; Colonoscopy-fiberoptic endoscopic approach to the colon and polypectomy. Med Ann Dist Columbia. 43:189–192. PMID: 4524804.8. Tagg W, Woods S, Razdan R, Gagliardi J, Steenbergen P. 2008; Hemoperitoneum after colonoscopy. Endoscopy. 40 Suppl 2:E136–E137. DOI: 10.1055/s-2007-995715. PMID: 18633865.
Article9. García-Martos E, Vara-Brenes D, Prados-Manzano R, Joya-Vázquez PP, Molina-Infante J. 2015; Hemoperitoneum: a rare complication after diagnostic colonoscopy. Gastroenterol Hepatol. 38:409–410. DOI: 10.1016/j.gastrohep.2014.09.001. PMID: 25767000.10. Salvador Milian E, Lorente Perez S, Arroyo Villarino MT, Sainz Samitier R. 1999; Hemoperitoneum as a complication of diagnostic colonoscopy. Gastroenterol Hepatol. 22:377. PMID: 10535213.11. Olshaker JS, Deckleman C. 1999; Delayed presentation of splenic rupture after colonoscopy. J Emerg Med. 17:455–457. DOI: 10.1016/S0736-4679(99)00040-2. PMID: 10338238.
Article12. Viamonte M, Wulkan M, Irani H. 1992; Splenic trauma as a complication of colonoscopy. Surg Laparosc Endosc. 2:154–157. DOI: 10.1097/00129689-199206000-00017. PMID: 1341527.
Article13. Fishback SJ, Pickhardt PJ, Bhalla S, Menias CO, Congdon RG, Macari M. 2011; Delayed presentation of splenic rupture following colonoscopy: clinical and CT findings. Emerg Radiol. 18:539–544. DOI: 10.1007/s10140-011-0982-3. PMID: 21887533.
Article14. Baek JB, Seong SH, Won DY, Bae KS, Kim IY. 2010; Spontaneous hemoperitoneum in patients taking anticoagulants. J Korean Surg Soc. 78:369–375. DOI: 10.4174/jkss.2010.78.6.369.
Article15. Demir MV, Demir TÖ, Yaylaci S, Genc AB. 2016; Spontaneous abdominal hemorrhage due to warfarin treatment. CHRISMED J Health Res. 3:298–300. DOI: 10.4103/2348-3334.190571.
Article16. Hylek EM, Singer DE. 1994; Risk factors for intracranial hemorrhage in outpatients taking warfarin. Ann Intern Med. 120:897–902. DOI: 10.7326/0003-4819-120-11-199406010-00001. PMID: 8172435.
Article17. Schulman S. 2003; Clinical practice. Care of patients receiving long-term anticoagulant therapy. N Engl J Med. 349:675–683. DOI: 10.1056/NEJMcp025373. PMID: 12917305.18. Garbay JR, Suc B, Rotman N, Fourtanier G, Escat J. 1996; Multicentre study of surgical complications of colonoscopy. Br J Surg. 83:42–44. DOI: 10.1002/bjs.1800830112. PMID: 8653359.
Article19. Eisen GM, Baron TH, Dominitz JA, et al. 2002; Guideline on the management of anticoagulation and antiplatelet therapy for endoscopic procedures. Gastrointest Endosc. 55:775–779. DOI: 10.1016/S0016-5107(02)70402-1. PMID: 12024126.
Article20. Reissman P, Durst AL. 1998; Splenic hematoma. A rare complication of colonoscopy. Surg Endosc. 12:154–155. DOI: 10.1007/s004649900618. PMID: 9479732.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Splenic Rupture following Colon Polypectomy: A Case Report and Review of Literature
- Spontaneous Rupture of a Primary Splenic Cyst Causing Hemoperitoneum
- A Case of Spontaneous Hemoperitoneum without Spleen Injury after a Diagnostic Colonoscopy
- Splenic artery aneurysm with the double-rupture phenomenon
- Aneurysm of Splenic Artery: A Case Report