Ann Hepatobiliary Pancreat Surg.
2020 Nov;24(4):445-453. 10.14701/ahbps.2020.24.4.445.
Portal vein reconstruction using side-to-side unification technique for infant-to-infant deceased donor whole liver transplantation
- Affiliations
-
- 1Departments of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 2Departments of Pediatrics, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2508853
- DOI: http://doi.org/10.14701/ahbps.2020.24.4.445
Abstract
- Backgrounds/Aims
Infant-to-infant whole liver transplantation (I2I-WLT) has been rarely performed in Korea. We analyze clinical sequences of our 7 cases of I2I-WLT and present evolution of surgical techniques to prevent PV stenosis.
Methods
A total of 7 cases of I2I-WLT were performed at our institution during last 13 years, which represented 0.1% of our LT volume. Patient perioperative profiles and clinical sequences were analyzed with focusing on portal vein (PV) complications.
Results
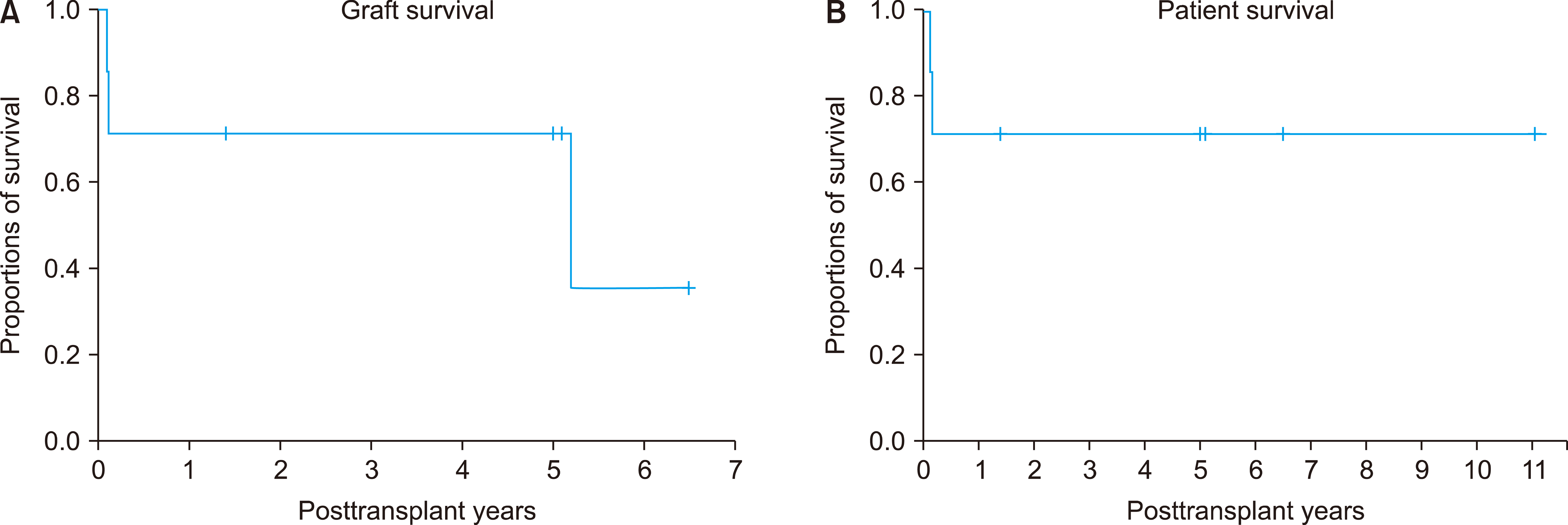
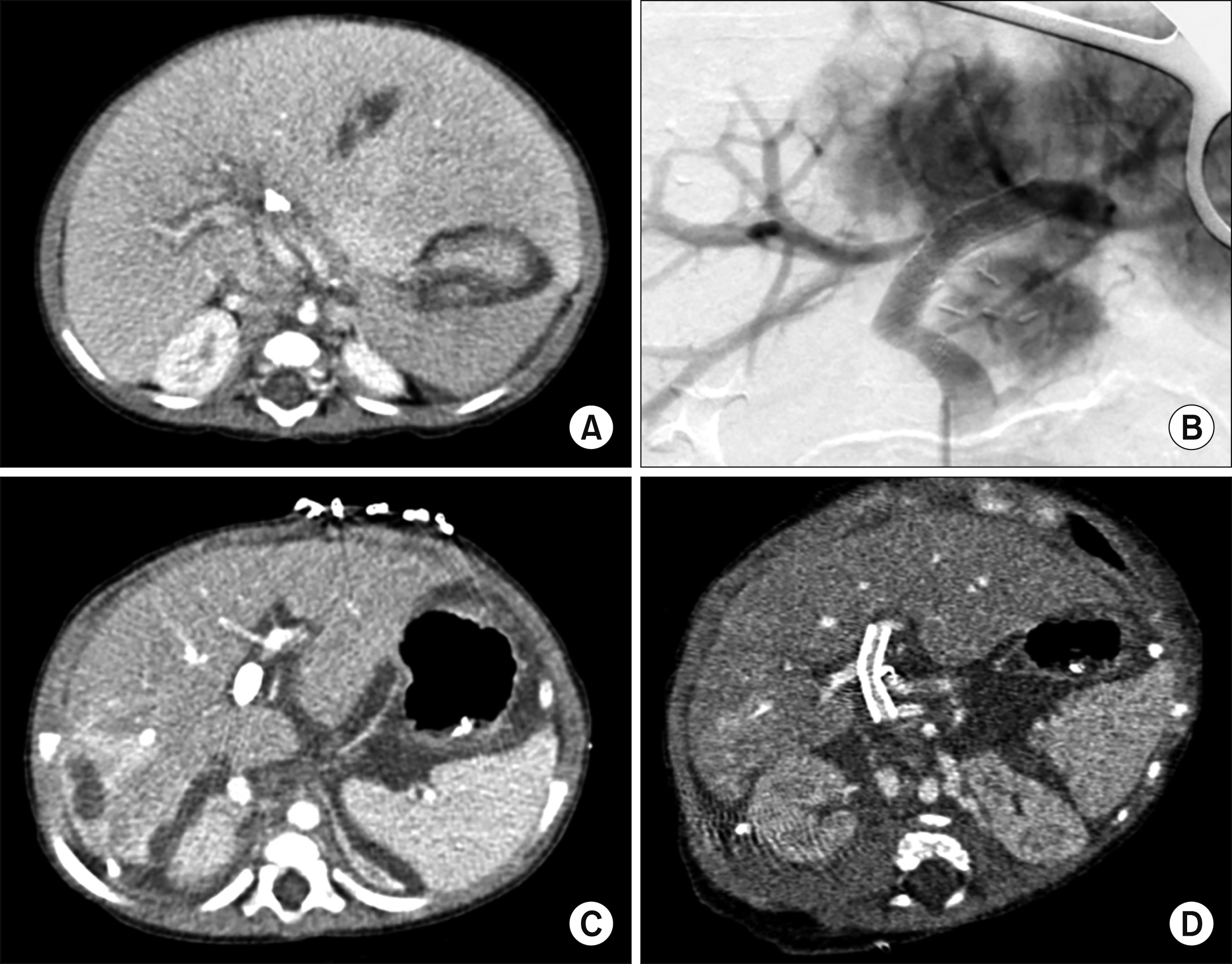
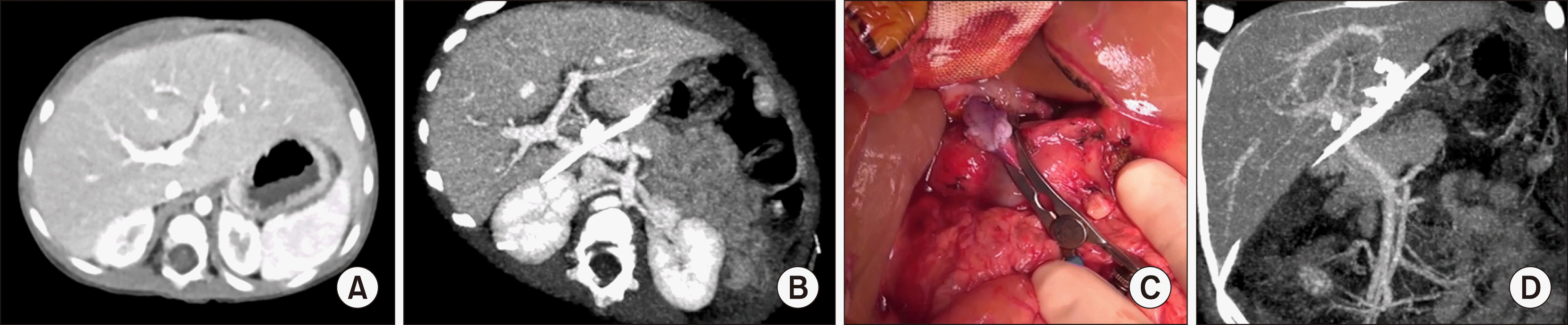
Donor ages were 6-17 months and graft weights were 140-525 g. Recipient ages were 7-16 months and body weights were 6-10.1 kg and Primary diagnoses were biliary atresia in 6 and progressive familial intrahepatic cholestasis in 1. The first case underwent PV stenting 2 months after I2I-WLT, and underwent retransplantation 6 years later. The second case underwent intraoperative PV stenting, but died 32 days later. The third case underwent repeated PV dilatation. The fourth, fifth and seventh cases experienced no surgical complications, and PV reconstruction was performed using a side-to-side unification venoplasty technique. The sixth case had poor development of the PV system, so customized PV venoplasty was performed, but PV occlusion requiring PV stenting occurred. Early retransplantation was performed, but scanty PV flow was detected despite no obvious PV stenosis, resulting in graft failure. Serious PV complications developed in 4, but none experienced after adoption of side-to-side unification venoplasty.
Conclusions
As PV size in infant donors and recipients is very small, PV reconstruction in I2I-WLT requires specialized surgical techniques of side-to-side unification venoplasty.
Figure
Cited by 1 articles
-
Pediatric deceased donor liver transplantation with
in situ size reduction for recipient-graft size matching
Jung-Man Namgoong, Shin Hwang, Dae-Yeon Kim, Tae-Yong Ha, Gi-Won Song, Dong-Hwan Jung, Kyung Mo Kim, Seak Hee Oh
Ann Hepatobiliary Pancreat Surg. 2021;25(3):431-435. doi: 10.14701/ahbps.2021.25.3.431.
Reference
-
1. Moon DB, Lee SG, Hwang S, Kim KH, Ahn CS, Ha TY, et al. 2013; Toward more than 400 liver transplantations a year at a single center. Transplant Proc. 45:1937–1941. DOI: 10.1016/j.transproceed.2012.12.015. PMID: 23769078.
Article2. Oh SH, Kim KM, Kim DY, Song SM, Kim T, Hwang S, et al. 2012; Clinical experience of more than 200 cases of pediatric liver transplantation at a single center: improved patient survival. Transplant Proc. 44:484–486. DOI: 10.1016/j.transproceed.2012.02.002. PMID: 22410052.
Article3. Hwang S, Kim DY, Ahn CS, Moon DB, Kim KM, Park GC, et al. 2013; Computational simulation-based vessel interposition reconstruction technique for portal vein hypoplasia in pediatric liver transplantation. Transplant Proc. 45:255–258. DOI: 10.1016/j.transproceed.2012.05.090. PMID: 23375311.
Article4. Mitchell A, John PR, Mayer DA, Mirza DF, Buckels JA, De Ville De Goyet J. 2002; Improved technique of portal vein reconstruction in pediatric liver transplant recipients with portal vein hypoplasia. Transplantation. 73:1244–1247. DOI: 10.1097/00007890-200204270-00009. PMID: 11981415.
Article5. Takahashi Y, Nishimoto Y, Matsuura T, Hayashida M, Tajiri T, Soejima Y, et al. 2009; Surgical complications after living donor liver transplantation in patients with biliary atresia: a relatively high incidence of portal vein complications. Pediatr Surg Int. 25:745–751. DOI: 10.1007/s00383-009-2430-y. PMID: 19655151.
Article6. Ueda M, Egawa H, Ogawa K, Uryuhara K, Fujimoto Y, Kasahara M, et al. 2005; Portal vein complications in the long-term course after pediatric living donor liver transplantation. Transplant Proc. 37:1138–1140. DOI: 10.1016/j.transproceed.2005.01.044. PMID: 15848648.
Article7. Gurusamy KS, Pamecha V, Davidson BR. 2011; Piggy-back graft for liver transplantation. Cochrane Database Syst Rev. (1):CD008258. DOI: 10.1002/14651858.CD008258.pub2. PMID: 21249703.
Article8. Jovine E, Mazziotti A, Grazi GL, Ercolani G, Masetti M, Morganti M, et al. 1997; Piggy-back versus conventional technique in liver transplantation: report of a randomized trial. Transpl Int. 10:109–112. DOI: 10.1111/j.1432-2277.1997.tb00550.x. PMID: 9089994.
Article9. Namgoong JM, Hwang S, Ahn CS, Jung DH, Park GC. 2020; Side-to-side portal vein reconstruction for infant-to-infant deceased donor whole liver transplantation: report of 2 cases with video. Ann Hepatobiliary Pancreat Surg. 24:301–304. DOI: 10.14701/ahbps.2020.24.3.301. PMID: 32843595. PMCID: PMC7452795.
Article10. Sakamoto S, Kanazawa H, Shigeta T, Uchida H, Sasaki K, Hamano I, et al. 2014; Technical considerations of living donor hepatectomy of segment 2 grafts for infants. Surgery. 156:1232–1237. DOI: 10.1016/j.surg.2014.05.003. PMID: 24909347.
Article11. Kasahara M, Sakamoto S, Umeshita K, Uemoto S. 2014; Effect of graft size matching on pediatric living-donor liver transplantation in Japan. Exp Clin Transplant. 12(Suppl 1):1–4. DOI: 10.6002/ect.25Liver.L5. PMID: 24635782.
Article12. Kasahara M, Umeshita K, Sakamoto S, Fukuda A, Furukawa H, Uemoto S. 2017; Liver transplantation for biliary atresia: a systematic review. Pediatr Surg Int. 33:1289–1295. DOI: 10.1007/s00383-017-4173-5. PMID: 28983725.
Article13. Gu LH, Fang H, Li FH, Zhang SJ, Han LZ, Li QG. 2015; Preoperative hepatic hemodynamics in the prediction of early portal vein thrombosis after liver transplantation in pediatric patients with biliary atresia. Hepatobiliary Pancreat Dis Int. 14:380–385. DOI: 10.1016/S1499-3872(15)60377-0. PMID: 26256082.
Article14. Yeh YT, Chen CY, Tseng HS, Wang HK, Tsai HL, Lin NC, et al. 2017; Enlarging vascular stents after pediatric liver transplantation. J Pediatr Surg. 52:1934–1939. DOI: 10.1016/j.jpedsurg.2017.08.060. PMID: 28927979.
Article15. Ko GY, Sung KB, Lee S, Yoon HK, Kim KR, Kim KM, et al. 2007; Stent placement for the treatment of portal vein stenosis or occlusion in pediatric liver transplant recipients. J Vasc Interv Radiol. 18:1215–1221. DOI: 10.1016/j.jvir.2007.06.029. PMID: 17911510.
Article16. Yabuta M, Shibata T, Shibata T, Shinozuka K, Isoda H, Okamoto S, et al. 2014; Long-term outcome of percutaneous transhepatic balloon angioplasty for portal vein stenosis after pediatric living donor liver transplantation: a single institute's experience. J Vasc Interv Radiol. 25:1406–1412. DOI: 10.1016/j.jvir.2014.03.034. PMID: 24854391.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Side-to-side portal vein reconstruction for infant-to-infant deceased donor whole liver transplantation: Report of 2 cases with video
- Tailored standardization of portal vein reconstruction for pediatric liver transplantation at Asan Medical Center
- End-to-side jump graft from superior mesenteric vein for portal vein reconstruction in pediatric liver transplantation: a case report
- Tailored techniques of graft outflow vein reconstruction in pediatric liver transplantation at Asan Medical Center
- Standardized surgical techniques for adult living donor liver transplantation using a modified right lobe graft: a video presentation from bench to reperfusion