J Korean Neurosurg Soc.
2020 Nov;63(6):730-737. 10.3340/jkns.2020.0007.
The Influence of Comorbidities on Reoperations Following Primary Surgery of Lumbar Degenerative Diseases : A Nationwide Population-Based Retrospective Cohort Study from 2009–2016
- Affiliations
-
- 1Department of Neurosurgery, Soonchunhyang University Hospital, Seoul, Korea
- 2Department of Biostatistics, Soonchunhyang University Hospital, Seoul, Korea
- 3Healthcare Data Convergence Department, Health Insurance Review & Assessment Service, Wonju, Korea
- KMID: 2508603
- DOI: http://doi.org/10.3340/jkns.2020.0007
Abstract
Objective
: Spinal degeneration is a progressive disease, worsening over time. Lumbar degenerative disease (LDD) is a major spinal disease in elderly patients. Surgical treatment is considered for medically intractable patients with LDD and reoperation after primary surgery is not uncommon. The surgical outcome is occasionally unpredictable because of comorbidities. In the present study, the relationship between comorbidities and the incidence of reoperation for LDD over time was determined.
Methods
: The claims data of the health insurance national database were used to identify a cohort of patients who underwent spinal surgery for LDD in 2009. The patients were followed up until 2016. Medical comorbidity was assessed according to the Charlson comorbidity index (CCI). Cox proportional hazard regression modeling was used to identify significant differences in sex, surgery, age, causative disease, and comorbidity.
Results
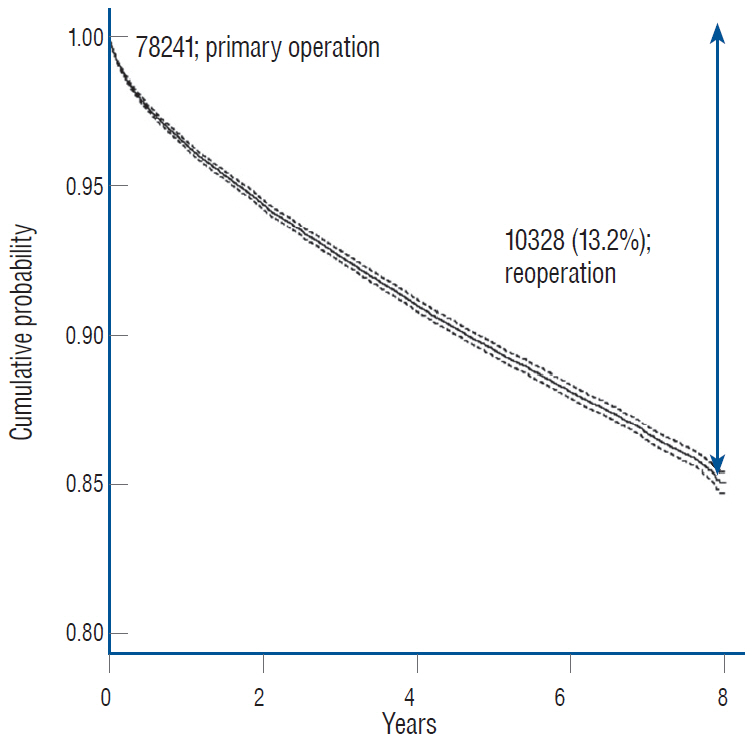
: The study cohort included 78241 patients; 10328 patients (13.2%) underwent reoperation during the observation period. The reoperation rate was statistically higher (p<0.01) in males, patients 55–74 years and 65–74 years of age, and patients with decompression or discectomy. Significant association was found between increasing reoperation rate and CCI score (p<0.01). Based on multivariate analysis of comorbidities, the significantly higher reoperation rates were observed in patients with peripheral vascular disease, pulmonary lung disease, peptic ulcer, diabetes, and diabetes complications (p<0.01).
Conclusion
: The study results indicate the reoperation rate for LDD is associated with patient comorbidities. The comorbidities identified in this study could be helpful in future LDD studies.
Figure
Reference
-
References
1. Alpantaki K, Kampouroglou A, Koutserimpas C, Effraimidis G, Hadjipavlou A. Diabetes mellitus as a risk factor for intervertebral disc degeneration: a critical review. Eur Spine J. 28:2129–2144. 2019.
Article2. Alvarez-Garcia O, Matsuzaki T, Olmer M, Masuda K, Lotz MK. Age-related reduction in the expression of FOXO transcription factors and correlations with intervertebral disc degeneration. J Orthop Res. 35:2682–2691. 2017.
Article3. Boukhenouna S, Wilson MA, Bahmed K, Kosmider B. Reactive oxygen species in chronic obstructive pulmonary disease. Oxid Med Cell Longev. 2018:5730395. 2018.
Article4. Chen Z, Xie P, Feng F, Chhantyal K, Yang Y, Rong L. Decompression alone versus decompression and fusion for lumbar degenerative spondylolisthesis: a meta-analysis. World Neurosurg. 111:e165–e177. 2018.
Article5. Cheng CY, Cheng YC, Wang TC, Yang WH. Fusion Techniques are related to a lower risk of reoperation in lumbar disc herniation: a 5-year observation study of a nationwide cohort in Taiwan. World Neurosurg. 117:e660–e668. 2018.
Article6. Cheung PWH, Fong HK, Wong CS, Cheung JPY. The influence of developmental spinal stenosis on the risk of re-operation on an adjacent segment after decompression-only surgery for lumbar spinal stenosis. Bone Joint J. 101-B:154–161. 2019.
Article7. El Shahawy MS, Hemida MH, El Metwaly I, Shady ZM. The effect of vitamin D deficiency on eradication rates of Helicobacter pylori infection. JGH Open. 2:270–275. 2018.
Article8. Fabiane SM, Ward KJ, Iatridis JC, Williams FM. Does type 2 diabetes mellitus promote intervertebral disc degeneration? Eur Spine J. 25:2716–2720. 2016.
Article9. Feng Y, Egan B, Wang J. Genetic factors in intervertebral disc degeneration. Genes Dis. 3:178–185. 2016.
Article10. Gerling MC, Leven D, Passias PG, Lafage V, Bianco K, Lee A, et al. Risk factors for reoperation in patients treated surgically for degenerative spondylolisthesis: a subanalysis of the 8-year data from the SPORT trial. Spine (Phila Pa 1976). 42:1559–1569. 2017.
Article11. Gordon M, Stark A, Sköldenberg OG, Kärrholm J, Garellick G. The influence of comorbidity scores on re-operations following primary total hip replacement: comparison and validation of three comorbidity measures. Bone Joint J. 95-B:1184–1191. 2013.12. Hong X, Liu L, Bao J, Shi R, Fan Y, Wu X. Characterization and risk factor analysis for reoperation after microendoscopic diskectomy. Orthopedics. 38:e490–e496. 2015.
Article13. Huang H, Cheng S, Zheng T, Ye Y, Ye A, Zhu S, et al. Vitamin D retards intervertebral disc degeneration through inactivation of the NF-κB pathway in mice. Am J Transl Res. 11:2496–2506. 2019.14. Kim CH, Chung CK, Shin S, Choi BR, Kim MJ, Park BJ, et al. The relationship between diabetes and the reoperation rate after lumbar spinal surgery: a nationwide cohort study. Spine J. 15:866–874. 2015.
Article15. Kim JA, Yoon S, Kim LY, Kim DS. Towards actualizing the value potential of Korea Health Insurance Review and Assessment (HIRA) data as a resource for health research: strengths, limitations, applications, and strategies for optimal use of HIRA data. J Korean Med Sci. 32:718–728. 2017.
Article16. Kim L, Kim JA, Kim S. A guide for the utilization of Health Insurance Review and Assessment service national patient samples. Epidemiol Health. 36:e2014008. 2014.
Article17. Liu C, Zhang JF, Sun ZY, Tian JW. Bioinformatics analysis of the gene expression profiles in human intervertebral disc degeneration associated with inflammatory cytokines. J Neurosurg Sci. 62:16–23. 2018.
Article18. Ma K, Chen S, Li Z, Deng X, Huang D, Xiong L, et al. Mechanisms of endogenous repair failure during intervertebral disc degeneration. Osteoarthritis Cartilage. 27:41–48. 2019.
Article19. Radcliff K, Curry P, Hilibrand A, Kepler C, Lurie J, Zhao W, et al. Risk for adjacent segment and same segment reoperation after surgery for lumbar stenosis: a subgroup analysis of the Spine Patient Outcomes Research Trial (SPORT). Spine (Phila Pa 1976). 38:531–539. 2013.
Article20. Sato S, Yagi M, Machida M, Yasuda A, Konomi T, Miyake A, et al. Reoperation rate and risk factors of elective spinal surgery for degenerative spondylolisthesis: minimum 5-year follow-up. Spine J. 15:1536–1544. 2015.
Article21. Sundararajan V, Henderson T, Perry C, Muggivan A, Quan H, Ghali WA. New ICD-10 version of the Charlson comorbidity index predicted inhospital mortality. J Clin Epidemiol. 57:1288–1294. 2004.
Article22. Suzuki S, Fujita N, Hosogane N, Watanabe K, Ishii K, Toyama Y, et al. Excessive reactive oxygen species are therapeutic targets for intervertebral disc degeneration. Arthritis Res Ther. 17:316. 2015.
Article23. Zhang Y, Zhao Y, Wang M, Si M, Li J, Hou Y, et al. Serum lipid levels are positively correlated with lumbar disc herniation--a retrospective study of 790 Chinese patients. Lipids Health Dis. 15:80. 2016.
Article24. Zhong ZM, Deviren V, Tay B, Burch S, Berven SH. Adjacent segment disease after instrumented fusion for adult lumbar spondylolisthesis: incidence and risk factors. Clin Neurol Neurosurg. 156:29–34. 2017.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Clinical Correlations between Diabetes, Cigarette Smoking and Obesity on Intervertebral Degenerative Disc Disease of the Lumbar Spine
- The Causes of Revision Arthrodesis for the Degenerative Changes at the Adjacent Segment after Lumbosacral Fusion for Degenerative Lumbar Diseases
- Principles of Lumbar Spine Stabilization
- Clinical Relationship of Degenerative Changes between the Cervical and Lumbar Spine
- Radiological Evaluation of the Initial Fixation between Cortical Bone Trajectory and Conventional Pedicle Screw Technique for Lumbar Degenerative Spondylolisthesis