Ann Lab Med.
2020 Nov;40(6):474-480. 10.3343/alm.2020.40.6.474.
Absolute Change in High-Sensitivity Cardiac Troponin I at Three Hours After Presentation is Useful for Diagnosing Acute Myocardial Infarction in the Emergency Department
- Affiliations
-
- 1Departments of Emergency Medicine, Konkuk University School of Medicine, Konkuk University Medical Center, Seoul, Korea
- 2Departments of Laboratory Medicine, Konkuk University School of Medicine, Konkuk University Medical Center, Seoul, Korea
- 3Division of Cardiology, Department of Internal Medicine, Konkuk University School of Medicine, Konkuk University Medical Center, Seoul, Korea
- KMID: 2507793
- DOI: http://doi.org/10.3343/alm.2020.40.6.474
Abstract
- Background
A rise and/or fall in cardiac troponin value with at least one value above the 99th percentile upper reference limit is essential for acute myocardial infarction (AMI) diagnosis. We evaluated the clinical usefulness of serial high-sensitivity cardiac troponin I (hs-cTnI) measurements in AMI diagnosis, in terms of the predictability of absolute and relative changes.
Methods
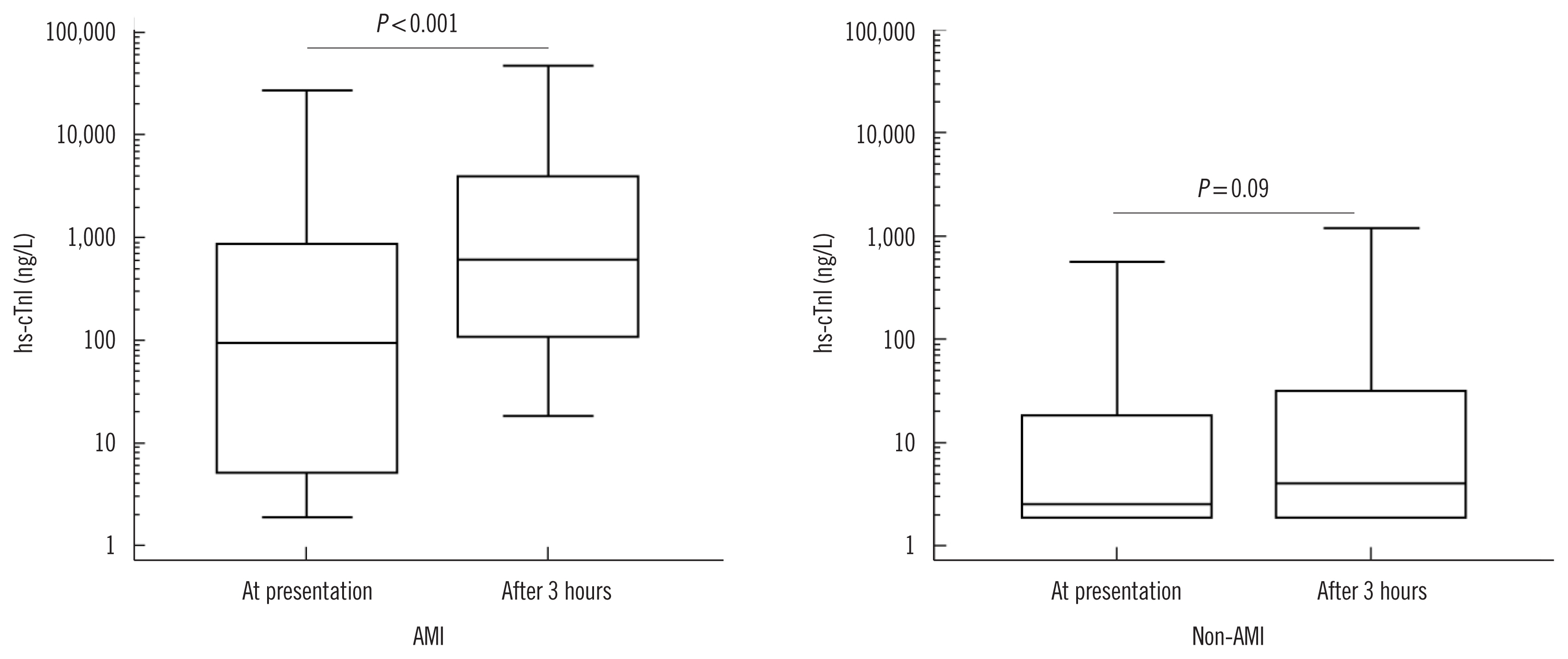
For this retrospective, forward observational study, we enrolled 281 patients older than 18 years who presented with chest pain at the emergency department (ED) between August 2015 and December 2016. The patients were grouped as AMI and nonAMI, and 73 (26%) were diagnosed as having AMI. Hs-cTnI (Abbott Diagnostics, Abbott Park, IL, USA) was measured at presentation and 3 hours later. We assessed the diagnostic performance of the absolute and relative changes in hs-cTnI.
Results
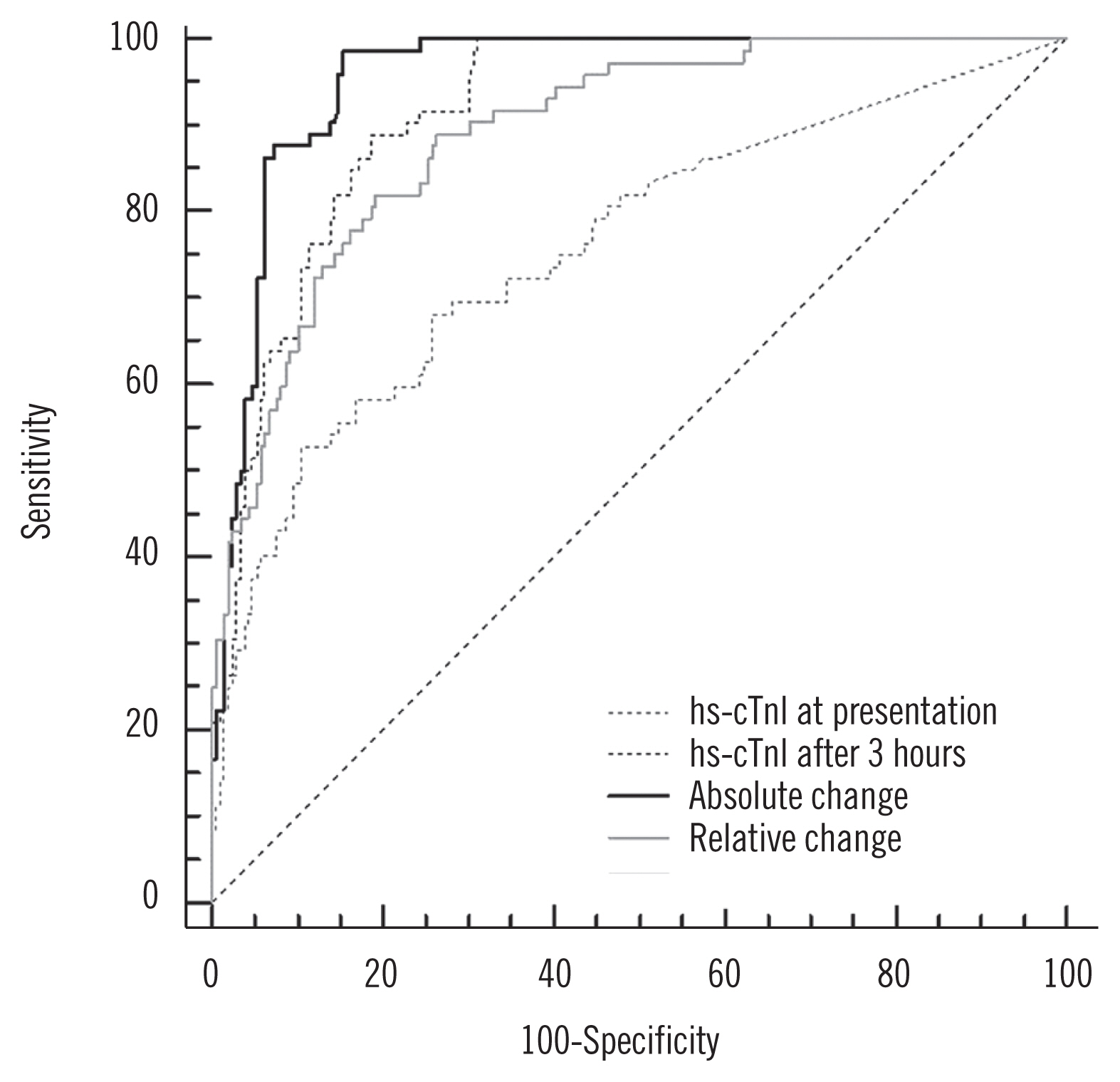
The cut-off values to predict AMI were 16.2 ng/L and 42.1% for the absolute and relative hs-cTnI changes, respectively. The area under the curve of hs-cTnI for AMI diagnosis was larger for absolute changes than for relative changes [0.96 (95% confidence interval [CI], 0.92–0.98) vs 0.89 (95% CI, 0.85–0.93)] (P = 0.014).
Conclusions
The absolute hs-cTnI change at 3 hours after presentation was superior to the relative change, and a rise and/or fall in hs-cTnI of > 16.2 ng/L at 3 hours after presentation was useful to identify AMI in patients presenting at the ED.
Keyword
Figure
Cited by 1 articles
-
Effect of Outlier Elimination on the 99th Percentile Upper Reference Limits of High-Sensitivity Cardiac Troponin I Assays Based on a Strictly Selected Healthy Reference Population
Sunyoung Ahn, Hyun-Ki Kim, Woochang Lee, Sail Chun, Won-Ki Min
Ann Lab Med. 2022;42(3):331-341. doi: 10.3343/alm.2022.42.3.331.
Reference
-
1. Kolansky DM. Acute coronary syndromes: morbidity, mortality, and pharmacoeconomic burden. Am J Manag Care. 2009; 15:S36–41.2. Foley AL. Not just chest pain: presenting symptoms of acute coronary syndrome by gender: A research to practice summary. J Emerg Nurs. 2019; 45:462–4.
Article3. Katus H, Ziegler A, Ekinci O, Giannitsis E, Stough WG, Achenbach S, et al. Early diagnosis of acute coronary syndrome. Eur Heart J. 2017; 38:3049–55.
Article4. Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, et al. Fourth universal definition of myocardial infarction (2018). Circulation. 2018; 138:e618–51.
Article5. Apple FS, Jaffe AS, Collinson P, Mockel M, Ordonez-Llanos J, Lindahl B, et al. IFCC educational materials on selected analytical and clinical applications of high sensitivity cardiac troponin assays. Clin Biochem. 2015; 48:201–3.
Article6. Thygesen K, Mair J, Giannitsis E, Mueller C, Lindahl B, Blankenberg S, et al. How to use high-sensitivity cardiac troponins in acute cardiac care. Eur Heart J. 2012; 33:2252–7.
Article7. Thygesen K, Mair J, Katus H, Plebani M, Venge P, Collinson P, et al. Recommendations for the use of cardiac troponin measurement in acute cardiac care. Eur Heart J. 2010; 31:2197–204.
Article8. Sugiura T, Dohi Y, Takase H, Yamashita S, Mizoguchi T, Fujii S, et al. Close association between circulating high-sensitivity cardiac troponin I and metabolic syndrome in the general population. Hypertens Res. 2019; 42:1768–75.
Article9. Rangaswami J, Bhalla V, Blair JEA, Chang TI, Costa S, Lentine KL, et al. Cardiorenal syndrome: classification, pathophysiology, diagnosis, and treatment strategies: A scientific statement from the American Heart Association. Circulation. 2019; 139:e840–78.
Article10. Ooi DS, Isotalo PA, Veinot JP. Correlation of antemortem serum creatine kinase, creatine kinase-MB, troponin I, and troponin T with cardiac pathology. Clin Chem. 2000; 46:338–44.
Article11. Collinson PO, Apple F, Jaffe AS. Use of troponins in clinical practice: evidence in favour of use of troponins in clinical practice. Heart. 2020; 106:253–5.
Article12. Vasile VC, Jaffe AS. High-sensitivity cardiac troponin for the diagnosis of patients with acute coronary syndromes. Curr Cardiol Rep. 2017; 19:92.
Article13. Roffi M, Patrono C, Collet JP, Mueller C, Valgimigli M, Andreotti F, et al. 2015 ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: task force for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2016; 37:267–315.14. Pickering JW, Greenslade JH, Cullen L, Flaws D, Parsonage W, Aldous S, et al. Assessment of the European Society of Cardiology 0-hour/1-hour algorithm to rule-out and rule-in acute myocardial infarction. Circulation. 2016; 134:1532–41.
Article15. Jaffe AS, Moeckel M, Giannitsis E, Huber K, Mair J, Mueller C, et al. In search for the holy grail: suggestions for studies to define delta changes to diagnose or exclude acute myocardial infarction: a position paper from the study group on biomarkers of the acute cardiovascular care association. Eur Heart J Acute Cardiovasc Care. 2014; 3:313–6.
Article16. Agewall S, Giannitsis E, Jernberg T, Katus H. Troponin elevation in coronary vs. non-coronary disease. Eur Heart J. 2011; 32:404–11.
Article17. Kavsak PA, Ko DT, Wang X, Macrae AR, Jaffe AS. Increasing cardiac troponin changes measured by a research high-sensitivity troponin I assay: absolute vs percentage changes and long-term outcomes in a chest pain cohort. Clin Chem. 2010; 56:1902–4.
Article18. Apple FS, Pearce LA, Smith SW, Kaczmarek JM, Murakami MM. Role of monitoring changes in sensitive cardiac troponin I assay results for early diagnosis of myocardial infarction and prediction of risk of adverse events. Clin Chem. 2009; 55:930–7.
Article19. NACB Writing Group. Wu AH, Jaffe AS, Apple FS, Jesse RL, Francis GL, et al. National Academy of Clinical Biochemistry laboratory medicine practice guidelines: use of cardiac troponin and B-type natriuretic peptide or N-terminal proB-type natriuretic peptide for etiologies other than acute coronary syndromes and heart failure. Clin Chem. 2007; 53:2086–96.20. Ji M, Moon HW, Hur M, Yun YM. Determination of high-sensitivity cardiac troponin I 99th percentile upper reference limits in a healthy Korean population. Clin Biochem. 2016; 49:756–61.
Article21. Reichlin T, Irfan A, Twerenbold R, Reiter M, Hochholzer W, Burkhalter H, et al. Utility of absolute and relative changes in cardiac troponin concentrations in the early diagnosis of acute myocardial infarction. Circulation. 2011; 124:136–45.
Article22. Fitzgerald G, Kerley RN, Kiernan TJ. High-sensitivity troponin assays: development and utility in a modern health-care system. Expert Rev Cardiovasc Ther. 2019; 17:763–70.
Article23. Irfan A, Reichlin T, Twerenbold R, Meister M, Moehring B, Wildi K, et al. Early diagnosis of myocardial infarction using absolute and relative changes in cardiac troponin concentrations. Am J Med. 2013; 126:781–88.e2.
Article24. Rubini Gimenez M, Twerenbold R, Jaeger C, Schindler C, Puelacher C, Wildi K, et al. One-hour rule-in and rule-out of acute myocardial infarction using high-sensitivity cardiac troponin I. Am J Med. 2015; 128:861–70.e4.
Article25. Yokoyama H, Higuma T, Endo T, Nishizaki F, Hanada K, Yokota T, et al. “30-minute-delta” of high-sensitivity troponin I improves diagnostic performance in acute myocardial infarction. J Cardiol. 2018; 71:144–8.
Article26. Mueller C, Twerenbold R, Reichlin T. Early diagnosis of myocardial infarction with sensitive cardiac troponin assays. Clin Chem. 2019; 65:490–1.
Article27. Reichlin T, Hochholzer W, Bassetti S, Steuer S, Stelzig C, Hartwiger S, et al. Early diagnosis of myocardial infarction with sensitive cardiac troponin assays. N Engl J Med. 2009; 361:858–67.
Article28. Gualandro DM, Twerenbold R, Boeddinghaus J, Nestelberger T, Puelacher C, Müller C. Biomarkers in cardiovascular medicine: towards precision medicine. Swiss Med Wkly. 2019; 149:w20125.
Article29. Wildi K, Nelles B, Twerenbold R, Rubini Giménez M, Reichlin T, Singeisen H, et al. Safety and efficacy of the 0 h/3 h protocol for rapid rule out of myocardial infarction. Am Heart J. 2016; 181:16–25.
Article30. Keller T, Zeller T, Ojeda F, Tzikas S, Lillpopp L, Sinning C, et al. Serial changes in highly sensitive troponin I assay and early diagnosis of myocardial infarction. JAMA. 2011; 306:2684–93.
Article31. Tan JWC, Lam CSP, Kasim SS, Aw TC, Abanilla JM, Chang WT, et al. Asia-pacific consensus statement on the optimal use of high-sensitivity troponin assays in acute coronary syndromes diagnosis: focus on hs-TnI. Heart Asia. 2017; 9:81–7.
Article32. Garg P, Morris P, Fazlanie AL, Vijayan S, Dancsi B, Dstidar AG, et al. Cardiac biomarkers of acute coronary syndrome: from history to high sensitivity cardiac troponin. Intern Emerg Med. 2017; 12:147–55.33. Marino R, Magrini L, Orsini F, Russo V, Cardelli P, Salerno G, et al. Comparison between soluble ST2 and high-sensitivity troponin I in predicting short-term mortality for patients presenting to the emergency department with chest pain. Ann Lab Med. 2017; 37:137–46.
Article34. Muller M, Bierner M, Vafaie M, Doerr S, Keller T, Blankenberg S, et al. Absolute and relative kinetic changes of high-sensitivity cardiac troponin T in acute coronary syndrome and in patients with increased troponin in the absence of acute coronary syndrome. Clin Chem. 2012; 58:209–18.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Diagnostic Value of Cardiac STATus(TM) for Diagnosing Acute Cardiac Ischemia in Patients with Acute Chest Pain in an Emergency Settings
- Is it Necessary to Study both Creatine Kinase MB and Troponin for an Acute Diagnosis of Myocardial Infarction?
- Absolute Change in High Sensitivity Cardiac Troponin I for Three Hours is Useful for Diagnosing Acute Myocardial Infarction in the Emergency Department: How to Get to Best Benefit From HS-Troponins in Clinical Practice?
- Limited Contribution of Creatine Kinase-Myocardial Band Alongside High-Sensitivity Cardiac Troponin in Diagnosing Acute Myocardial Infarction in an Emergency Department
- Efficacy of the Troponin T Rapid Assay Kit in Early Diagnosis of Acute Myocardial Infarction