Clin Endosc.
2020 Sep;53(5):525-534. 10.5946/ce.2020.173.
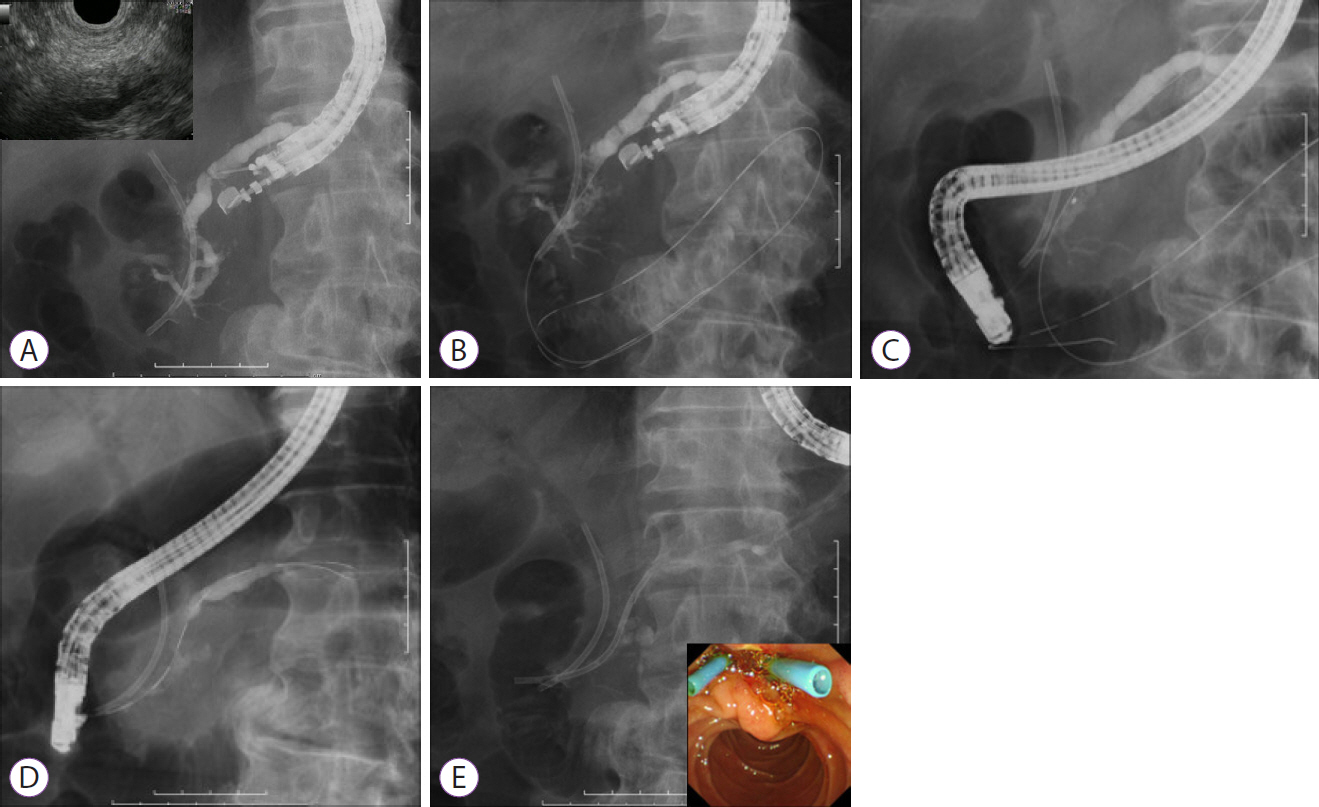
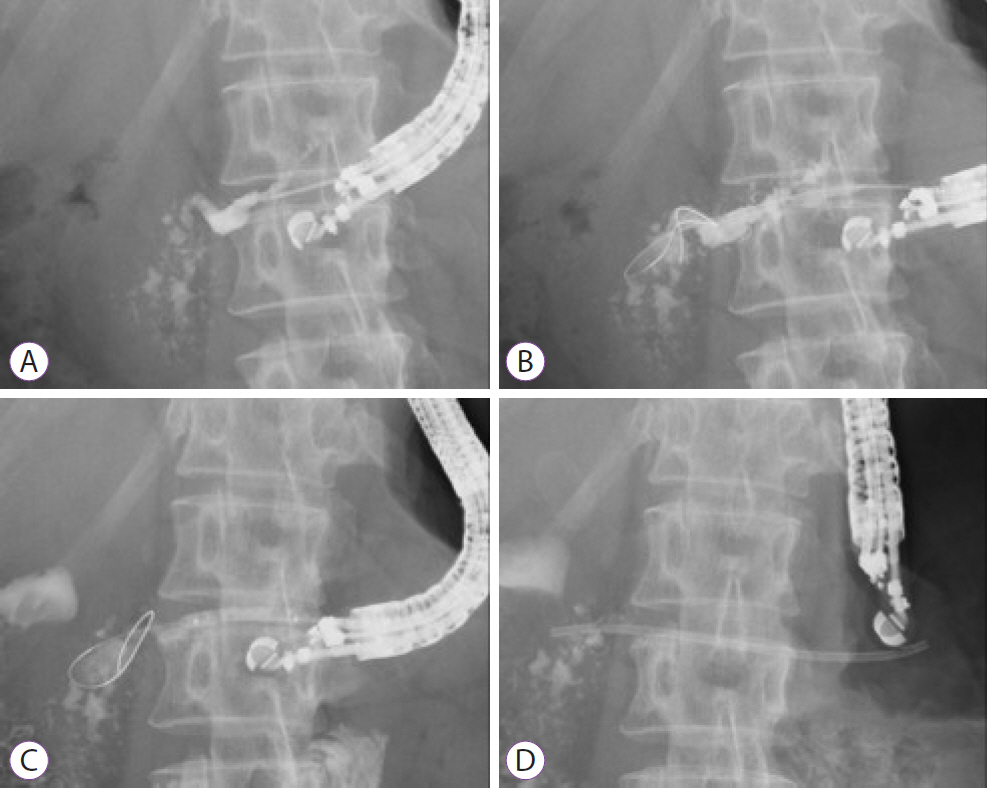
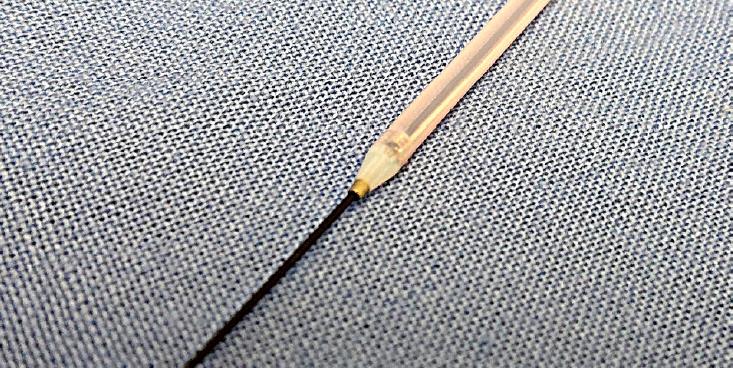
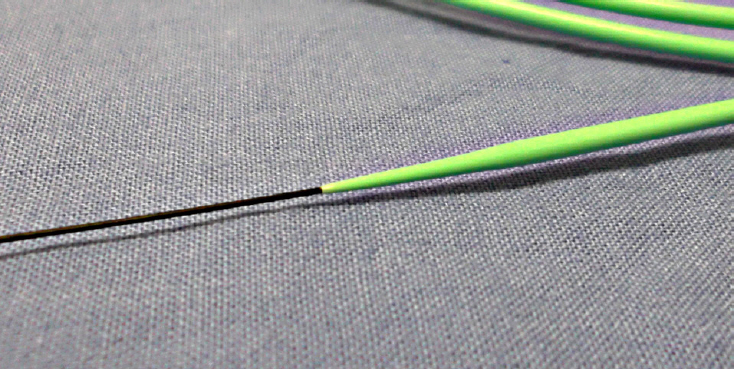
Endoscopic Ultrasound-Guided Pancreatic Duct Drainage: Techniques and Literature Review of Transmural Stenting
- Affiliations
-
- 1Aoyama Hospital, Fujiidera, Osaka, Japan
- 2Second Department of Internal Medicine, Osaka Medical College, Takatsuki, Osaka, Japan
- KMID: 2507585
- DOI: http://doi.org/10.5946/ce.2020.173
Abstract
- Endoscopic ultrasound-guided pancreatic duct drainage (EUS-PD) has emerged as an option in patients with failure of retrograde access to the pancreatic duct (PD) because of difficulty in cannulation or surgically altered anatomy. This article provides a comprehensive review of the techniques and outcomes of EUS-PD, especially EUS-guided pancreatic transmural stenting. The clinical data derived from a total of 401 patients were reviewed in which the overall technical and clinical success rates were 339/401 (85%, range 63%–100%) and 328/372 (88%, range 76%–100%), respectively. Short-term adverse events occurred in 25% (102/401) of the cases, which included abdominal pain (n=45), acute pancreatitis (n=17), bleeding (n=10), and issues associated with pancreatic juice leakage such as perigastric or peripancreatic fluid collection (n=9). In conclusion, although EUS-PD remains a challenging procedure with a high risk of adverse events such as pancreatic juice leakage, perforation, and severe acute pancreatitis, the procedure seems to be a promising alternative for PD drainage in patients with altered anatomy or unsuccessful endoscopic retrograde pancreatography.
Keyword
Figure
Cited by 1 articles
-
Endoscopic Ultrasound-guided Drainage in Pancreatobiliary Diseases
Tae Hyeon Kim, Hyung Ku Chon
Korean J Gastroenterol. 2022;79(5):203-209. doi: 10.4166/kjg.2022.064.
Reference
-
1. Bataille L, Deprez P. A new application for therapeutic EUS: main pancreatic duct drainage with a “pancreatic rendezvous technique”. Gastrointest Endosc. 2002; 55:740–743.
Article2. Oh D, Park DH, Song TJ, et al. Long-term outcome of endoscopic ultrasound-guided pancreatic duct drainage using a fully covered self-expandable metal stent for pancreaticojejunal anastomosis stricture. J Gastroenterol Hepatol. 2020; 35:994–1001.
Article3. Tessier G, Bories E, Arvanitakis M, et al. EUS-guided pancreatogastrostomy and pancreatobulbostomy for the treatment of pain in patients with pancreatic ductal dilatation inaccessible for transpapillary endoscopic therapy. Gastrointest Endosc. 2007; 65:233–241.
Article4. Hayat U, Freeman ML, Trikudanathan G, Azeem N, Amateau SK, Mallery J. Endoscopic ultrasound-guided pancreatic duct intervention and pancreaticogastrostomy using a novel cross-platform technique with small-caliber devices. Endosc Int Open. 2020; 8:E196–E202.
Article5. Uchida D, Kato H, Saragai Y, et al. Indications for endoscopic ultrasound-guided pancreatic drainage: for benign or malignant cases? Can J Gastroenterol Hepatol. 2018; 2018:8216109.
Article6. Matsunami Y, Itoi T, Sofuni A, et al. Evaluation of a new stent for EUS-guided pancreatic duct drainage: long-term follow-up outcome. Endosc Int Open. 2018; 6:E505–E512.
Article7. Will U, Reichel A, Fueldner F, Meyer F. Endoscopic ultrasonography-guided drainage for patients with symptomatic obstruction and enlargement of the pancreatic duct. World J Gastroenterol. 2015; 21:13140–13151.
Article8. Fujii LL, Topazian MD, Abu Dayyeh BK, et al. EUS-guided pancreatic duct intervention: outcomes of a single tertiary-care referral center experience. Gastrointest Endosc. 2013; 78:854–864.e1.
Article9. Itoi T, Kasuya K, Sofuni A, et al. Endoscopic ultrasonography-guided pancreatic duct access: techniques and literature review of pancreatography, transmural drainage and rendezvous techniques. Dig Endosc. 2013; 25:241–252.
Article10. Itoi T, Yasuda I, Kurihara T, Itokawa F, Kasuya K. Technique of endoscopic ultrasonography-guided pancreatic duct intervention (with videos). J Hepatobiliary Pancreat Sci. 2014; 21:E4–E9.
Article11. Chen YI, Levy MJ, Moreels TG, et al. An international multicenter study comparing EUS-guided pancreatic duct drainage with enteroscopy-assisted endoscopic retrograde pancreatography after Whipple surgery. Gastrointest Endosc. 2017; 85:170–177.
Article12. Dhir V, Isayama H, Itoi T, et al. Endoscopic ultrasonography-guided biliary and pancreatic duct interventions. Dig Endosc. 2017; 29:472–485.
Article13. Ogura T, Ohama H, Higuchi K. Endoscopic ultrasound-guided pancreatic transmural stenting and transmural intervention. Clin Endosc. 2020; 53:429–435.
Article14. Ogura T, Nishioka N, Yamada M, Ueshima K, Higuchi K. Endoscopic ultrasound-guided pancreatic duct drainage using a fine-gauge balloon catheter. Endoscopy. 2019; 51:E145–E146.
Article15. Dalal A, Patil G, Maydeo A. Six-year retrospective analysis of endoscopic ultrasonography-guided pancreatic ductal interventions at a tertiary referral center. Dig Endosc. 2020; 32:409–416.
Article16. Mandai K, Uno K, Yasuda K. Endoscopic ultrasound-guided pancreatic duct drainage using a novel fine-gauge electrocautery dilator. Endoscopy. 2019; 51:E388–E389.
Article17. Krafft MR, Nasr JY. Anterograde endoscopic ultrasound-guided pancreatic duct drainage: a technical review. Dig Dis Sci. 2019; 64:1770–1781.
Article18. Honjo M, Itoi T, Tsuchiya T, et al. Safety and efficacy of ultra-tapered mechanical dilator for EUS-guided hepaticogastrostomy and pancreatic duct drainage compared with electrocautery dilator (with video). Endosc Ultrasound. 2018; 7:376–382.
Article19. Kitamura K, Yamamiya A, Ishii Y, Nomoto T, Honma T, Yoshida H. Electrocautery vs non-electrocautery dilation catheters in endoscopic ultrasonography-guided pancreatic fluid collection drainage. World J Gastrointest Endosc. 2016; 8:458–465.20. Kahaleh M, Artifon EL, Perez-Miranda M, et al. Endoscopic ultrasonography guided biliary drainage: summary of consortium meeting, May 7th, 2011, Chicago. World J Gastroenterol. 2013; 19:1372–1379.
Article21. Fujii-Lau LL, Levy MJ. Endoscopic ultrasound-guided pancreatic duct drainage. J Hepatobiliary Pancreat Sci. 2015; 22:51–57.
Article22. Chapman CG, Waxman I, Siddiqui UD. Endoscopic ultrasound (EUS)-guided pancreatic duct drainage: the basics of when and how to perform EUS-guided pancreatic duct interventions. Clin Endosc. 2016; 49:161–167.
Article23. Park DH, Jang JW, Lee SS, Seo DW, Lee SK, Kim MH. EUS-guided biliary drainage with transluminal stenting after failed ERCP: predictors of adverse events and long-term results. Gastrointest Endosc. 2011; 74:1276–1284.
Article24. Khashab MA, Messallam AA, Penas I, et al. International multicenter comparative trial of transluminal EUS-guided biliary drainage via hepatogastrostomy vs. choledochoduodenostomy approaches. Endosc Int Open. 2016; 4:E175–E181.
Article25. Kanno Y, Ito K, Koshita S, et al. Efficacy of a newly developed dilator for endoscopic ultrasound-guided biliary drainage. World J Gastrointest Endosc. 2017; 9:304–309.
Article26. Amano M, Ogura T, Onda S, et al. Prospective clinical study of endoscopic ultrasound-guided biliary drainage using novel balloon catheter (with video). J Gastroenterol Hepatol. 2017; 32:716–720.
Article27. Tyberg A, Sharaiha RZ, Kedia P, et al. EUS-guided pancreatic drainage for pancreatic strictures after failed ERCP: a multicenter international collaborative study. Gastrointest Endosc. 2017; 85:164–169.
Article28. Park DH, Kim MH, Moon SH, Lee SS, Seo DW, Lee SK. Feasibility and safety of placement of a newly designed, fully covered self-expandable metal stent for refractory benign pancreatic ductal strictures: a pilot study (with video). Gastrointest Endosc. 2008; 68:1182–1189.
Article29. Oh D, Park DH, Cho MK, et al. Feasibility and safety of a fully covered self-expandable metal stent with antimigration properties for EUS-guided pancreatic duct drainage: early and midterm outcomes (with video). Gastrointest Endosc. 2016; 83:366–373.e2.
Article30. Bang JY, Varadarajulu S. Lumen-apposing metal stents for endoscopic ultrasonography-guided interventions. Dig Endosc. 2019; 31:619–626.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Technical tips for endoscopic ultrasound-guided pancreatic duct access and drainage
- Endoscopic Ultrasound-Guided Pancreatic Transmural Stenting and Transmural Intervention
- Endoscopic Drainage of Pseudocysts
- Endoscopic Ultrasound-Guided Pancreatobiliary Endoscopy in Surgically Altered Anatomy
- Endoscopic Ultrasound-Guided Drainage of Pancreatic Fluid Collections (with Video)