Korean J Ophthalmol.
2020 Apr;34(2):143-149. 10.3341/kjo.2019.0090.
Motor and Sensory Outcomes of Infantile Exotropia: A 10-Year Study (2008–2017)
- Affiliations
-
- 1Ophthalmic Epidemiology Research Center, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
- 2Department of Ophthalmology, School of Medicine, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
- 3Negah Specialty Ophthalmic Research Center, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
- 4Ophthalmic Research Center, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
- 5Department of Optometry, School of Rehabilitation, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
- 6Basir Eye Safety Research Center, Basir Eye Clinic, Tehran, Iran.
- KMID: 2507404
- DOI: http://doi.org/10.3341/kjo.2019.0090
Abstract
- Purpose
We aimed to determine the long-term motor and sensory outcomes of patients with infantile exotropia.
Methods
In this longitudinal retrospective (historical cohort) study, the records of 76 patients with infantile exotropia were Studied. Subjects with constant exotropia manifesting before the age of 1 year who were at least 5 years old at recruitment time between 2008 and 2017 were included.
Results
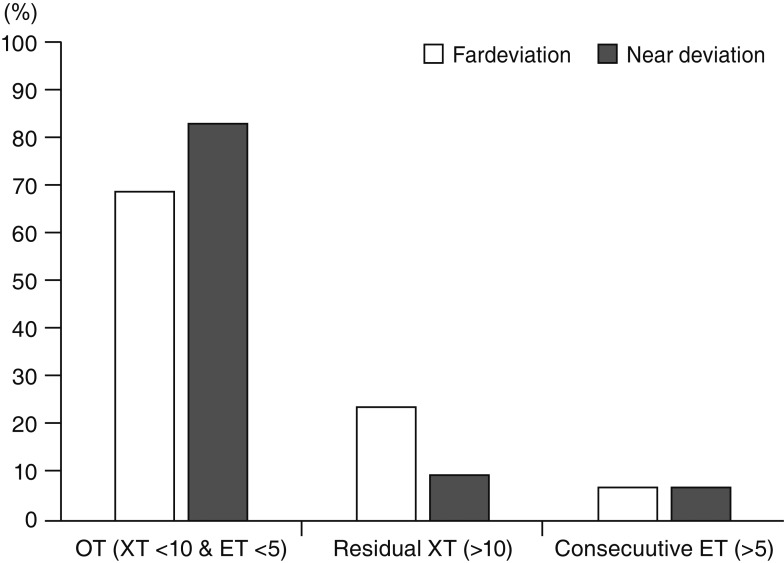
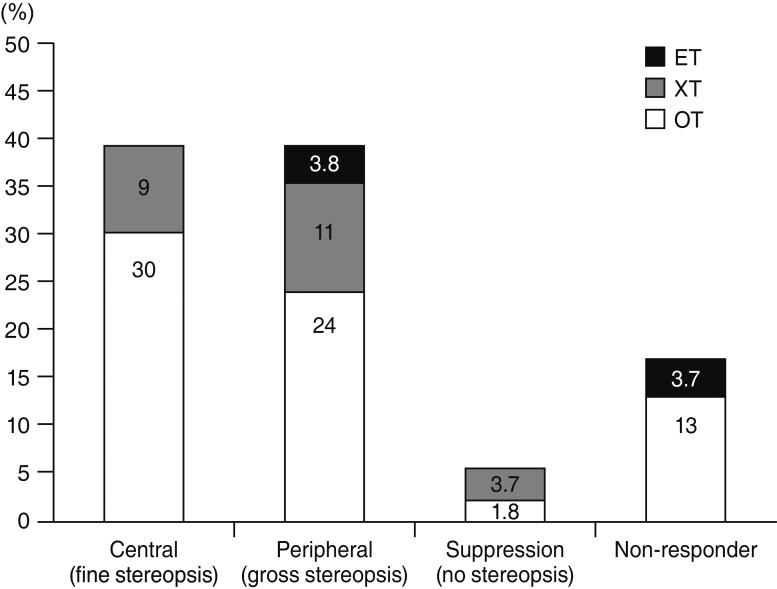
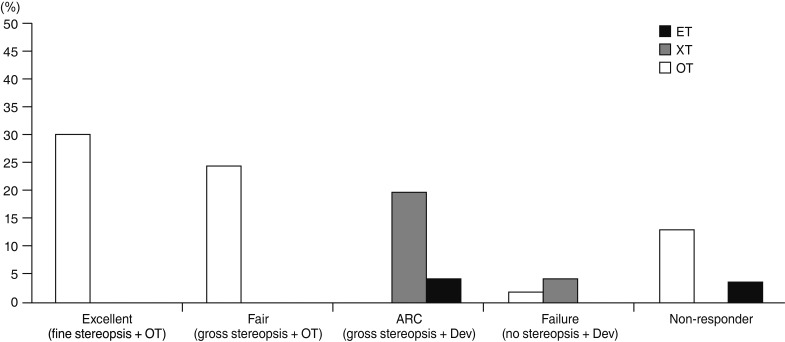
The medical records of 26 patients were excluded due to not participating in follow-up examinations or having incomplete records. In total, 54 infantile exotropic patients (51.9% male) with a mean age of 11.1 ± 6.8 years and follow-up of 4.99 ± 3.58 years were studied. Postoperative sensory outcomes (central stereopsis [<60 sec/arc], peripheral fusion [60–3,000 sec/arc], and non-stereopsis [>3,000 sec/arc]) were observed in 38.9%, 38.9%, and 21.2% of patients, respectively. In terms of postoperative motor outcomes, 69%, 24%, and 7% were achieved as orthophoria, residual exotropia, and consecutive esotropia, respectively. Patients with a higher surgical age (p = 0.022) and better visual acuity (p = 0.004) had significantly better sensory outcomes, while higher preoperative deviation resulted in more suppression (p = 0.039, rs = 0.218).
Conclusions
With rates of 69% for motor success and 78.8% for sensory success, surgical outcomes of infantile exotropic patients seems to be favorable. Further studies are recommended to verify our findings.
Keyword
Figure
Reference
-
1. Yam JC, Wu PK, Chong GS, et al. Long-term ocular alignment after bilateral lateral rectus recession in children with infantile and intermittent exotropia. J AAPOS. 2012; 16:274–279. PMID: 22681946.
Article2. Yoo EJ, Kim SH. Optimal surgical timing in infantile exotropia. Can J Ophthalmol. 2014; 49:358–362. PMID: 25103653.
Article3. Hunter DG, Kelly JB, Buffenn AN, Ellis FJ. Long-term outcome of uncomplicated infantile exotropia. J AAPOS. 2001; 5:352–356. PMID: 11753254.
Article4. Biedner B. Congenital constant exotropia: surgical results in six patients. Binocul Vis. 1993; 8:137–140.5. Na KH, Kim SH. Early versus late surgery for infantile exotropia. J AAPOS. 2018; 22:3–6. PMID: 29158152.
Article6. Rajavi Z, Lashgari A, Sabbaghi H, et al. The incidence of reoperation and related risk factors among patients with infantile exotropia. J Pediatr Ophthalmol Strabismus. 2017; 54:22–30. PMID: 27783093.
Article7. Feng L, Zhou J, Chen L, Hess RF. Sensory eye balance in surgically corrected intermittent exotropes with normal stereopsis. Sci Rep. 2015; 5:13075. PMID: 26287935.
Article8. Hiles DA, Biglan AW. Early surgery of infantile exotropia. Trans Pa Acad Ophthalmol Otolaryngol. 1983; 36:161–168. PMID: 6659036.9. Moore S, Cohen RL. Congenital exotropia. Am Orthopt J. 1985; 35:68–70.
Article10. Choi YM, Kim SH. Comparison of clinical features between two different types of exotropia before 12 months of age based on stereopsis outcome. Ophthalmology. 2013; 120:3–7. PMID: 23031669.
Article11. Schalij-Delfos NE, de Graaf ME, Treffers WF, et al. Long term follow up of premature infants: detection of strabismus, amblyopia, and refractive errors. Br J Ophthalmol. 2000; 84:963–967. PMID: 10966945.
Article12. Rajavi Z, Sabbaghi H, Baghini AS, et al. Prevalence of amblyopia and refractive errors among primary school children. J Ophthalmic Vis Res. 2015; 10:408–416. PMID: 27051485.
Article13. Parks M. Concomitant esodeviations. In : Tasman W, Jaeger E, editors. Duane's clinical ophthalmology. Philadelphila: Lippincott, Williams & Wilkins;2000. p. 12.14. Seo HJ, Kim SH. Long-term postoperative development of stereopsis in infantile exotropia. Asia Pac J Ophthalmol (Phila). 2015; 4:371–375. PMID: 26727191.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Sensory and Motor Functions in Patients with Constant and Intermittent Infantile Exotropia
- Clinical effect of early surgery in infantile exotropia
- Surgical Outcomes of Intermittent Exotropia According to the Constancy
- The Comparison of Long-term Surgical Results for Sensory Exotropia and Comitant Exotropia
- Clinical Course and Outcome of Infantile Exotropia