Infect Chemother.
2020 Mar;52(1):31-38. 10.3947/ic.2020.52.1.31.
Korean Registry for Improving Sepsis Survival (KISS): Protocol for a Multicenter Cohort of Adult Patients with Sepsis or Septic Shock
- Affiliations
-
- 1Division of Infectious Diseases, Department of Internal Medicine, Korea University College of Medicine, Seoul, Korea
- 2Department of Internal Medicine and AIDS research institute, Yonsei University College of Medicine, Seoul, Korea
- 3Division of Infectious Diseases, Department of Internal Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 4Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Korea
- 5Division of Infectious Diseases, Department of Internal Medicine, Hallym University College of Medicine, Seoul, Korea
- 6Division of Infectious Diseases, Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea
- KMID: 2507321
- DOI: http://doi.org/10.3947/ic.2020.52.1.31
Abstract
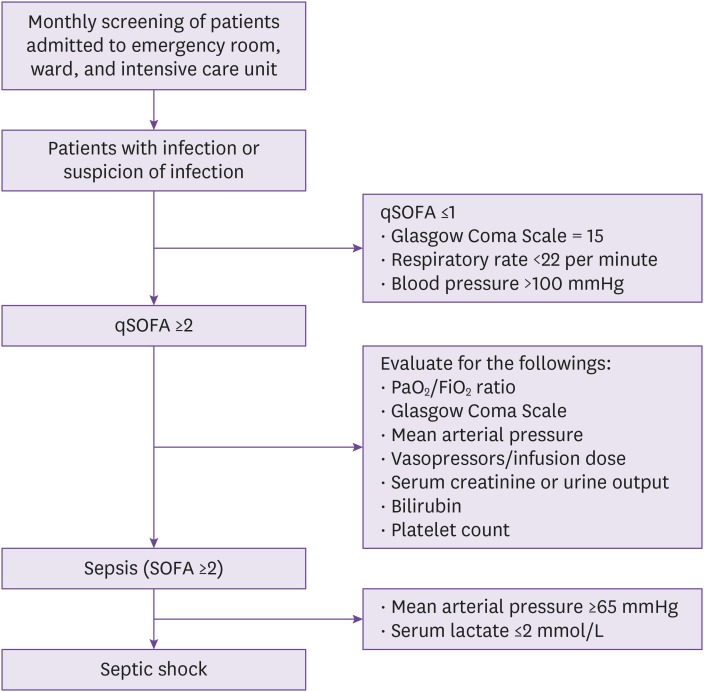
- Sepsis is one of the significant causes of morbidity and mortality. The burden caused by sepsis has continued to increase in recent years in the Korea, highlighting the urgent need for the implementation of strategies to improve sepsis treatment outcomes. We therefore designed a web-based sepsis registry system (“Korean Registry for Improving Sepsis Survival” [KISS]) protocol to be used in hospitals in the Korea for evaluation of the epidemiology and clinical characteristics of patients with sepsis, via an analysis of outcome predictors. The inclusion criteria of this registry are as follows: adult patients ≥18 years admitted to the participating hospitals who are diagnosed with sepsis or septic shock. Demographic and clinical information data of the patients will be collected from hospital medical records and will be recorded in a case report form, which will be entered into a web-based data management system. The analysis of the collected data will be performed as follows: (1) epidemiological and clinical characteristics of sepsis and septic shock, (2) application of sepsis bundles and antibiotic stewardship, and (3) audit and feedback. In conclusion, we aim to build the comprehensive web-based sepsis registry in the Korea through a nation-wide network of participating hospitals. Information collected and analyzed through the KISS can be used for further improvements in the clinical management of sepsis. Furthermore, the KISS will facilitate research leading to the formulation of public health policies regarding sepsis bundle and antibiotic stewardship strategies in the Korea.
Keyword
Figure
Reference
-
1. Fleischmann C, Scherag A, Adhikari NK, Hartog CS, Tsaganos T, Schlattmann P, Angus DC, Reinhart K. International Forum of Acute Care Trialists. Assessment of global incidence and mortality of hospital-treated sepsis. current estimates and limitations. Am J Respir Crit Care Med. 2016; 193:259–272. PMID: 26414292.
Article2. Torio CM, Moore BJ. National inpatient hospital costs: The most expensive conditions by Payer, 2013: Statistical Brief #204. Accessed 8 February 2020. Available at: https://www.hcup-us.ahrq.gov/reports/statbriefs/sb204-Most-Expensive-Hospital-Conditions.jsp?utm_source=AHRQ&utm_medium=AHRQSTAT&utm_content=Content&utm_term=HCUP&utm_campaign=AHRQ_SB_204_2016.3. Angus DC, Linde-Zwirble WT, Lidicker J, Clermont G, Carcillo J, Pinsky MR. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med. 2001; 29:1303–1310. PMID: 11445675.
Article4. Park M, Kim K, Lee JH, Kang C, Jo YH, Kim DH, Kang KW, Lee SH, Park C, Kim J, Chung H, Park H, Jang S. Awareness and knowledge of sepsis in the general Korean population: comparison with the awareness and knowledge of acute myocardial infarction and stroke. Clin Exp Emerg Med. 2014; 1:41–48. PMID: 27752551.
Article5. Park DW, Chun BC, Kim JM, Sohn JW, Peck KR, Kim YS, Choi YH, Choi JY, Kim SI, Eom JS, Kim HY, Song JY, Song YG, Choi HJ, Kim MJ. Epidemiological and clinical characteristics of community-acquired severe sepsis and septic shock: a prospective observational study in 12 university hospitals in Korea. J Korean Med Sci. 2012; 27:1308–1314. PMID: 23166410.
Article6. Korean Statistical Information Service. Accessed 8 February 2020. Available at: http://kosis.kr/statHtml/statHtml.do?orgId=101&tblId=DT_1B34E01&vw_cd=MT_ZTITLE&list_id=D11&seqNo=&lang_mode=ko&language=kor&obj_var_id=&itm_id=&conn_path=MT_ZTITLE.7. Rhodes A, Evans LE, Alhazzani W, Levy MM, Antonelli M, Ferrer R, Kumar A, Sevransky JE, Sprung CL, Nunnally ME, Rochwerg B, Rubenfeld GD, Angus DC, Annane D, Beale RJ, Bellinghan GJ, Bernard GR, Chiche JD, Coopersmith C, De Backer DP, French CJ, Fujishima S, Gerlach H, Hidalgo JL, Hollenberg SM, Jones AE, Karnad DR, Kleinpell RM, Koh Y, Lisboa TC, Machado FR, Marini JJ, Marshall JC, Mazuski JE, McIntyre LA, McLean AS, Mehta S, Moreno RP, Myburgh J, Navalesi P, Nishida O, Osborn TM, Perner A, Plunkett CM, Ranieri M, Schorr CA, Seckel MA, Seymour CW, Shieh L, Shukri KA, Simpson SQ, Singer M, Thompson BT, Townsend SR, Van der Poll T, Vincent JL, Wiersinga WJ, Zimmerman JL, Dellinger RP. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock: 2016. Intensive Care Med. 2017; 43:304–377. PMID: 28101605.
Article8. Seymour CW, Gesten F, Prescott HC, Friedrich ME, Iwashyna TJ, Phillips GS, Lemeshow S, Osborn T, Terry KM, Levy MM. Time to treatment and mortality during mandated emergency care for sepsis. N Engl J Med. 2017; 376:2235–2244. PMID: 28528569.
Article9. Levy MM, Rhodes A, Phillips GS, Townsend SR, Schorr CA, Beale R, Osborn T, Lemeshow S, Chiche JD, Artigas A, Dellinger RP. Surviving sepsis campaign: association between performance metrics and outcomes in a 7.5-year study. Intensive Care Med. 2014; 40:1623–1633. PMID: 25270221.
Article10. Levy MM, Dellinger RP, Townsend SR, Linde-Zwirble WT, Marshall JC, Bion J, Schorr C, Artigas A, Ramsay G, Beale R, Parker MM, Gerlach H, Reinhart K, Silva E, Harvey M, Regan S, Angus DC. Surviving Sepsis Campaign. The surviving sepsis campaign: results of an international guideline-based performance improvement program targeting severe sepsis. Crit Care Med. 2010; 38:367–374. PMID: 20035219.
Article11. New York State. Department of health: Sepsis. Accessed 8 February 2020. Available at: https://www.health.ny.gov/diseases/conditions/sepsis/.12. Levy MM, Gesten FC, Phillips GS, Terry KM, Seymour CW, Prescott HC, Friedrich M, Iwashyna TJ, Osborn T, Lemeshow S. Mortality changes associated with mandated public reporting for sepsis. The results of the New York State initiative. Am J Respir Crit Care Med. 2018; 198:1406–1412. PMID: 30189749.
Article13. Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, Bellomo R, Bernard GR, Chiche JD, Coopersmith CM, Hotchkiss RS, Levy MM, Marshall JC, Martin GS, Opal SM, Rubenfeld GD, van der Poll T, Vincent JL, Angus DC. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016; 315:801–810. PMID: 26903338.
Article14. Shin TG, Hwang SY, Kang GH, Kim WY, Ryoo SM, Kim K, Jo YH, Chung SP, Joo YS, Beom JH, Choi SH, Yoon YH, Kwon WY, Lim TH, Han KS, Choi HS, Suh GJ. Korean Shock Society septic shock registry: a preliminary report. Clin Exp Emerg Med. 2017; 4:146–153. PMID: 29026888.
Article15. Venkatesh AK, Slesinger T, Whittle J, Osborn T, Aaronson E, Rothenberg C, Tarrant N, Goyal P, Yealy DM, Schuur JD. Preliminary performance on the new CMS sepsis-1 national quality measure: early insights from the emergency quality network (E-QUAL). Ann Emerg Med. 2018; 71:10–15.e1. PMID: 28789803.
Article16. Liu VX, Morehouse JW, Marelich GP, Soule J, Russell T, Skeath M, Adams C, Escobar GJ, Whippy A. Multicenter implementation of a treatment bundle for patients with sepsis and intermediate lactate values. Am J Respir Crit Care Med. 2016; 193:1264–1270. PMID: 26695114.
Article17. Scheer CS, Fuchs C, Kuhn SO, Vollmer M, Rehberg S, Friesecke S, Abel P, Balau V, Bandt C, Meissner K, Hahnenkamp K, Gründling M. Quality improvement initiative for severe sepsis and septic shock reduces 90-day mortality: a 7.5-year observational study. Crit Care Med. 2017; 45:241–252. PMID: 27661863.18. Fitzpatrick F, Tarrant C, Hamilton V, Kiernan FM, Jenkins D, Krockow EM. Sepsis and antimicrobial stewardship: two sides of the same coin. BMJ Qual Saf. 2019; 28:758–761.
Article19. Health Service Executive (HSE). National sepsis report, 2017. Accessed 8 February 2020. Available at: https://www.hse.ie/eng/services/publications/clinical-strategy-and-programmes/sepsis-annual-report-2017.pdf.20. NHS England. Technical guidance for refreshing NHS plans 2018/19 annex A: commissioning for quality and innovation (CQUIN) indicator specification 2017-2019. Accessed 8 February 2020. Available at: https://www.england.nhs.uk/publication/cquin-indicator-specification/.21. Burston J, Adhikari S, Hayen A, Doolan H, Kelly ML, Fu K, Jensen TO, Konecny P. A role for antimicrobial stewardship in clinical sepsis pathways: a prospective interventional study. Infect Control Hosp Epidemiol. 2017; 38:1032–1038. PMID: 28693625.
Article22. Australian and New Zealand Intensive Care Society (ANZICS). Center for outcome and resource evaluation. Accessed 8 February 2020. Available at: http:// www.anzics.com.au/Pages/CORE/About-CORE.aspx.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Sepsis, Severe Sepsis and Septic Shock in the Elderly
- Treatment Guidelines of Sepsis and Septic Shock
- Mortality among adult patients with sepsis and septic shock in Korea: a systematic review and meta-analysis
- Current Insights into Sepsis Treatments
- The predictive value of procalcitonin for septic shock in sepsis patients