Yeungnam Univ J Med.
2020 Jul;37(3):186-193. 10.12701/yujm.2019.00465.
Improvement of catheter-related outcomes after application of tunneled cuffed hemodialysis catheter insertion without fluoroscopy
- Affiliations
-
- 1Division of Nephrology, Department of Internal Medicine, Yeungnam University College of Medicine, Daegu, Korea
- KMID: 2506517
- DOI: http://doi.org/10.12701/yujm.2019.00465
Abstract
- Background
Non-tunneled catheters (NTCs) are used for hemodialysis (HD) in many centers in which fluoroscopy is not easily accessed despite high complication rates and conditions requiring long-term HD. Therefore, here we aimed to evaluate the superiority of catheter-related outcomes after the application of tunneled cuffed catheter (TCC) without fluoroscopy versus unconditioned NTC insertion.
Methods
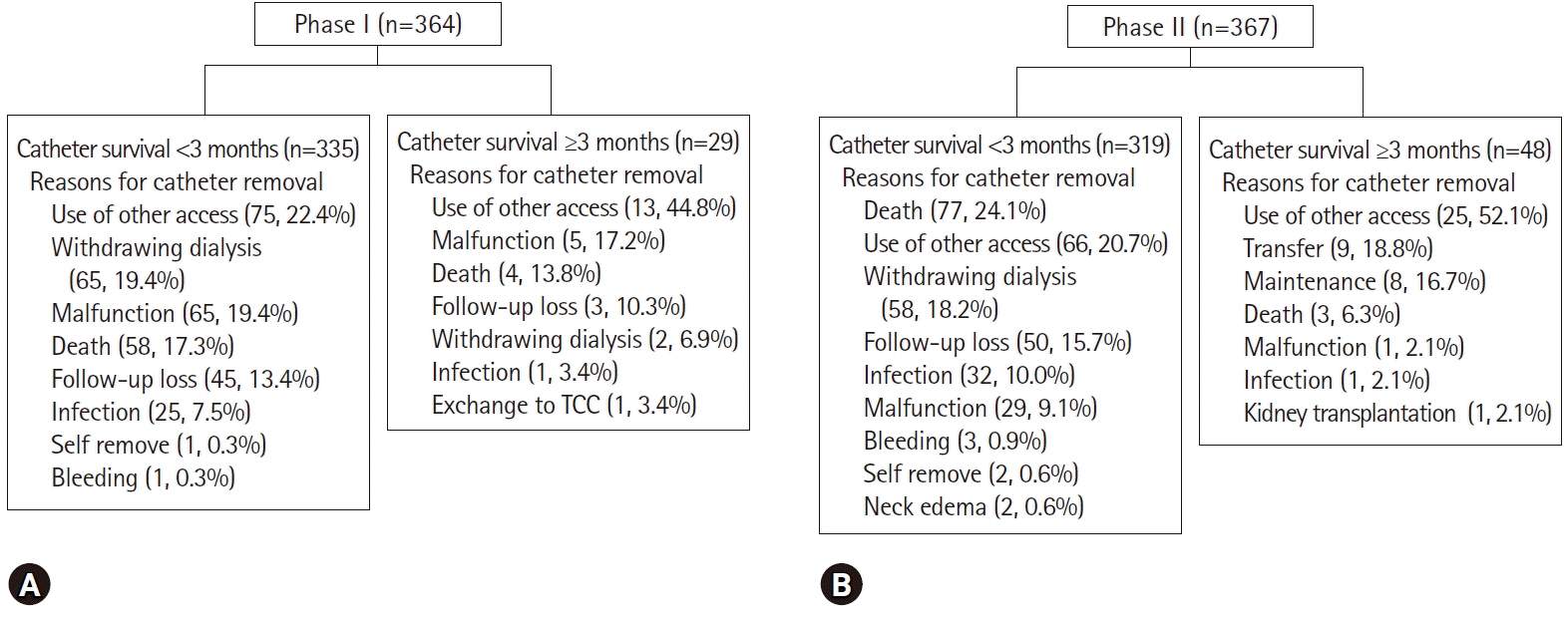
We divided the participants into two phases: those receiving NTCs between March 2010 and February 2011 (phase I), and those receiving TCCs or NTCs between March 2011 and February 2012 (phase II). Catheter survival, nurse satisfaction, and reasons for catheter removal were analyzed.
Results
Two hundred and sixty patients in phase I and 300 patients in phase II were enrolled in this study. The success rate of TCC insertion was 99.2%. The catheter survival rate in phase I was 65.5% at 1 month, while that in phase II was 74.9% at 1 month (p=0.023). We compared catheter survival between TCCs and NTCs for all periods regardless of phase. The TCC survival rate was higher than the NTC survival rate (p<0.001). Catheter-associated problems led to catheter removal in 97 patients (26.6%) in phase I and 68 patients (18.5%) in phase II (p=0.009). Among 14 HD nurses, all reported being satisfied with manipulation during pre-/post-HD, manupulation during HD, and overall. Eleven HD nurses (78.6%) reported being satisfied with the workload.
Conclusion
Compared with unconditional NTC insertion for HD, TCC insertion without fluoroscopy improved the overall catheter survival and nurse satisfaction rates.
Figure
Reference
-
References
1. US Renal Data System. USRDS 2011 annual data report: atlas of chronic kidney disease and end-stage renal disease in the United States [Internet]. Bethesda (MD): National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases;2011. [cited 2019 May 30]. http://www.usrds.org/adr.aspx.2. McDonald S, Excell L, Livingstone B. ANZDATA: Australia and New Zealand dialysis and transplant registry [Internet]. Adelaide (AU): ANZDATA Registry;[cited 2019 May 30]. http://www.anzdata.org.au/anzdata/.3. Jin DC. Current status of dialysis therapy in Korea. Korean J Intern Med. 2011; 26:123–31.
Article4. Yoon HE, Chung S, Chung HW, Shin MJ, Lee SJ, Kim YS, et al. Status of initiating pattern of hemodialysis: a multi-center study. J Korean Med Sci. 2009; 24(Suppl 2):S102–8.
Article5. Vats HS. Complications of catheters: tunneled and nontunneled. Adv Chronic Kidney Dis. 2012; 19:188–94.
Article6. Ponikvar R. Hemodialysis catheters. Ther Apher Dial. 2005; 9:218–22.
Article7. Vascular Access Work Group. Clinical practice guidelines for vascular access. Am J Kidney Dis. 2006; 48(Suppl 1):S248–73.8. Hwang HS, Kang SH, Choi SR, Sun IO, Park HS, Kim Y. Comparison of the palindrome vs. step-tip tunneled hemodialysis catheter: a prospective randomized trial. Semin Dial. 2012; 25:587–91.
Article9. Kang SH, Park WK, Do JY, Cho KH, Park JW, Yoon KW. J-tip guide wire entrapment within the heart during central venous catheterization. Hemodial Int. 2012; 16:438–40.
Article10. Oliver MJ. Acute dialysis catheters. Semin Dial. 2001; 14:432–5.
Article11. Wang K, Wang P, Liang X, Lu X, Liu Z. Epidemiology of haemodialysis catheter complications: a survey of 865 dialysis patients from 14 haemodialysis centres in Henan province in China. BMJ Open. 2015; 5:e007136.
Article12. Mendu ML, May MF, Kaze AD, Graham DA, Cui S, Chen ME, et al. Non-tunneled versus tunneled dialysis catheters for acute kidney injury requiring renal replacement therapy: a prospective cohort study. BMC Nephrol. 2017; 18:351.
Article13. Yevzlin AS, Song GU, Sanchez RJ, Becker YT. Fluoroscopically guided vs modified traditional placement of tunneled hemodialysis catheters: clinical outcomes and cost analysis. J Vasc Access. 2007; 8:245–51.
Article14. Yeum CH, Kim SW, Nah MY, Ma SK, Ko JH, Kim NH, et al. Percutaneous catheterization of the internal jugular vein for hemodialysis. Korean J Intern Med. 2001; 16:242–6.
Article15. Beathard GA, Litchfield T; Physician Operators Forum of RMS Lifeline Inc. Effectiveness and safety of dialysis vascular access procedures performed by interventional nephrologists. Kidney Int. 2004; 66:1622–32.
Article16. Motta Elias R, da Silva Makida SC, Abensur H, Martins Castro MC, Affonso Moyses RM, Pereira BJ, et al. Insertion of tunneled hemodialysis catheters without fluoroscopy. J Vasc Access. 2010; 11:138–42.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Safety and durable patency of tunneled hemodialysis catheter inserted without fluoroscopy
- Complete atrioventricular block during tunneled cuffed hemodialysis catheter insertion in a patient with pre-existing left bundle branch block
- Giant Right Atrial Thrombus associated with Tunneled Cuffed Hemodialysis Catheter: A Case of Successful Treatment with Thrombolytic Agent and Anticoagulant
- Association between initial vascular access and survival in hemodialysis according to age
- Placement of Tunneled Cuffed Hemodialysis Catheters Via Internal Jugular Vein by an Interventional Radiologist and a Vascular Surgeon Together