J Korean Neurosurg Soc.
2020 Sep;63(5):623-630. 10.3340/jkns.2020.0096.
Is the Agricultural Work a Risk Factor for Koreans Elderly Spinal Sagittal Imbalance?
- Affiliations
-
- 1Department of Neurosurgery, Chonnam National University Medical School & Research Institute of Medical Sciences, Gwangju, Korea
- KMID: 2506026
- DOI: http://doi.org/10.3340/jkns.2020.0096
Abstract
Objective
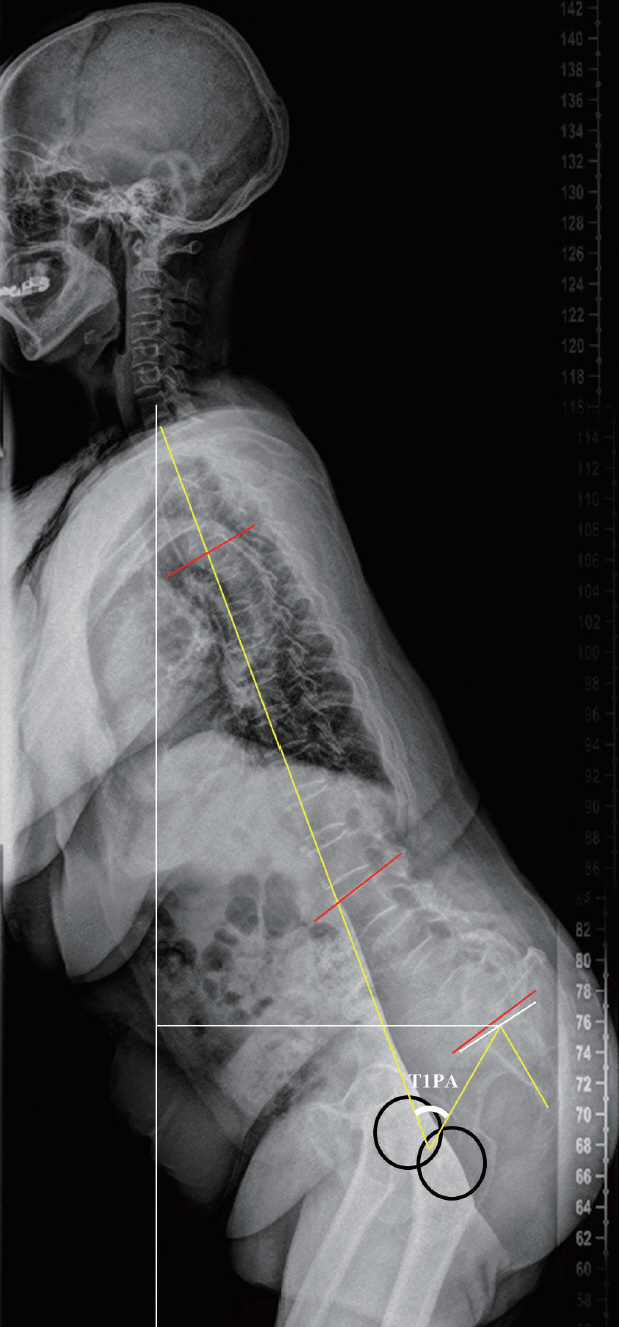
: A primary degenerative sagittal imbalance has been considered because of unique lifestyles such as the prolonged crouched posture during agricultural work and performing activities of daily living on the floor. Previous papers have reported that sagittal imbalance disease is often seen distinctly in the farming districts of “oriental” countries such as Korea and Japan. However, this finding was only evaluated with the use of X-ray, and other factors such as magnetic resonance imaging (MRI), muscle volume, compression fracture, and laboratory results were not considered. Thus, using these, we evaluate the agricultural work-associated factors for Korean elderly spinal sagittal imbalance.
Methods
: We recruited 103 Korean participants who had a sagittal vertical axis (SVA) of >5 cm in this Korean Elderly Sagittal Imbalance Cohort Study. The following were evaluated : radiological parameters, MRI, compression fracture, vitamin D, parathyroid hormone, C-telopeptide, osteocalcin, bone mineral density and muscle fatty change, muscle volume, and health-related quality of life from patients’ survey. Moreover, in this survey, the farmers’ annual working hours were investigated. Subsequently, we analyzed the associated factors for spinal sagittal imbalance depending on occupation.
Results
: A total of 46 participants were farmers, and the others were housewives, sellers, and office workers. The farmer group had more SVA (141 vs. 99 mm, p=0.001) and pelvic tilt (31° vs. 24°, p=0.004) and lesser lumbar lordosis (20° vs. 30°, p=0.009) and thoracic kyphosis (24° vs. 33°, p=0.03) than non-farmer group. A significantly positive correlation was noted between the working hour and SVA in the farmer group (p=0.014). The visual analogue scale score for back pain (8.26 vs. 6.96, p=0.008) and Oswestry Disability Index (23.5 vs. 19.1, p=0.003) in the farmer group were higher than that in the non-farmer group, but the Short Form-36 score was not significantly different between the two groups. The Mini-Mental State Exam score was significantly lower in the farmer group than in the non-farmer group (24.85 vs. 26.98, p=0.002).
Conclusion
: The farmer group had more sagittal imbalance and back pain in proportion to the working hours even though the muscle and bone factors and general laboratory condition were not significantly different between the two groups. These results supported that the long hours spent in the crouched posture while performing agricultural work were a risk factor for severe sagittal imbalance.
Keyword
Figure
Cited by 1 articles
-
The Relationship Between Low Back Pain and Sagittal Spinal Alignment and Back Muscle Mass in Korean Fishery Workers
Minjung Kook, Insuh Kim, Jeongyeon Seo, Hyundong Kim, Heesung Nam, Nami Han
Ann Rehabil Med. 2023;47(6):459-467. doi: 10.5535/arm.23075.
Reference
-
References
1. Ailon T, Smith JS, Shaffrey CI, Lenke LG, Brodke D, Harrop JS, et al. Degenerative spinal deformity. Neurosurgery 77 Suppl. 4:S75–S91. 2015.
Article2. Ames CP, Scheer JK, Lafage V, Smith JS, Bess S, Berven SH, et al. Adult spinal deformity: epidemiology, health impact, evaluation, and management. Spine Deform. 4:310–322. 2016.
Article3. Battaglia PJ, Maeda Y, Welk A, Hough B, Kettner N. Reliability of the Goutallier classification in quantifying muscle fatty degeneration in the lumbar multifidus using magnetic resonance imaging. J Manipulative Physiol Ther. 37:190–197. 2014.
Article4. Bess S, Line B, Fu KM, McCarthy I, Lafage V, Schwab F, et al. The health impact of symptomatic adult spinal deformity: comparison of deformity types to United States population norms and chronic diseases. Spine (Phila Pa 1976). 41:224–233. 2016.5. Cho NH, Jung YO, Lim SH, Chung CK, Kim HA. The prevalence and risk factors of low back pain in rural community residents of Korea. Spine (Phila Pa 1976). 37:2001–2010. 2012.
Article6. Claus A, Hides J, Moseley GL, Hodges P. Sitting versus standing: does the intradiscal pressure cause disc degeneration or low back pain? J Electromyogr Kinesiol. 18:550–558. 2008.
Article7. Department of Economic and Social Affairs United Nations : World population ageing, 1950-2050. New York: United Nations;2002.8. Glassman SD, Berven S, Bridwell K, Horton W, Dimar JR. Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine (Phila Pa 1976). 30:682–688. 2005.
Article9. Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC. Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res. (304):78–83. 1994.10. Kado DM, Prenovost K, Crandall C. Narrative review: hyperkyphosis in older persons. Ann Intern Med. 147:330–338. 2007.
Article11. Kim KT, Lee SH, Suk KS, Lee JH, Im YS, Seo EM. Loss of sagittal balance and clinical outcomes following corrective osteotomy for lumbar degenerative kyphosis. J Korean Orthop Assoc. 44:83–92. 2009.
Article12. Kim MJ, Ahn KY, Jeon YJ. Association of type of physical activity and sedentary time with lower back pain in Korean above 50 years : Korean National Health and Nutrition Examination Survey VI 2014. Korean Soc Sports Sci. 25:1107–1120. 2016.13. Le Huec JC, Faundez A, Dominguez D, Hoffmeyer P, Aunoble S. Evidence showing the relationship between sagittal balance and clinical outcomes in surgical treatment of degenerative spinal diseases: a literature review. Int Orthop. 39:87–95. 2015.
Article14. Lee CH, Chung CK, Jang JS, Kim SM, Chin DK, Lee JK. 'Lumbar degenerative kyphosis' is not byword for degenerative sagittal imbalance: time to replace a misconception. J Korean Neurosurg Soc. 60:125–129. 2017.
Article15. Lee CH, Chung CK, Kim CH, Kwon JW. Health care burden of spinal diseases in the Republic of Korea: analysis of a nationwide database from 2012 through 2016. Neurospine. 15:66–76. 2018.
Article16. Lee CS, Kim YT, Kim E. Clinical study of lumbar degenerative kyphosis. J Korean Soc Spine Surg. 4:27–35. 1997.17. Lee SH, Kim KT, Suk KS, Lee JH, Seo EM, Huh DS. Sagittal decompensation after corrective osteotomy for lumbar degenerative kyphosis: classification and risk factors. Spine (Phila Pa 1976). 36:E538–E544. 2011.18. Mueller G, Morlock MM, Vollmer M, Honl M, Hille E, Schneider E. Intramuscular pressure in the erector spinae and intra-abdominal pressure related to posture and load. Spine (Phila Pa 1976). 23:2580–2590. 1998.
Article19. Protopsaltis T, Schwab F, Bronsard N, Smith JS, Klineberg E, Mundis G, et al. TheT1 pelvic angle, a novel radiographic measure of global sagittal deformity, accounts for both spinal inclination and pelvic tilt and correlates with health-related quality of life. J Bone Joint Surg Am. 96:1631–1640. 2014.
Article20. Roussouly P, Gollogly S, Berthonnaud E, Dimnet J. Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine (Phila Pa 1976). 30:346–353. 2005.
Article21. Roussouly P, Pinheiro-Franco JL. Biomechanical analysis of the spinopelvic organization and adaptation in pathology. Eur Spine J 20 Suppl. 5(Suppl 5):609–618. 2011.
Article22. Ryu DS, Shinn JK, Kim BW, Moon BJ, Ha Y, Lee JK, et al. Prospective observational cohort study of health-related quality of life: marked adult sagittal deformity (ASD) in comparison with mild to moderate ASD. Spine (Phila Pa 1976). 44:1723–1730. 2019.
Article23. Takemitsu Y, Harada Y, Iwahara T, Miyamoto M, Miyatake Y. Lumbar degenerative kyphosis. Clinical, radiological and epidemiological studies. Spine (Phila Pa 1976). 13:1317–1326. 1988.24. Taneichi H. Update on pathology and surgical treatment for adult spinal deformity. J Orthop Sci. 21:116–123. 2016.
Article25. Terran J, Schwab F, Shaffrey CI, Smith JS, Devos P, Ames CP, et al. The SRS-Schwab adult spinal deformity classification: assessment and clinical correlations based on a prospective operative and nonoperative cohort. Neurosurgery. 73:559–568. 2013.26. Yip YB, Ho SC, Chan SG. Identifying risk factors for low back pain (LBP) in Chinese middle-aged women: a case-control study. Health Care Women Int. 25:358–369. 2004.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Sagittal Imbalance
- Proximal Junctional Problems in Surgical Treatment of Lumbar Degenerative Sagittal Imbalance Patients and Relevant Risk Factors
- Optimal Standing Radiographic Positioning in Patients with Sagittal Imbalance
- Spinal Sagittal Imbalance is Associated with Vertebral Fracture without a Definite History of Falls: Cross-Sectional, Comparative Study of Cohort with and without a Distal Radius Fracture
- Proximal Junctional Failure after Corrective Surgery: Focusing on Elderly Patients with Severe Sagittal Imbalance