Arch Hand Microsurg.
2020 Sep;25(3):207-218. 10.12790/ahm.20.0037.
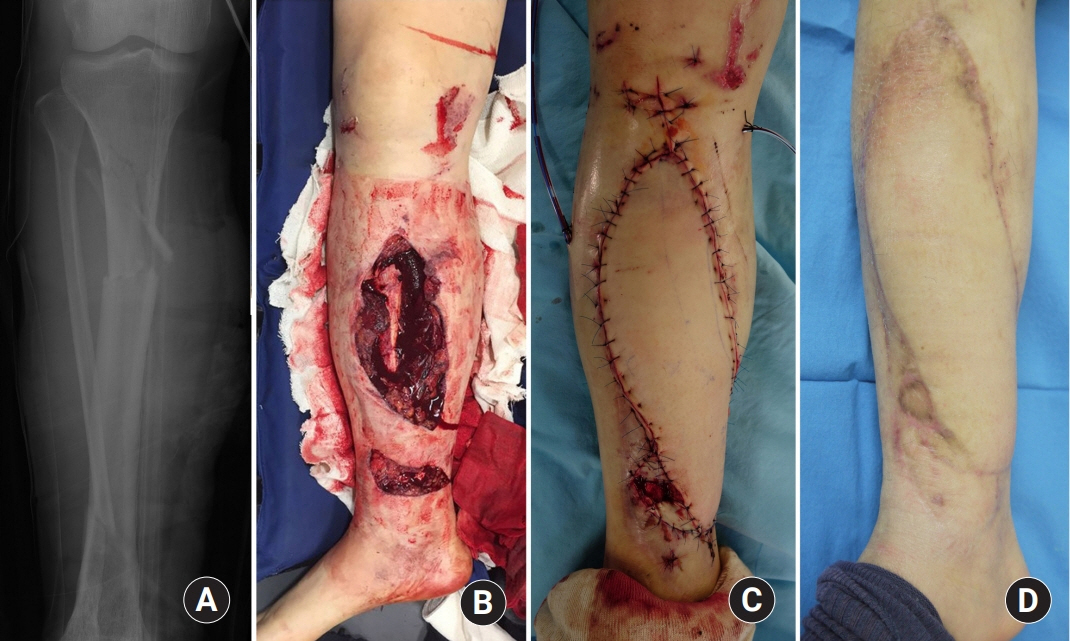
Soft Tissue Reconstruction for Open Tibia Fractures
- Affiliations
-
- 1Department of Orthopedic Surgery, College of Medicine, The Catholic University of Korea, Seoul, Korea
- KMID: 2505902
- DOI: http://doi.org/10.12790/ahm.20.0037
Abstract
- Tibia fractures are the most common long bone fracture and about 24% of them are open fractures. Open fractures accompany disruption of the soft tissue around the fracture site and the fractures are exposed to the external environment. Contamination of the fracture site and devitalization of the injured soft tissue greatly increase the risk of infection, nonunion, and other complications. The first and most important treatment goal of open fractures is prevention of infection. To accomplish this objective, immediate radical debridement and irrigation, second-look operation, and subsequent soft tissue reconstruction should be performed as soon as possible. However, early soft tissue reconstruction is not always possible and when it should be delayed, negative pressure wound therapy is recommended. Among various reconstructive armamentarium including skin graft, local flaps, pedicled flaps, and free flaps, the best method need to be chosen based on patient’s general condition, size of defect, neurovascular status, range of injury zone, and cosmetic and functional perspectives. Preoperative in-depth evaluation of vascular structures is mandatory and free flaps are preferred when the range of injury zone is wide.
Keyword
Figure
Cited by 1 articles
-
Outcomes after Arterial Reconstruction with Autogenous Vein Graft for Limb Salvage in Traumatized Extremity
Mooheon Jeon, Young Keun Lee
Arch Hand Microsurg. 2021;26(3):184-192. doi: 10.12790/ahm.21.0092.
Reference
-
1. Court-Brown CM, McBirnie J. The epidemiology of tibial fractures. J Bone Joint Surg Br. 1995; 77:417–21.
Article2. Gustilo RB, Anderson JT. Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: retrospective and prospective analyses. J Bone Joint Surg Am. 1976; 58:453–8.3. Gustilo RB, Mendoza RM, Williams DN. Problems in the management of type III (severe) open fractures: a new classification of type III open fractures. J Trauma. 1984; 24:742–6.4. Brumback RJ, Jones AL. Interobserver agreement in the classification of open fractures of the tibia. The results of a survey of two hundred and forty-five orthopaedic surgeons. J Bone Joint Surg Am. 1994; 76:1162–6.
Article5. Melvin JS, Dombroski DG, Torbert JT, Kovach SJ, Esterhai JL, Mehta S. Open tibial shaft fractures: I. Evaluation and initial wound management. J Am Acad Orthop Surg. 2010; 18:10–9.
Article6. Patzakis MJ, Wilkins J. Factors influencing infection rate in open fracture wounds. Clin Orthop Relat Res. 1989; (243):36–40.
Article7. Lange RH, Bach AW, Hansen ST Jr, Johansen KH. Open tibial fractures with associated vascular injuries: prognosis for limb salvage. J Trauma. 1985; 25:203–8.8. Caudle RJ, Stern PJ. Severe open fractures of the tibia. J Bone Joint Surg Am. 1987; 69:801–7.
Article9. Soni A, Tzafetta K, Knight S, Giannoudis PV. Gustilo IIIC fractures in the lower limb: our 15-year experience. J Bone Joint Surg Br. 2012; 94:698–703.10. Waikakul S, Sakkarnkosol S, Vanadurongwan V. Vascular injuries in compound fractures of the leg with initially adequate circulation. J Bone Joint Surg Br. 1998; 80:254–8.
Article11. Duymaz A, Karabekmez FE, Vrtiska TJ, Mardini S, Moran SL. Free tissue transfer for lower extremity reconstruction: a study of the role of computed angiography in the planning of free tissue transfer in the posttraumatic setting. Plast Reconstr Surg. 2009; 124:523–9.
Article12. Haddock NT, Weichman KE, Reformat DD, Kligman BE, Levine JP, Saadeh PB. Lower extremity arterial injury patterns and reconstructive outcomes in patients with severe lower extremity trauma: a 26-year review. J Am Coll Surg. 2010; 210:66–72.
Article13. O’Malley O, Trompeter AJ, Krishnanandan S, et al. How common are vascular injuries in open tibial fractures?: a prospective longitudinal cohort study. Eur J Orthop Surg Traumatol. 2019; 29:1119–24.
Article14. Chummun S, Wigglesworth TA, Young K, et al. Does vascular injury affect the outcome of open tibial fractures? Plast Reconstr Surg. 2013; 131:303–9.
Article15. Stranix JT, Lee ZH, Jacoby A, et al. Not all Gustilo type IIIB fractures are created equal: arterial injury impacts limb salvage outcomes. Plast Reconstr Surg. 2017; 140:1033–41.16. Crowley DJ, Kanakaris NK, Giannoudis PV. Debridement and wound closure of open fractures: the impact of the time factor on infection rates. Injury. 2007; 38:879–89.
Article17. Zalavras CG. Prevention of infection in open fractures. Infect Dis Clin North Am. 2017; 31:339–52.
Article18. Pollak AN, Jones AL, Castillo RC, Bosse MJ, MacKenzie EJ; LEAP Study Group. The relationship between time to surgical debridement and incidence of infection after open high-energy lower extremity trauma. J Bone Joint Surg Am. 2010; 92:7–15.19. Schenker ML, Yannascoli S, Baldwin KD, Ahn J, Mehta S. Does timing to operative debridement affect infectious complications in open long-bone fractures?: a systematic review. J Bone Joint Surg Am. 2012; 94:1057–64.20. Srour M, Inaba K, Okoye O, et al. Prospective evaluation of treatment of open fractures: effect of time to irrigation and debridement. JAMA Surg. 2015; 150:332–6.21. Mener A, Staley CA, Lunati MP, Pflederer J, Reisman WM, Schenker ML. Is operative debridement greater than 24 hours post-admission associated with increased likelihood of post-operative infection? J Surg Res. 2020; 247:461–8.22. Rinker B, Amspacher JC, Wilson PC, Vasconez HC. Subatmospheric pressure dressing as a bridge to free tissue transfer in the treatment of open tibia fractures. Plast Reconstr Surg. 2008; 121:1664–73.
Article23. Stannard JP, Volgas DA, Stewart R, McGwin G Jr, Alonso JE. Negative pressure wound therapy after severe open fractures: a prospective randomized study. J Orthop Trauma. 2009; 23:552–7.
Article24. Schlatterer DR, Hirschfeld AG, Webb LX. Negative pressure wound therapy in grade IIIB tibial fractures: fewer infections and fewer flap procedures? Clin Orthop Relat Res. 2015; 473:1802–11.
Article25. Virani SR, Dahapute AA, Bava SS, Muni SR. Impact of negative pressure wound therapy on open diaphyseal tibial fractures: a prospective randomized trial. J Clin Orthop Trauma. 2016; 7:256–9.
Article26. Liu X, Zhang H, Cen S, Huang F. Negative pressure wound therapy versus conventional wound dressings in treatment of open fractures: a systematic review and meta-analysis. Int J Surg. 2018; 53:72–9.
Article27. Costa ML, Achten J, Bruce J, et al. Effect of negative pressure wound therapy vs standard wound management on 12-month disability among adults with severe open fracture of the lower limb: the WOLLF randomized clinical trial. JAMA. 2018; 319:2280–8.28. Kim JH, Lee DH. Negative pressure wound therapy vs. conventional management in open tibia fractures: Systematic review and meta-analysis. Injury. 2019; 50:1764–72.
Article29. Grant-Freemantle MC, Ryan ÉJ, Flynn SO, et al. The effectiveness of negative pressure wound therapy versus conventional dressing in the treatment of open fractures: a systematic review and meta-analysis. J Orthop Trauma. 2020; 34:223–30.
Article30. Godina M. Early microsurgical reconstruction of complex trauma of the extremities. Plast Reconstr Surg. 1986; 78:285–92.
Article31. Wood T, Sameem M, Avram R, Bhandari M, Petrisor B. A systematic review of early versus delayed wound closure in patients with open fractures requiring flap coverage. J Trauma Acute Care Surg. 2012; 72:1078–85.
Article32. Liu DS, Sofiadellis F, Ashton M, MacGill K, Webb A. Early soft tissue coverage and negative pressure wound therapy optimises patient outcomes in lower limb trauma. Injury. 2012; 43:772–8.
Article33. Haykal S, Roy M, Patel A. Meta-analysis of timing for microsurgical free-flap reconstruction for lower limb injury: evaluation of the Godina principles. J Reconstr Microsurg. 2018; 34:277–92.
Article34. Cherubino M, Valdatta L, Tos P, et al. Role of negative pressure therapy as damage control in soft tissue reconstruction for open tibial fractures. J Reconstr Microsurg. 2017; 33(S 01):S08–13.
Article35. Shammas RL, Mundy LR, Truong T, et al. Identifying predictors of time to soft-tissue reconstruction following open tibia fractures. Plast Reconstr Surg. 2018; 142:1620–8.
Article36. Krug E, Berg L, Lee C, et al. Evidence-based recommendations for the use of negative pressure wound therapy in traumatic wounds and reconstructive surgery: steps towards an international consensus. Injury. 2011; 42 Suppl 1:S1–12.
Article37. Harvin WH, Stannard JP. Negative-pressure wound therapy in acute traumatic and surgical wounds in orthopaedics. JBJS Rev. 2014; 2:01874474-201404000-00001.
Article38. Robert N. Negative pressure wound therapy in orthopaedic surgery. Orthop Traumatol Surg Res. 2017; 103(1 Suppl):S99–103.
Article39. Steiert AE, Gohritz A, Schreiber TC, Krettek C, Vogt PM. Delayed flap coverage of open extremity fractures after previous vacuum-assisted closure (VAC) therapy: worse or worth? J Plast Reconstr Aesthet Surg. 2009; 62:675–83.40. Raju A, Ooi A, Ong YS, Tan BK. Traumatic lower limb injury and microsurgical free flap reconstruction with the use of negative pressure wound therapy: is timing crucial? J Reconstr Microsurg. 2014; 30:427–30.
Article41. Lee ZH, Stranix JT, Rifkin WJ, et al. Timing of microsurgical reconstruction in lower extremity trauma: an update of the Godina paradigm. Plast Reconstr Surg. 2019; 144:759–67.42. Oh HK. Damage control and provisional fixation. J Korean Fract Soc. 2010; 23:346–52.
Article43. Lenz A, Franklin GA, Cheadle WG. Systemic inflammation after trauma. Injury. 2007; 38:1336–45.
Article44. Kim JJ, Kim KH. Management of polytrauma. J Korean Orthop Assoc. 2018; 53:1–8.
Article45. D’Alleyrand JC, O’Toole RV. The evolution of damage control orthopedics: current evidence and practical applications of early appropriate care. Orthop Clin North Am. 2013; 44:499–507.46. Pape HC, Andruszkow H, Pfeifer R, Hildebrand F, Barkatali BM. Options and hazards of the early appropriate care protocol for trauma patients with major fractures: towards safe definitive surgery. Injury. 2016; 47:787–91.
Article47. Jeon BJ, Mun GH. Perspectives on reconstructive microsurgery in Korea. J Korean Med Assoc. 2011; 54:604–16.
Article48. Melvin JS, Dombroski DG, Torbert JT, Kovach SJ, Esterhai JL, Mehta S. Open tibial shaft fractures: II. Definitive management and limb salvage. J Am Acad Orthop Surg. 2010; 18:108–17.
Article49. Hallock GG. Evidence-based medicine: lower extremity acute trauma. Plast Reconstr Surg. 2013; 132:1733–41.50. Cho EH, Shammas RL, Carney MJ, et al. Muscle versus fasciocutaneous free flaps in lower extremity traumatic reconstruction: a multicenter outcomes analysis. Plast Reconstr Surg. 2018; 141:191–9.51. AlMugaren FM, Pak CJ, Suh HP, Hong JP. Best local flaps for lower extremity reconstruction. Plast Reconstr Surg Glob Open. 2020; 8:e2774.
Article52. Park JW. Reconstruction of traumatic soft tissue defect: local Flap. J Korean Fract Soc. 2010; 23:251–6.
Article53. Park JW. Reconstruction of a traumatic soft tissue defect. J Korean Fract Soc. 2015; 28:256–65.
Article54. Lee JH. Treatment of traumatic soft tissue defect: free flap. J Korean Fract Soc. 2010; 23:257–62.
Article55. Park IJ, Sur YJ, You SL. Reconstruction of the soft tissue defect on anteromedial surface of the leg using medial hemisoleus flap. Arch Reconstr Microsurg. 2014; 23:76–81.
Article56. Yaremchuk MJ, Brumback RJ, Manson PN, Burgess AR, Poka A, Weiland AJ. Acute and definitive management of traumatic osteocutaneous defects of the lower extremity. Plast Reconstr Surg. 1987; 80:1–14.
Article57. Loos MS, Freeman BG, Lorenzetti A. Zone of injury: a critical review of the literature. Ann Plast Surg. 2010; 65:573–7.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Surgical Treatment of Distal Tibia Fractures
- Two - stage Reconstruction for Open Infected Un - united Fractures of Tibia
- A Clinical Study on the Fractures of Tibia with Severe Compounding and Soft Tissue Injury
- Reconstruction of a Traumatic Soft Tissue Defect
- Contributing Factors for Nonunion in Open Tibial Fractures Treated with External Fixation