J Liver Cancer.
2020 Mar;20(1):53-59. 10.17998/jlc.20.1.53.
A Survey of Liver Cancer Specialists’ Views on the National Liver Cancer Screening Program in Korea
- Affiliations
-
- 1Department of Internal Medicine, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea
- 2Department of Internal Medicine, Korea University College of Medicine, Seoul, Korea
- 3Department of Surgery, Yonsei University College of Medicine, Seoul, Korea
- 4Department of Gastroenterology and Hepatology, Hanyang University College of Medicine, Seoul, Korea
- 5Department of Internal Medicine, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea
- 6Department of Radiology, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea
- 7Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- KMID: 2505842
- DOI: http://doi.org/10.17998/jlc.20.1.53
Abstract
- Background/Aims
To reduce the cancer burden, the Korean government initiated the National Cancer Control Plan including the National Liver Cancer Screening Program (NLCSP). Ultrasonography examinations and α-fetoprotein tests at six-month intervals are currently offered for high-risk individuals. High-risk individuals are identified by reviewing the National Health Insurance Service claims data for medical use for the past two years using International Classification of Diseases Codes for specific liver disease. We surveyed the attitudes and opinions towards the NLCSP to understand the issues surrounding the NLCSP in Korea.
Methods
Altogether, 90 Korean Liver Cancer Association members participated in online and offline surveys between November and December 2019.
Results
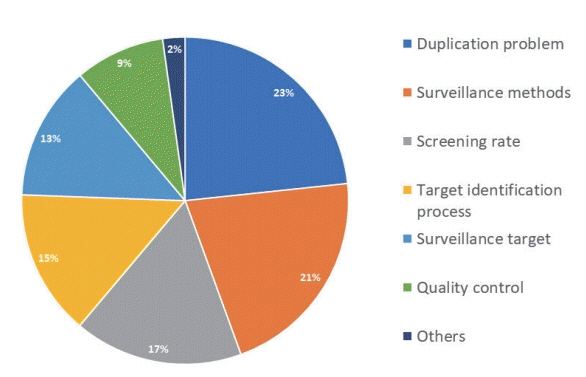
Approximately one-quarter (27%) of the survey participants rated the NLCSP as very contributing and about two-thirds (68%) as contributing to some extent toward reducing hepatocellular carcinoma (HCC)-related deaths in Korea. Most (87.8%) responded that the current process of identifying high-risk individuals needs improvement. Many (78.9%) were concerned that the current process identifies individuals who use medical services and paradoxically misses those who do not. When asked for the foremost priority for improvement, solving ‘duplication issues between the NLCSP and private clinic HCC screening practices’ was the most commonly selected choice (23.3%).
Conclusions
The survey participants positively rated the role of the NLCSP in reducing liver cancer deaths. However, many participants rated the NCLSP as needing improvement in all areas. This survey can be a relevant resource for future health policy decisions regarding the NLCSP in Korea.
Figure
Cited by 1 articles
-
Current status of ultrasonography in national cancer surveillance program for hepatocellular carcinoma in South Korea: a large-scale multicenter study
Sun Hong Yoo, Soon Sun Kim, Sang Gyune Kim, Jung Hyun Kwon, Han-Ah Lee, Yeon Seok Seo, Young Kul Jung, Hyung Joon Yim, Do Seon Song, Seong Hee Kang, Moon Young Kim, Young-Hwan Ahn, Jieun Han, Young Seok Kim, Young Chang, Soung Won Jeong, Jae Young Jang, Jeong-Ju Yoo
J Liver Cancer. 2023;23(1):189-201. doi: 10.17998/jlc.2023.03.11.
Reference
-
1. Kim BH, Park JW. Epidemiology of liver cancer in South Korea. Clin Mol Hepatol. 2018; 24:1–9.2. Kweon SS. Epidemiology of liver cancer in Korea. J Korean Med Assoc. 2019; 62:416–423.3. Yoo KY. Cancer control activities in the Republic of Korea. Jpn J Clin Oncol. 2008; 38:327–333.4. Suh M, Song S, Cho HN, Park B, Jun JK, Choi E, et al. Trends in Participation Rates for the National Cancer Screening Program in Korea, 2002-2012. Cancer Res Treat. 2017; 49:798–806.5. Kim Y, Jun JK, Choi KS, Lee HY, Park EC. Overview of the National Cancer screening programme and the cancer screening status in Korea. Asian Pac J Cancer Prev. 2011; 12:725–730.6. Korean Liver Cancer Association; National Cancer Center. 2018 Korean Liver Cancer Association-National Cancer Center Korea Practice Guidelines for the Management of Hepatocellular Carcinoma. Gut Liver. 2019; 13:227–299.7. Jung KW, Won YJ, Kong HJ, Oh CM, Shin A, Lee JS. Survival of Korean adult cancer patients by stage at diagnosis, 2006-2010: national cancer registry study. Cancer Res Treat. 2013; 45:162–171.8. Kwon JW, Tchoe HJ, Lee J, Suh JK, Lee JH, Shin S. The impact of national surveillance for liver cancer: Results from Real-World Setting in Korea. Gut Liver. 2020; 14:108–116.9. Jung M. National Cancer Screening Programs and evidence-based healthcare policy in South Korea. Health policy. 2015; 119:26–32.10. Shim JJ, Park HJ, Kim JW, Hwang EJ, Lee CK, Jang JY, et al. The Korean National Liver Cancer Surveillance Program: Experience of a Single Healthcare Center in 2011. Korean J Med. 2013; 84:672–680.11. Choi IS, Oh CH, Park SY, Ahn SE, Park SJ, Choi HR, et al. Incidence of primary liver cancer in subjects with chronic hepatitis B in Korean National Liver Cancer Screening Program. J Liver Cancer. 2017; 17:136–143.12. Suh M, Choi KS, Park B, Lee YY, Jun JK, Lee DH, et al. Trends in Cancer Screening Rates among Korean Men and Women: Results of the Korean National Cancer Screening Survey, 2004-2013. Cancer Res Treat. 2016; 48:1–10.13. Choi MH, Jung SE, Choi JI, Jeong WK, Kim HC, Kim Y, et al. Quality management of ultrasound surveillance for hepatocellular carcinoma under the Korean National Cancer Screening Program. J Ultrasound Med. 2018; 37:245–254.14. Kim DY, Kim HJ, Jeong SE, Kim SG, Kim HJ, Sinn DH, et al. The Korean guideline for hepatocellular carcinoma surveillance. J Korean Med Assoc. 2015; 58:385–397.15. Na SK, Song BC. Development and surveillance of hepatocellular carcinoma in patients with sustained virologic response after antiviral therapy for chronic hepatitis C. Clin Mol Hepatol. 2019; 25:234–244.16. Zhang X, Wong GL, Wong VW. Application of transient elastography in nonalcoholic fatty liver disease. Clin Mol Hepatol. 2019; Nov. 8. . doi: 10.3350/cmh.2019.0001n. [Epub ahead of print].
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Trends in Cancer Screening Rates among Korean Men and Women: Results from the Korean National Cancer Screening Survey (KNCSS), 2004-2011
- Trends in Participation Rates for the National Cancer Screening Program in Korea, 2002-2012
- Epidemiology of liver cancer in Korea
- Trends in Cancer Screening Rates among Korean Men and Women: Results from the Korean National Cancer Screening Survey (KNCSS), 2004-2010
- Trends in Cancer Screening Rates among Korean Men and Women: Results of the Korean National Cancer Screening Survey, 2004–2018