J Korean Assoc Oral Maxillofac Surg.
2020 Aug;46(4):220-227. 10.5125/jkaoms.2020.46.4.220.
Oral rehabilitation of Papillon–Lefèvre syndrome patients by dental implants: a systematic review
- Affiliations
-
- 1Department of Periodontics, Dental School of Shahid Beheshti University of Medical Sciences, Tehran, Iran
- 2Department of Oral and Maxillofacial Pathology, School of Dentistry, Shahid Beheshti University of Medical Sciences, Tehran, Iran
- 3Dental Research Center, Research Institute of Dental Sciences, Shahid Beheshti University of Medical Sciences, Tehran, Iran
- 4Community Oral Health Department, School of Dentistry, Shahid Beheshti University of Medical Sciences, Tehran, Iran
- 5Department of Biostatistics, School of Allied Medical Sciences, Shahid Beheshti University of Medical Sciences, Tehran, Iran
- KMID: 2505433
- DOI: http://doi.org/10.5125/jkaoms.2020.46.4.220
Abstract
Objectives
Papillon–Lefèvre syndrome (PLS) is a rare autosomal recessive disorder. These patients lose their teeth at a young age and are in need of prosthetic rehabilitation. The aim of this systematic review was to assess the success of dental implant placement in these patients.
Materials and Methods
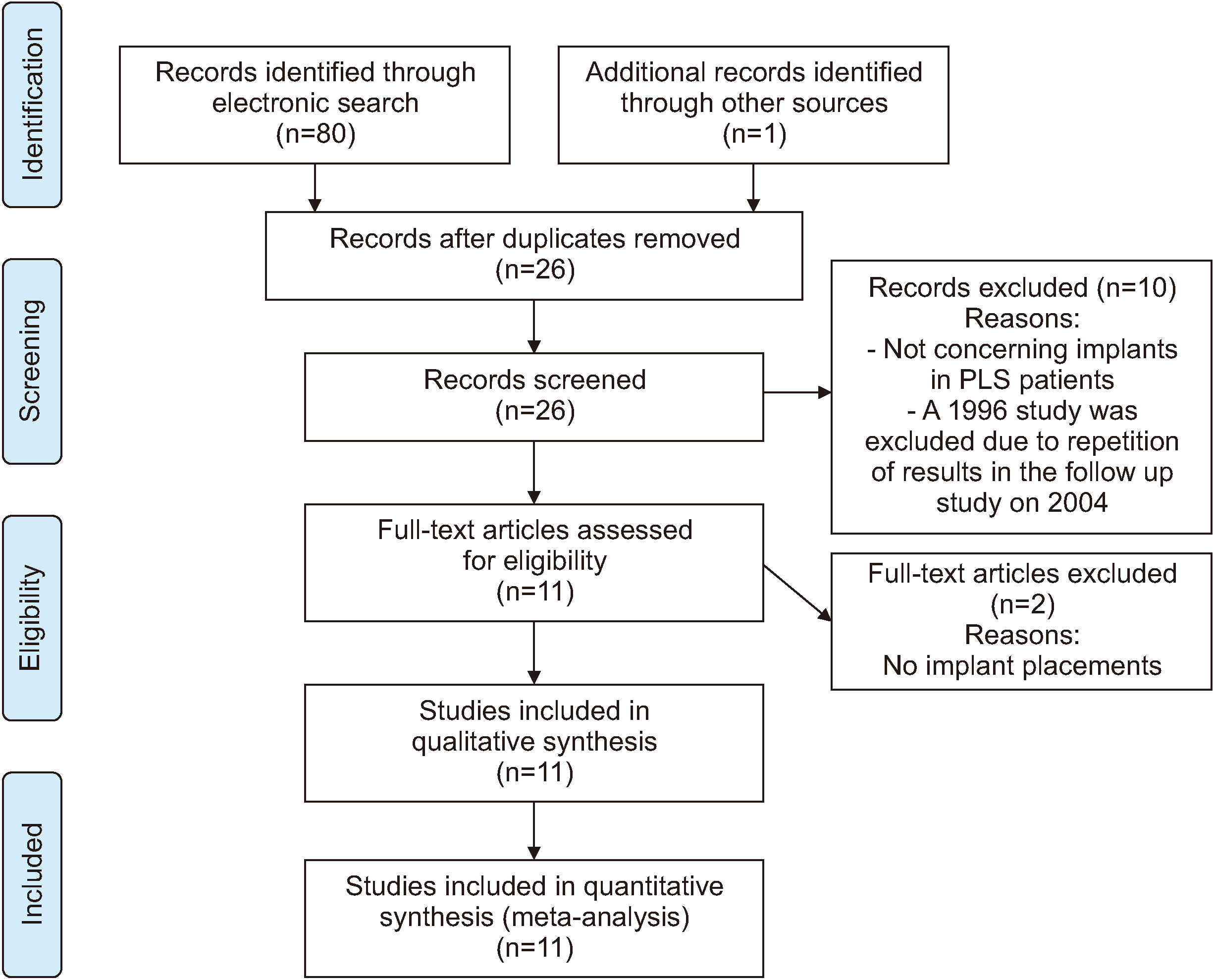
An electronic search was performed in PubMed Central, Scopus, and Web of Science using the keyword “Papillon–Lefèvre syndrome” AND “dental implant” OR “prosthodontics”. Articles reporting implant placement in patients with PLS until July 2019 were included.
Results
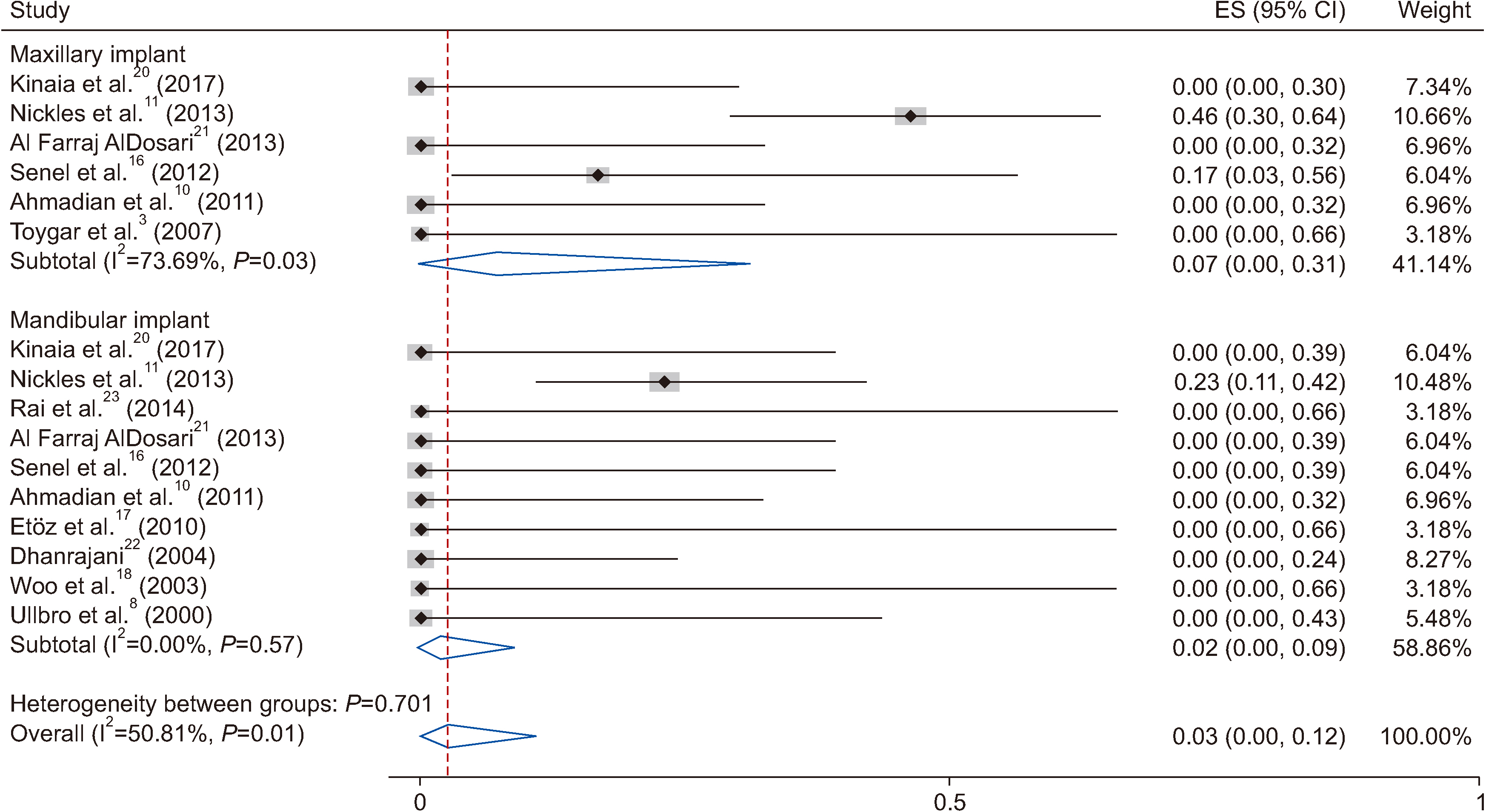
Assessment of the included 11 articles reporting 15 cases showed 136 implant placements in these patients. Implant failure occurred in 3 patients (20 implants). The peri-implantitis and failure rate was higher in the maxilla. Meta-analysis showed the probability of failure to be 7% (95% confidence interval [CI] 0%-31%) for maxillary implants and 2% (95% CI 0%-9%) for mandibular implants. The follow-up time ranged between 1 and 20 years. Healing after bone graft and implant placement in these patients was uneventful.
Conclusion
Dental implants may be a viable treatment option for PLS patients. Implantation can help preserve alveolar bone if the patients’ immunological and growing conditions are well-considered and proper oral hygiene and compliance with the maintenance program are continued.
Keyword
Figure
Reference
-
References
1. Bohner L, Hanisch M, Kleinheinz J, Jung S. 2019; Dental implants in growing patients: a systematic review. Br J Oral Maxillofac Surg. 57:397–406. https://doi.org/10.1016/j.bjoms.2019.04.011 . DOI: 10.1016/j.bjoms.2019.04.011. PMID: 31076220.
Article2. Heuberer S, Dvorak G, Mayer C, Watzek G, Zechner W. 2015; Dental implants are a viable alternative for compensating oligodontia in adolescents. Clin Oral Implants Res. 26:e22–7. https://doi.org/10.1111/clr.12323 . DOI: 10.1111/clr.12323. PMID: 24383943.
Article3. Toygar HU, Kircelli C, Firat E, Guzeldemir E. 2007; Combined therapy in a patient with Papillon-Lefèvre syndrome: a 13-year follow-up. J Periodontol. 78:1819–24. https://doi.org/10.1902/jop.2007.070004 . DOI: 10.1902/jop.2007.070004. PMID: 17760554.
Article4. Machado RA, Cuadra-Zelaya FJM, Martelli-Júnior H, Miranda RT, Casarin RCV, Corrêa MG, et al. 2019; Clinical and molecular analysis in Papillon-Lefèvre syndrome. Am J Med Genet A. 179:2124–31. https://doi.org/10.1002/ajmg.a.61285 . DOI: 10.1002/ajmg.a.61285. PMID: 31282082.
Article5. Hart TC, Shapira L. 1994; Papillon-Lefèvre syndrome. Periodontol 2000. 6:88–100. https://doi.org/10.1111/j.1600-0757.1994.tb00029.x . DOI: 10.1111/j.1600-0757.1994.tb00029.x. PMID: 9673173.
Article6. Nagy N, Vályi P, Csoma Z, Sulák A, Tripolszki K, Farkas K, et al. 2014; CTSC and Papillon-Lefèvre syndrome: detection of recurrent mutations in Hungarian patients, a review of published variants and database update. Mol Genet Genomic Med. 2:217–28. https://doi.org/10.1002/mgg3.61 . DOI: 10.1002/mgg3.61. PMID: 24936511. PMCID: PMC4049362.
Article7. Roberts H, White P, Dias I, McKaig S, Veeramachaneni R, Thakker N, et al. 2016; Characterization of neutrophil function in Papillon-Lefèvre syndrome. J Leukoc Biol. 100:433–44. https://doi.org/10.1189/jlb.5A1015-489R . DOI: 10.1189/jlb.5A1015-489R. PMID: 26957212.
Article8. Ullbro C, Crossner CG, Lundgren T, Stålblad PA, Renvert S. 2000; Osseointegrated implants in a patient with Papillon-Lefèvre syndrome. A 4 1/2-year follow up. J Clin Periodontol. 27:951–4. https://doi.org/10.1034/j.1600-051x.2000.027012951.x . DOI: 10.1034/j.1600-051x.2000.027012951.x. PMID: 11140563.
Article9. Tinanoff N, Tempro P, Maderazo EG. 1995; Dental treatment of Papillon-Lefèvre syndrome: 15-year follow-up. J Clin Periodontol. 22:609–12. https://doi.org/10.1111/j.1600-051x.1995.tb00813.x . DOI: 10.1111/j.1600-051X.1995.tb00813.x. PMID: 8583017.
Article10. Ahmadian L, Monzavi A, Arbabi R, Hashemi HM. 2011; Full-mouth rehabilitation of an edentulous patient with Papillon-Lefèvre syndrome using dental implants: a clinical report. J Prosthodont. 20:643–8. https://doi.org/10.1111/j.1532-849X.2011.00768.x . DOI: 10.1111/j.1532-849X.2011.00768.x. PMID: 21974795.
Article11. Nickles K, Schacher B, Ratka-Krüger P, Krebs M, Eickholz P. 2013; Long-term results after treatment of periodontitis in patients with Papillon-Lefèvre syndrome: success and failure. J Clin Periodontol. 40:789–98. https://doi.org/10.1111/jcpe.12120 . DOI: 10.1111/jcpe.12120. PMID: 23829197.
Article12. Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group. 2009; Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 151:264–9. https://doi.org/10.1371/journal.pmed.1000097 . DOI: 10.1371/journal.pmed.1000097. PMID: 19621072. PMCID: PMC2707599.
Article13. Riley DS, Barber MS, Kienle GS, Aronson JK, von Schoen-Angerer T, Tugwell P, et al. 2017; CARE guidelines for case reports: explanation and elaboration document. J Clin Epidemiol. 89:218–35. W64. https://doi.org/10.1016/j.jclinepi.2017.04.026 . DOI: 10.1016/j.jclinepi.2017.04.026. PMID: 28529185.
Article14. De Vree H, Steenackers K, De Boever JA. 2000; Periodontal treatment of rapid progressive periodontitis in 2 siblings with Papillon-Lefèvre syndrome: 15-year follow-up. J Clin Periodontol. 27:354–60. https://doi.org/10.1034/j.1600-051x.2000.027005354.x . DOI: 10.1034/j.1600-051x.2000.027005354.x. PMID: 10847540.
Article15. Pacheco JJ, Coelho C, Salazar F, Contreras A, Slots J, Velazco CH. 2002; Treatment of Papillon-Lefèvre syndrome periodontitis. J Clin Periodontol. 29:370–4. https://doi.org/10.1034/j.1600-051x.2002.290414.x . DOI: 10.1034/j.1600-051X.2002.290414.x. PMID: 11966936.
Article16. Senel FC, Altintas NY, Bagis B, Cankaya M, Pampu AA, Satiroglu I, et al. 2012; A 3-year follow-up of the rehabilitation of Papillon-Lefèvre syndrome by dental implants. J Oral Maxillofac Surg. 70:163–7. https://doi.org/10.1016/j.joms.2011.03.058 . DOI: 10.1016/j.joms.2011.03.058. PMID: 21802810.
Article17. Etöz OA, Ulu M, Kesim B. 2010; Treatment of patient with Papillon-Lefèvre syndrome with short dental implants: a case report. Implant Dent. 19:394–9. https://doi.org/10.1097/ID.0b013e3181ed0798 . DOI: 10.1097/ID.0b013e3181ed0798. PMID: 20881810.
Article18. Woo I, Brunner DP, Yamashita DD, Le BT. 2003; Dental implants in a young patient with Papillon-Lefèvre syndrome: a case report. Implant Dent. 12:140–4. https://doi.org/10.1097/01.id.0000041223.08656.a7 . DOI: 10.1097/01.ID.0000041223.08656.A7. PMID: 12861881.
Article19. Wiebe CB, Häkkinen L, Putnins EE, Walsh P, Larjava HS. 2001; Successful periodontal maintenance of a case with Papillon-Lefèvre syndrome: 12-year follow-up and review of the literature. J Periodontol. 72:824–30. https://doi.org/10.1902/jop.2001.72.6.824 . DOI: 10.1902/jop.2001.72.6.824. PMID: 11453246.
Article20. Kinaia BM, Hope K, Zuhaili A, Tulasne JF. 2017; Full-mouth rehabilitation with calvarium bone grafts and dental implants for a Papillon-Lefèvre syndrome patient: case report. Int J Oral Maxillofac Implants. 32:e259–64. https://doi.org/10.11607/jomi.6282 . DOI: 10.11607/jomi.6282. PMID: 29140387.
Article21. Al Farraj AlDosari A. 2013; Oral rehabilitation of a case of Papillon-Lefèvre syndrome with dental implants. Saudi Med J. 34:424–7.22. Dhanrajani PJ. 2003; Re: "Dental implants in a young patient with Papillon-Lefèvre syndrome: a case report" (Implant Dent. 2003;12(2):140-4). Implant Dent. 13:280. https://doi.org/10.1097/01.id.0000148561.03643.75 . DOI: 10.1097/01.id.0000148561.03643.75. PMID: 15591986.
Article23. Rai R, Kumar A, Deshpande V. 2014; Papillon-Lefèvre syndrome - the prosthodontic management. J Pierre Fauchard Acad. 28:23–7. https://doi.org/10.1016/j.jpfa.2014.03.002 . DOI: 10.1016/j.jpfa.2014.03.002.
Article24. Oesterle LJ, Cronin RJ Jr Jr, Ranly DM. 1993; Maxillary implants and the growing patient. Int J Oral Maxillofac Implants. 8:377–87.25. Chrcanovic BR. 2018; Dental implants in patients with ectodermal dysplasia: a systematic review. J Craniomaxillofac Surg. 46:1211–7. https://doi.org/10.1016/j.jcms.2018.05.038 . DOI: 10.1016/j.jcms.2018.05.038. PMID: 29884311.
Article26. Cortellini S, Favril C, De Nutte M, Teughels W, Quirynen M. 2019; Patient compliance as a risk factor for the outcome of implant treatment. Periodontol 2000. 81:209–25. https://doi.org/10.1111/prd.12293 . DOI: 10.1111/prd.12293. PMID: 31407429.
Article27. Lin CY, Chen Z, Pan WL, Wang HL. 2019; The effect of supportive care in preventing peri-implant diseases and implant loss: a systematic review and meta-analysis. Clin Oral Implants Res. 30:714–24. https://doi.org/10.1111/clr.13496 . DOI: 10.1111/clr.13496. PMID: 31231883.
Article28. Atarbashi-Moghadam F, Atarbashi-Moghadam S, Namdari M, Shahrabi-Farahani S. 2018; Reactive oral lesions associated with dental implants. A systematic review. J Investig Clin Dent. 9:e12342. https://doi.org/10.1111/jicd.12342 . DOI: 10.1111/jicd.12342. PMID: 29752778.
Article29. Dreyer H, Grischke J, Tiede C, Eberhard J, Schweitzer A, Toikkanen SE, et al. 2018; Epidemiology and risk factors of peri-implantitis: a systematic review. J Periodontal Res. 53:657–81. https://doi.org/10.1111/jre.12562 . DOI: 10.1111/jre.12562. PMID: 29882313.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Atypical Maxillary Sinusitis Accompanied with Papillon-Lefevre Syndrome
- Two Cases of Papillon-Lefevre Syndrome
- Novel Compound Heterozygous Mutations in CTSC Gene in a Chinese Family with Papillon–Lefevre Syndrome
- THE STUDY ON THE USE OF DENTAL IMPLANTS FOR FUNCTIONAL REHABILITATION OF ORAL TUMOR PATIENTS
- Bone loss-related factors in tissue and bone level dental implants: a systematic review of clinical trials