Clin Endosc.
2020 Jul;53(4):458-465. 10.5946/ce.2019.121.
Efficacy and Safety of Endoscopic Treatment for Gastrointestinal Stromal Tumors in the Upper Gastrointestinal Tract
- Affiliations
-
- 1Department of Gastroenterology, Southeast University Affiliated Zhongda Hospital, Nanjing, China
- 2Department of Orthopedics, Southeast University Affiliated Zhongda Hospital, Nanjing, China
- KMID: 2504950
- DOI: http://doi.org/10.5946/ce.2019.121
Abstract
- Background/Aims
Endoscopic treatment (ET) has been applied for decades to treat subepithelial tumors, including gastrointestinal stromal tumors (GISTs). However, the efficacy of ET remains debatable. In this study, we evaluated the efficacy and safety of ET for GISTs in the upper gastrointestinal tract.
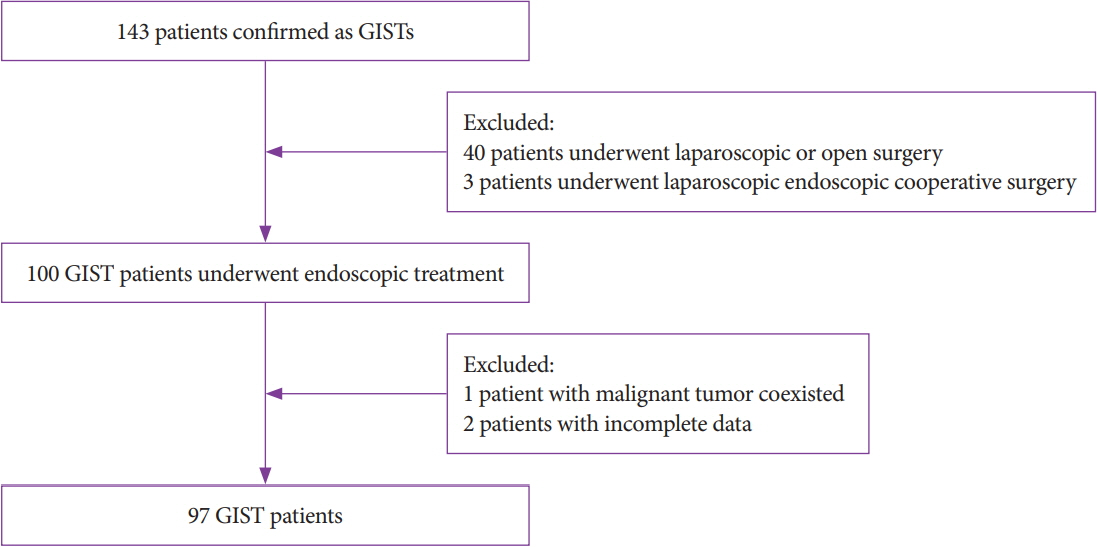
Methods
This retrospective single-center study included 97 patients who underwent ET. All patients were enrolled from July 2014 to July 2018. Parameters such as demographics, size, resection margin, complications, pathological features, procedure time, total cost, and follow-up were investigated and analyzed.
Results
Our study achieved 100% en bloc resection and 77.4% (72/93) R0 resection. The most common location was the fundus with a mean tumor size of 2.1±1.43 cm. The mean age, procedure time, hospital stay, and cost were 59.7±11.29 years, 64.7±35.23 minutes, 6.8 days, and 5,337 dollars, respectively. According to National Institutes of Health classification, 63 (64.9%), 26 (26.8%), 5 (5.2%), and 3 (3.1%) patients belonged to the very low, low, intermediate, and high risk classification, respectively. Immunohistochemistry results showed a 100% positive rate of CD34, DOG-1, CD117, and Ki67. A mean follow-up of 21.3±13.0 months showed no recurrence or metastasis.
Conclusions
ET is effective and safe for curative removal of GISTs in the upper gastrointestinal tract, and it can be a treatment of choice for patients with no metastasis.
Keyword
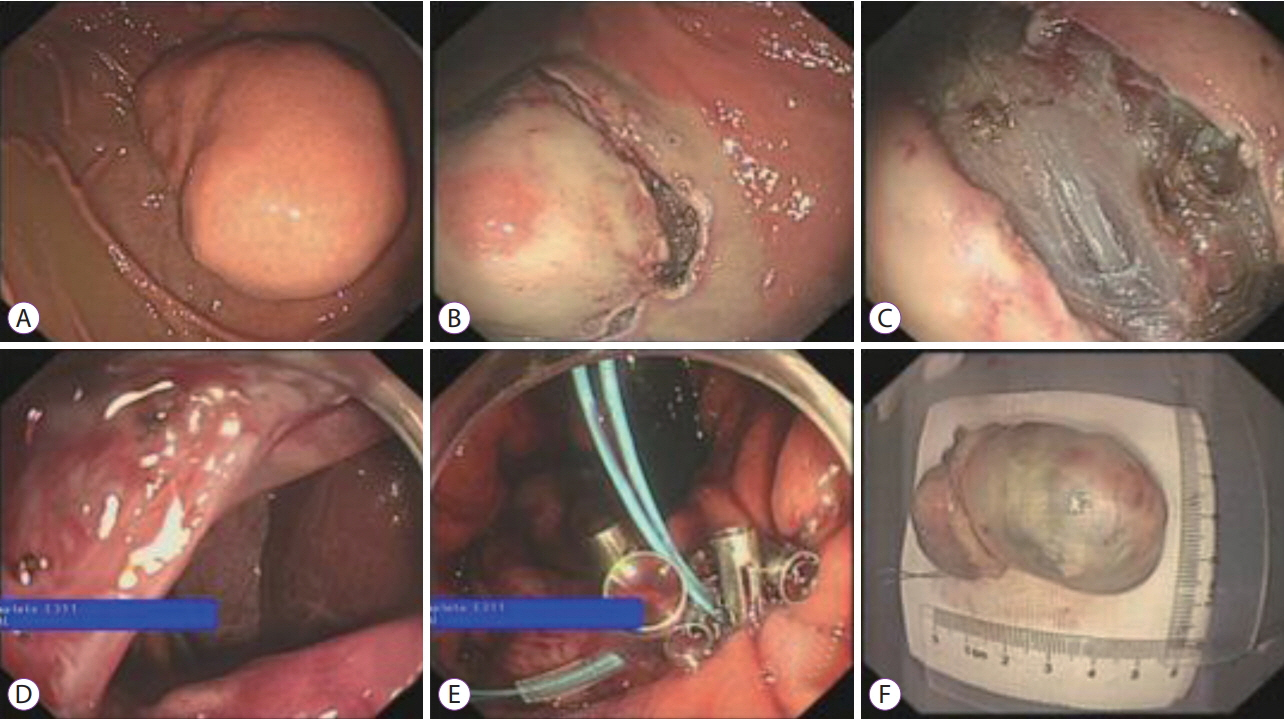
Figure
Cited by 1 articles
-
Endoscopic Treatment for Gastrointestinal Stromal Tumors in the Upper Gastrointestinal Tract
In Kyung Yoo, Joo Young Cho
Clin Endosc. 2020;53(4):383-384. doi: 10.5946/ce.2020.122.
Reference
-
1. Nilsson B, Bümming P, Meis-Kindblom JM, et al. Gastrointestinal stromal tumors: the incidence, prevalence, clinical course, and prognostication in the preimatinib mesylate era--a population-based study in western Sweden. Cancer. 2005; 103:821–829.2. Alvarado-Cabrero I, Vázquez G, Sierra Santiesteban FI, Hernández-Hernández DM, Pompa AZ. Clinicopathologic study of 275 cases of gastrointestinal stromal tumors: the experience at 3 large medical centers in Mexico. Ann Diagn Pathol. 2007; 11:39–45.
Article3. Chhoda A, Jain D, Surabhi VR, Singhal S. Contrast enhanced harmonic endoscopic ultrasound: a novel approach for diagnosis and management of gastrointestinal stromal tumors. Clin Endosc. 2018; 51:215–221.
Article4. Fletcher CD, Berman JJ, Corless C, et al. Diagnosis of gastrointestinal stromal tumors: a consensus approach. Int J Surg Pathol. 2002; 10:81–89.
Article5. ESMO/European Sarcoma Network Working Group. Gastrointestinal stromal tumours: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2014; 25 Suppl 3:iii21–iii26.6. Yin X, Yin Y, Chen H, et al. Comparison analysis of three different types of minimally invasive procedures for gastrointestinal stromal tumors ≤5 cm. J Laparoendosc Adv Surg Tech A. 2018; 28:58–64.7. He G, Wang J, Chen B, et al. Feasibility of endoscopic submucosal dissection for upper gastrointestinal submucosal tumors treatment and value of endoscopic ultrasonography in pre-operation assess and post-operation follow-up: a prospective study of 224 cases in a single medical center. Surg Endosc. 2016; 30:4206–4213.
Article8. Andalib I, Yeoun D, Reddy R, Xie S, Iqbal S. Endoscopic resection of gastric gastrointestinal stromal tumors originating from the muscularis propria layer in North America: methods and feasibility data. Surg Endosc. 2018; 32:1787–1792.
Article9. Li J, Tang J, Lua GW, et al. Safety and efficacy of endoscopic submucosal dissection of large (≥3 cm) subepithelial tumors located in the cardia. Surg Endosc. 2017; 31:5183–5191.10. Kim HH. Endoscopic treatment for gastrointestinal stromal tumor: advantages and hurdles. World J Gastrointest Endosc. 2015; 7:192–205.
Article11. Marcella C, Shi RH, Sarwar S. Clinical overview of GIST and its latest management by endoscopic resection in upper GI: a literature review. Gastroenterol Res Pract. 2018; 2018:6864256.
Article12. Miettinen M, Sobin LH, Lasota J. Gastrointestinal stromal tumors of the stomach: a clinicopathologic, immunohistochemical, and molecular genetic study of 1765 cases with long-term follow-up. Am J Surg Pathol. 2005; 29:52–68.13. DeMatteo RP, Lewis JJ, Leung D, Mudan SS, Woodruff JM, Brennan MF. Two hundred gastrointestinal stromal tumors: recurrence patterns and prognostic factors for survival. Ann Surg. 2000; 231:51–58.14. Demetri GD, von Mehren M, Antonescu CR, et al. NCCN task force report: update on the management of patients with gastrointestinal stromal tumors. J Natl Compr Canc Netw. 2010; 8 Suppl 2:S1–S41. quiz S42-S44.
Article15. Nishida T, Hirota S, Yanagisawa A, et al. Clinical practice guidelines for gastrointestinal stromal tumor (GIST) in Japan: English version. Int J Clin Oncol. 2008; 13:416–430.
Article16. Puchalski CM. Spirituality in the cancer trajectory. Ann Oncol. 2012; 23 Suppl 3:49–55.
Article17. Miettinen M, Lasota J. Gastrointestinal stromal tumors: pathology and prognosis at different sites. Semin Diagn Pathol. 2006; 23:70–83.
Article18. Hiki N, Yamamoto Y, Fukunaga T, et al. Laparoscopic and endoscopic cooperative surgery for gastrointestinal stromal tumor dissection. Surg Endosc. 2008; 22:1729–1735.
Article19. Namikawa T, Hanazaki K. Laparoscopic endoscopic cooperative surgery as a minimally invasive treatment for gastric submucosal tumor. World J Gastrointest Endosc. 2015; 7:1150–1156.
Article20. He Z, Sun C, Zheng Z, et al. Endoscopic submucosal dissection of large gastrointestinal stromal tumors in the esophagus and stomach. J Gastroenterol Hepatol. 2013; 28:262–267.
Article21. Zhang J, Huang K, Ding S, et al. Clinical applicability of various treatment approaches for upper gastrointestinal submucosal tumors. Gastroenterol Res Pract. 2016; 2016:9430652.
Article22. Chun SY, Kim KO, Park DS, et al. Endoscopic submucosal dissection as a treatment for gastric subepithelial tumors that originate from the muscularis propria layer: a preliminary analysis of appropriate indications. Surg Endosc. 2013; 27:3271–3279.
Article23. Lee CM, Kim HH. Minimally invasive surgery for submucosal (subepithelial) tumors of the stomach. World J Gastroenterol. 2014; 20:13035–13043.
Article24. Chu YY, Lien JM, Tsai MH, et al. Modified endoscopic submucosal dissection with enucleation for treatment of gastric subepithelial tumors originating from the muscularis propria layer. BMC Gastroenterol. 2012; 12:124.
Article25. Zhang Y, Ye LP, Zhou XB, et al. Safety and efficacy of endoscopic excavation for gastric subepithelial tumors originating from the muscularis propria layer: results from a large study in China. J Clin Gastroenterol. 2013; 47:689–694.26. Inoue H, Ikeda H, Hosoya T, et al. Submucosal endoscopic tumor resection for subepithelial tumors in the esophagus and cardia. Endoscopy. 2012; 44:225–230.
Article27. Schmidt A, Bauder M, Riecken B, von Renteln D, Muehleisen H, Caca K. Endoscopic full-thickness resection of gastric subepithelial tumors: a single-center series. Endoscopy. 2015; 47:154–158.
Article28. Xu MD, Cai MY, Zhou PH, et al. Submucosal tunneling endoscopic resection: a new technique for treating upper GI submucosal tumors originating from the muscularis propria layer (with videos). Gastrointest Endosc. 2012; 75:195–199.
Article29. Lu J, Zheng M, Jiao T, Wang Y, Lu X. Transcardiac tunneling technique for endoscopic submucosal dissection of gastric fundus tumors arising from the muscularis propria. Endoscopy. 2014; 46:888–892.
Article30. Li QL, Chen WF, Zhang C, et al. Clinical impact of submucosal tunneling endoscopic resection for the treatment of gastric submucosal tumors originating from the muscularis propria layer (with video). Surg Endosc. 2015; 29:3640–3646.
Article31. Tan Y, Tang X, Guo T, et al. Comparison between submucosal tunneling endoscopic resection and endoscopic full-thickness resection for gastric stromal tumors originating from the muscularis propria layer. Surg Endosc. 2017; 31:3376–3382.
Article32. Gong W, Xiong Y, Zhi F, Liu S, Wang A, Jiang B. Preliminary experience of endoscopic submucosal tunnel dissection for upper gastrointestinal submucosal tumors. Endoscopy. 2012; 44:231–235.
Article33. Ye LP, Zhang Y, Mao XL, Zhu LH, Zhou X, Chen JY. Submucosal tunneling endoscopic resection for small upper gastrointestinal subepithelial tumors originating from the muscularis propria layer. Surg Endosc. 2014; 28:524–530.
Article34. Tamura T, Kitano M. Contrast enhanced endoscopic ultrasound imaging for gastrointestinal subepithelial tumors. Clin Endosc. 2019; 52:306–313.
Article35. Kantsevoy SV, Bitner M, Mitrakov AA, Thuluvath PJ. Endoscopic suturing closure of large mucosal defects after endoscopic submucosal dissection is technically feasible, fast, and eliminates the need for hospitalization (with videos). Gastrointest Endosc. 2014; 79:503–507.
Article36. Vance RB, Agrawal D. Endoscopic repair of gastric perforation with an over-the-scope clip after endoscopic mucosal resection. Gastrointest Endosc. 2014; 80:1205–1206.
Article37. Yahagi N, Nishizawa T, Akimoto T, Ochiai Y, Goto O. New endoscopic suturing method: string clip suturing method. Gastrointest Endosc. 2016; 84:1064–1065.
Article38. Nishizawa T, Uraoka T, Suzuki H, et al. New endoscopic suturing method: slip knot clip suturing. Gastrointest Endosc. 2015; 82:570–571.
Article39. Nishizawa T, Uraoka T, Sagara S, et al. Endoscopic slipknot clip suturing method: an ex vivo feasibility study (with video). Gastrointest Endosc. 2016; 83:447–450.40. Nishizawa T, Ochiai Y, Uraoka T, et al. Endoscopic slip-knot clip suturing method: prospective pilot study (with video). Gastrointest Endosc. 2017; 85:433–437.
Article41. Akimoto T, Goto O, Sasaki M, et al. “Hold-and-drag” closure technique using repositionable clips for large mucosal defects after colonic endoscopic submucosal dissection. Endosc Int Open. 2016; 4:E1068–E1072.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Current Techniques for Treating Gastrointestinal Stromal Tumors in the Upper Gastrointestinal Tract
- Endoscopic Treatment of Submucosal Tumor from Upper Gastrointestinal Tract
- The Role of Endoscopic Ultrasonography in Differentiating Benign and Malignant Stromal Tumors of Upper Gastrointestinal Tract
- Endoscopic Treatment for Gastrointestinal Stromal Tumors in the Upper Gastrointestinal Tract
- A case of huge Gastrointestinal stromal tumor masquerading as an ovarian malignancy