Ann Surg Treat Res.
2020 Aug;99(2):110-117. 10.4174/astr.2020.99.2.110.
Retrorectal tumor: a single-center 10-years’ experience
- Affiliations
-
- 1Department of General Surgery, Çukurova University Faculty of Medicine, Adana, Turkey
- 2Department of Orthopedics and Traumatology, Çukurova University Faculty of Medicine, Adana, Turkey
- 3Department of Orthopedics and Traumatology, Koç University Faculty of Medicine, Istanbul, Turkey
- 4Department of Plastic and Reconstructive Surgery, Çukurova University Faculty of Medicine, Adana, Turkey
- KMID: 2504823
- DOI: http://doi.org/10.4174/astr.2020.99.2.110
Abstract
- Purpose
Retrorectal tumors (RTs) are a rare incidence and recommendations on the ideal surgical approaches are lacking. This study aimed to evaluate outcomes and follow-up results of patients undergoing excision of RTs at our institution.
Methods
A retrospective review was conducted for undergoing surgery for RT between January 2009 and January 2019. Demographic characteristics, presenting symptoms, preoperative diagnostic tests, surgical procedures, histopathological results, intraoperative and postoperative complications, postoperative hospital stay, postoperative 30-day mortality, 90-day unplanned readmission rate, and long-term outcomes were evaluated.
Results
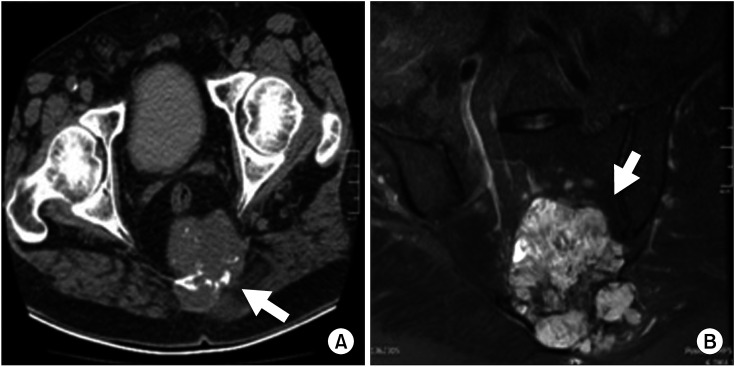
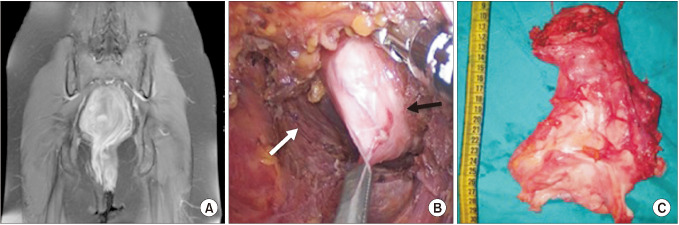
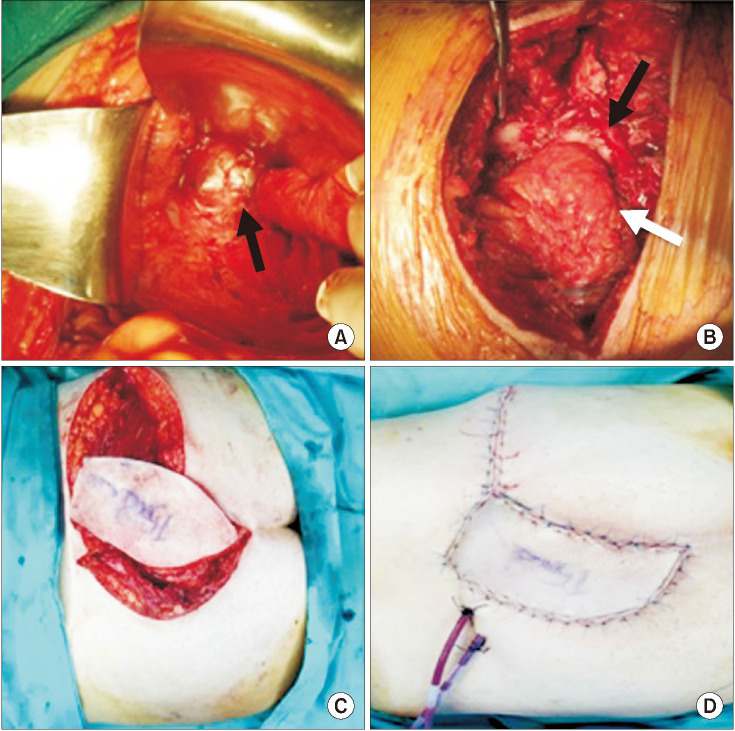
Twenty patients with a mean age of 48.3 ± 14.2 were analyzed. The most common presenting complaint was perineal pain (35.0%). Magnetic resonance imaging and computed tomography was preferred in 18 and 2 patients, respectively. Tumor localization was below the level of the third sacral vertebrae in 14 patients for whom the posterior surgical approach was used. No postoperative mortality was recorded at the end of follow-up of 53.8 ± 40 months. Mean length of postoperative hospital stay was 8.6 ± 9.4 days. Ten percent of the patients had unplanned hospital readmission within 90 days after discharge. Recurrence developed in 1 patient, for whom pathology were reported as chordoma.
Conclusion
RT should be managed by a multidisciplinary team given the complexity and heterogeneity of these tumors despite the fact that the majority are benign. A good understanding of pelvic anatomy and characterization of lesions through detailed radiological imaging is crucial to optimize surgical planning. Complete surgical resection is key for prolonged disease-free and overall survival of patients diagnosed with RTs.
Keyword
Figure
Reference
-
1. Jao SW, Beart RW Jr, Spencer RJ, Reiman HM, Ilstrup DM. Retrorectal tumors: Mayo Clinic experience, 1960-1979. Dis Colon Rectum. 1985; 28:644–652. PMID: 2996861.2. Bosca A, Pous S, Artes MJ, Gomez F, Granero Castro P, Garcia-Granero E. Tumours of the retrorectal space: management and outcome of a heterogeneous group of diseases. Colorectal Dis. 2012; 14:1418–1423. PMID: 22390258.3. Uhlig BE, Johnson RL. Presacral tumors and cysts in adults. Dis Colon Rectum. 1975; 18:581–589. PMID: 1181162.4. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004; 240:205–213. PMID: 15273542.5. Hobson KG, Ghaemmaghami V, Roe JP, Goodnight JE, Khatri VP. Tumors of the retrorectal space. Dis Colon Rectum. 2005; 48:1964–1974. PMID: 15981068.6. Hassan I, Wietfeldt ED. Presacral tumors: diagnosis and management. Clin Colon Rectal Surg. 2009; 22:84–93. PMID: 20436832.7. Abel ME, Nelson R, Prasad ML, Pearl RK, Orsay CP, Abcarian H. Parasacrococcygeal approach for the resection of retrorectal developmental cysts. Dis Colon Rectum. 1985; 28:855–858. PMID: 4053899.8. Bouts C, Van der Speeten K. A single center retrospective analysis of Kraske’s transsacral approach: a review. Surg Sci. 2014; 5:454–466.9. Baek SK, Hwang GS, Vinci A, Jafari MD, Jafari F, Moghadamyeghaneh Z, et al. Retrorectal tumors: a comprehensive literature review. World J Surg. 2016; 40:2001–2015. PMID: 27083451.10. Hopper L, Eglinton TW, Wakeman C, Dobbs BR, Dixon L, Frizelle FA. Progress in the management of retrorectal tumours. Colorectal Dis. 2016; 18:410–417. PMID: 26367385.11. Chereau N, Lefevre JH, Meurette G, Mourra N, Shields C, Parc Y, et al. Surgical resection of retrorectal tumours in adults: long-term results in 47 patients. Colorectal Dis. 2013; 15:e476–e482. PMID: 23601092.12. Lev-Chelouche D, Gutman M, Goldman G, Even-Sapir E, Meller I, Issakov J, et al. Presacral tumors: a practical classification and treatment of a unique and heterogeneous group of diseases. Surgery. 2003; 133:473–478. PMID: 12773974.13. Macafee DA, Sagar PM, El-Khoury T, Hyland R. Retrorectal tumours: optimization of surgical approach and outcome. Colorectal Dis. 2012; 14:1411–1417. PMID: 22339762.14. Sagar AJ, Tan WS, Codd R, Fong SS, Sagar PM. Surgical strategies in the management of recurrent retrorectal tumours. Tech Coloproctol. 2014; 18:1023–1027. PMID: 24925354.15. Merchea A, Larson DW, Hubner M, Wenger DE, Rose PS, Dozois EJ. The value of preoperative biopsy in the management of solid presacral tumors. Dis Colon Rectum. 2013; 56:756–760. PMID: 23652750.16. Neale JA. Retrorectal tumors. Clin Colon Rectal Surg. 2011; 24:149–160. PMID: 22942797.17. Ucar AD, Yoldas T, Oymaci E, Erkan N, Caliskan C, Yildirim M, et al. Totally curative surgical resection of retrorectal tumors. Hepatogastroenterology. 2015; 62:606–611. PMID: 26897938.18. Woodfield JC, Chalmers AG, Phillips N, Sagar PM. Algorithms for the surgical management of retrorectal tumours. Br J Surg. 2008; 95:214–221. PMID: 17933000.19. Fuchs B, Dickey ID, Yaszemski MJ, Inwards CY, Sim FH. Operative management of sacral chordoma. J Bone Joint Surg Am. 2005; 87:2211–2216. PMID: 16203885.20. Stacchiotti S, Longhi A, Ferraresi V, Grignani G, Comandone A, Stupp R, et al. Phase II study of imatinib in advanced chordoma. J Clin Oncol. 2012; 30:914–920. PMID: 22331945.21. Casali PG, Stacchiotti S, Grosso F, Messina A, Crippa F, Tamborini E, et al. Adding cisplatin to imatinib re-establishes tumor response following secondary resistance to imatinib in advanced chorcoma (abstract 10038). J Clin Oncol. 2007; 25:554s.22. Lee SE, Park SY. Sarcomatoid carcinoma of the small intestine: a rare and highly aggressive tumor. J Korean Surg Soc. 2012; 83:321–324. PMID: 23166892.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Laparoscopic approach in the surgical treatment of large retrorectal tumors: a short-term experience at a single tertiary center case series in Korea
- Clinicopathological features of retrorectal tumors in adults: 9 years of experience in a single institution
- A Retrorectal Neurofibroma Resected by Transsacral Approach
- Clinicopathological Features of Retrorectal Tumors in an Adult: A Case Report and Review of the Literatures
- Laparoscopic Resection of a Huge Retrorectal Tumor