J Korean Neurosurg Soc.
2020 Jul;63(4):487-494. 10.3340/jkns.2019.0191.
Postoperative Non-Pathological Fever Following Posterior Cervical Fusion Surgery : Is Laminoplasty a Better Preventive Method than Laminectomy?
- Affiliations
-
- 1Department of Neurological Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 2Department of Emergency Medicine, Gangneung Asan Hospital, University of Ulsan College of Medicine, Gangneung, Korea
- KMID: 2504643
- DOI: http://doi.org/10.3340/jkns.2019.0191
Abstract
Objective
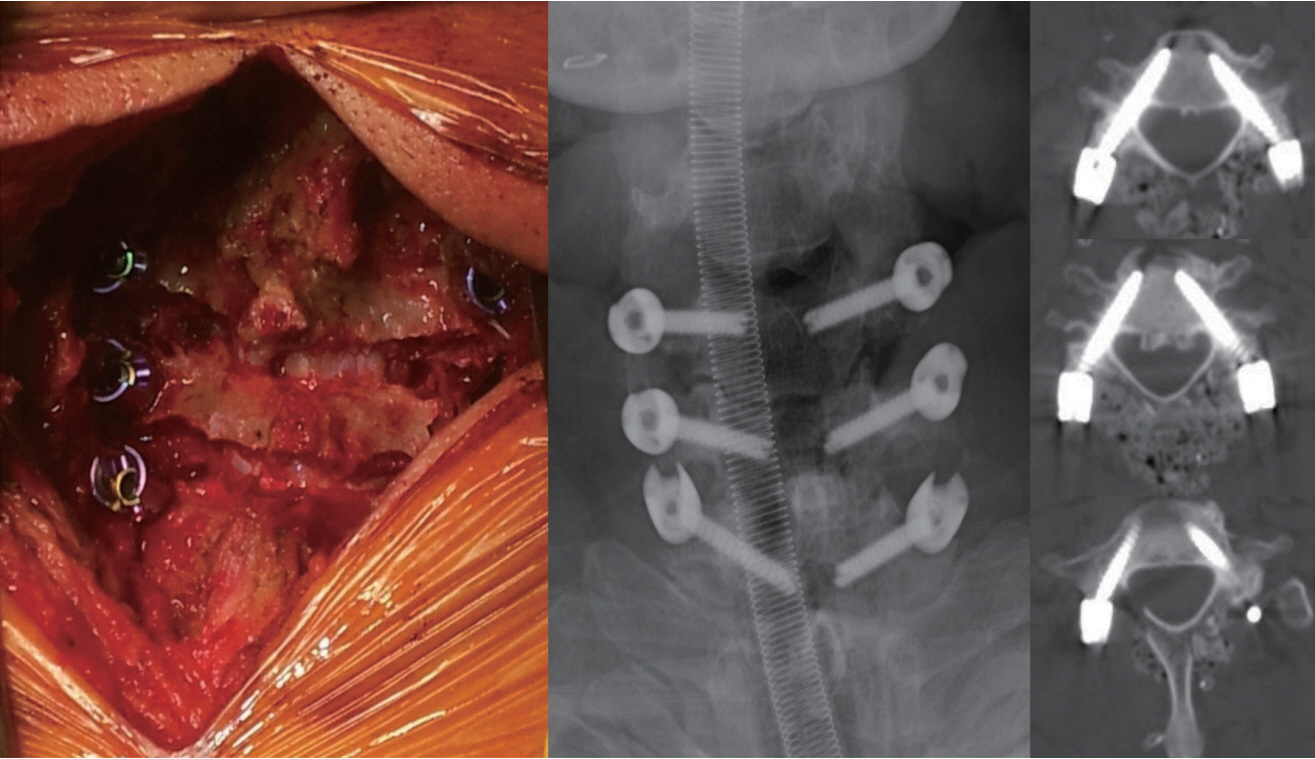
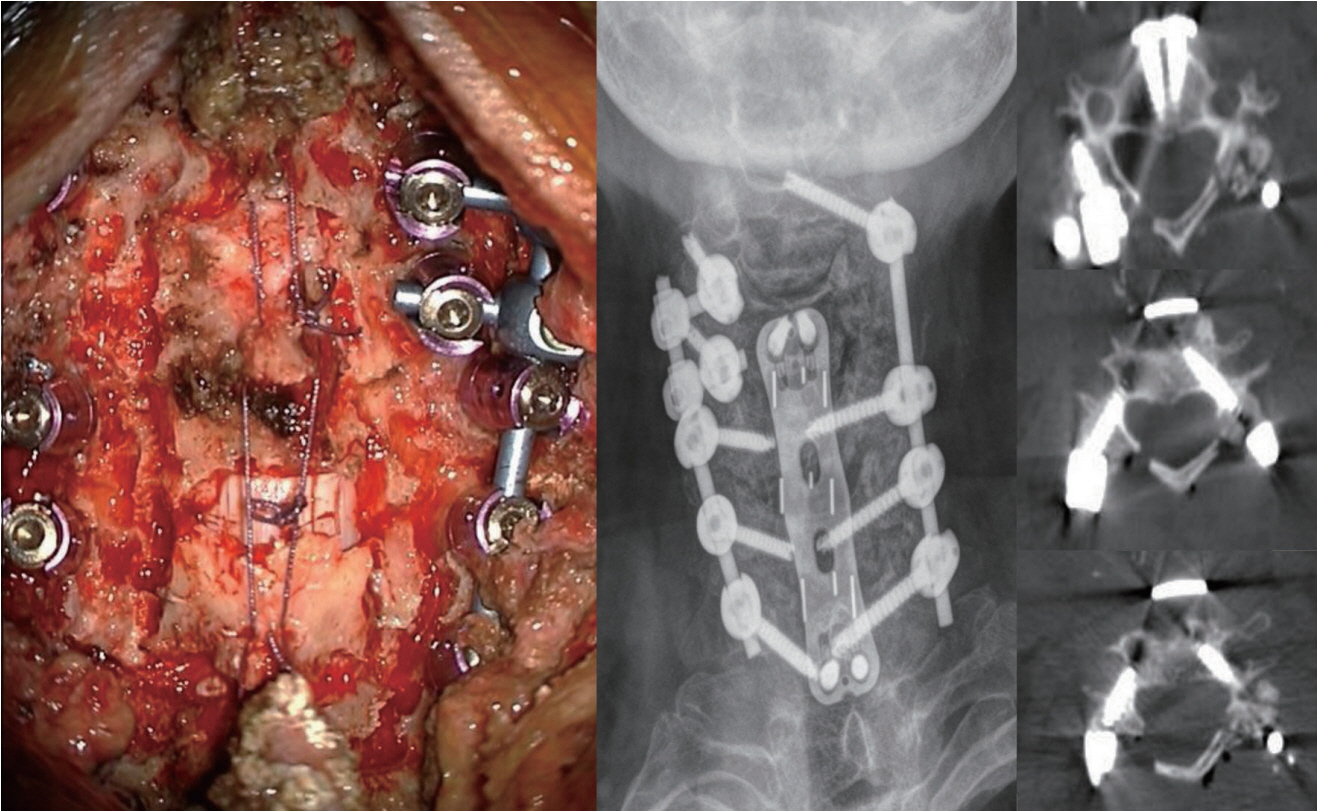
: To analyze the incidence and characteristics of delayed postoperative fever in posterior cervical fusion using cervical pedicle screws (CPS).
Methods
: This study analyzed 119 patients who underwent posterior cervical fusion surgery using CPS. Delayed fever was defined as no fever for the first 3 postoperative days, followed by an ear temperature ≥38°C on postoperative day 4 and subsequent days. Patient age, sex, diagnosis, laminectomy, surgical level, revision status, body mass index, underlying medical disease, surgical duration, and transfusion status were retrospectively reviewed.
Results
: Of 119 patients, seven were excluded due to surgical site infection, spondylitis, pneumonia, or surgical level that included the thoracic spine. Of the 112 included patients, 28 (25%) were febrile and 84 (75%) were afebrile. Multivariate logistic regression analysis showed that laminectomy was a statistically significant risk factor for postoperative non-pathological fever (odds ratio, 10.251; p=0.000). In contrast, trauma or tumor surgery and underlying medical disease were not significant risk factors for fever.
Conclusion
: Patients who develop delayed fever 4 days after posterior cervical fusion surgery using CPS are more likely to have non-pathologic fever than surgical site infection. Laminectomy is a significant risk factor for non-pathologic fever.
Keyword
Figure
Cited by 2 articles
-
Comparison between Anterior Cervical Decompression with Fusion and Posterior Cervical Fusion with Wide Facetectomy for Treatment of Severe Bony Foraminal Stenosis
Subum Lee, Dae-Chul Cho, Haemin Chon, Sung Woo Roh, Il Choi, Jin Hoon Park
J Korean Neurosurg Soc. 2021;64(4):552-561. doi: 10.3340/jkns.2020.0263.Reliability of Early Ambulation after Intradural Spine Surgery : Risk Factors and a Preventive Method for Cerebrospinal Fluid Leak Related Complications
Subum Lee, Dae-Chul Cho, Kyoung-Tae Kim, Young-Seok Lee, Seung Chul Rhim, Jin Hoon Park
J Korean Neurosurg Soc. 2021;64(5):799-807. doi: 10.3340/jkns.2020.0350.
Reference
-
References
1. Andres BM, Taub DD, Gurkan I, Wenz JF. Postoperative fever after total knee arthroplasty: the role of cytokines. Clin Orthop Relat Res. (415):221–231. 2003.
Article2. Badillo AT, Sarani B, Evans SR. Optimizing the use of blood cultures in the febrile postoperative patient. J Am Coll Surg. 194:477–487. quiz 554-556. 2002.
Article3. Blumstein GW, Andras LM, Seehausen DA, Harris L, Ross PA, Skaggs DL. Fever is common postoperatively following posterior spinal fusion: infection is an uncommon cause. J Pediatr. 166:751–755. 2015.
Article4. Chon H, Park JH. Cervical vertebral body fracture with ankylosing spondylitis treated with cervical pedicle screw: a fracture body overlapping reduction technique. J Clin Neurosci. 41:150–153. 2017.
Article5. Clark JA, Bar-Yosef S, Anderson A, Newman MF, Landolfo K, Grocott HP. Postoperative hyperthermia following off-pump versus on-pump coronary artery bypass surgery. J Cardiothorac Vasc Anesth. 19:426–429. 2005.
Article6. De Holl D, Rodeheaver G, Edgerton MT, Edlich RF. Potentiation of infection by suture closure of dead space. Am J Surg. 127:716–720. 1974.
Article7. Galicier C, Richet H. A prospective study of postoperative fever in a general surgery department. Infect Control. 6:487–490. 1985.
Article8. Garibaldi RA, Brodine S, Matsumiya S, Coleman M. Evidence for the non-infectious etiology of early postoperative fever. Infect Control. 6:273–277. 1985.
Article9. Guinn S, Castro FP Jr, Garcia R, Barrack RL. Fever following total knee arthroplasty. Am J Knee Surg. 12:161–164. 1999.10. Heller JG, Edwards CC 2nd, Murakami H, Rodts GE. Laminoplasty versus laminectomy and fusion for multilevel cervical myelopathy: an independent matched cohort analysis. Spine (Phila Pa 1976). 26:1330–1336. 2001.
Article11. Herrick DB, Tanenbaum JE, Mankarious M, Vallabh S, Fleischman E, Kurra S, et al. The relationship between surgical site drains and reoperation for wound-related complications following posterior cervical spine surgery: a multicenter retrospective study. J Neurosurg Spine. 29:628–634. 2018.
Article12. Hobar PC, Masson JA, Herrera R, Ginsburg CM, Sklar F, Sinn DP, et al. Fever after craniofacial surgery in the infant under 24 months of age. Plast Reconstr Surg. 102:32–36. 1998.
Article13. Kiragu AW, Zier J, Cornfield DN. Utility of blood cultures in postoperative pediatric intensive care unit patients. Pediatr Crit Care Med. 10:364–368. 2009.
Article14. Kwon BK, Fisher CG, Boyd MC, Cobb J, Jebson H, Noonan V, et al. A prospective randomized controlled trial of anterior compared with posterior stabilization for unilateral facet injuries of the cervical spine. J Neurosurg Spine. 7:1–12. 2007.
Article15. Lau D, Winkler EA, Than KD, Chou D, Mummaneni PV. Laminoplasty versus laminectomy with posterior spinal fusion for multilevel cervical spondylotic myelopathy: influence of cervical alignment on outcomes. J Neurosurg Spine. 27:508–517. 2017.
Article16. Lee BJ, Park JH, Jeon SR, Roh SW, Rhim SC, Jung SK. Posterior cervical muscle-preserving interspinous process approach and decompression: more minimally invasive and modified shiraishi’s selective laminectomy. World Neurosurg. 133:e412–e420. 2020.
Article17. Lee JK, Jung SK, Lee YS, Jeon SR, Roh SW, Rhim SC, et al. Analysis of the fusion and graft resorption rates, as measured by computed tomography, 1 year after posterior cervical fusion using a cervical pedicle screw. World Neurosurg. 99:171–178. 2017.
Article18. Lee S, Seo J, Lee MK, Jeon SR, Roh SW, Rhim SC, et al. Widening of the safe trajectory range during subaxial cervical pedicle screw placement: advantages of a curved pedicle probe and laterally located starting point without creating a funnel-shaped hole. J Neurosurg Spine. 27:150–157. 2017.
Article19. Livelli FD Jr, Johnson RA, McEnany MT, Sherman E, Newell J, Block PC, et al. Unexplained in-hospital fever following cardiac surgery. Natural history, relationship to postpericardiotomy syndrome, and a prospective study of therapy with indomethacin versus placebo. Circulation. 57:968–975. 1978.
Article20. Memtsoudis SG, Hughes A, Ma Y, Chiu YL, Sama AA, Girardi FP. Increased in-hospital complications after primary posterior versus primary anterior cervical fusion. Clin Orthop Relat Res. 469:649–657. 2011.
Article21. Park JH, Jeon SR, Roh SW, Kim JH, Rhim SC. The safety and accuracy of freehand pedicle screw placement in the subaxial cervical spine: a series of 45 consecutive patients. Spine (Phila Pa 1976). 39:280–285. 2014.
Article22. Sebastian A, Huddleston P 3rd, Kakar S, Habermann E, Wagie A, Nassr A. Risk factors for surgical site infection after posterior cervical spine surgery: an analysis of 5,441 patients from the ACS NSQIP 2005-2012. Spine J. 16:504–509. 2016.
Article23. Seo J, Park JH, Song EH, Lee YS, Jung SK, Jeon SR, et al. postoperative nonpathologic fever after spinal surgery: incidence and risk factor analysis. World Neurosurg. 103:78–83. 2017.
Article24. Sharp NE, Alemayehu H, Desai A, Holcomb GW 3rd, St Peter SD. Fever after redo Nissen fundoplication with hiatal hernia repair. J Surg Res. 190:594–597. 2014.
Article25. Shiraishi T, Kato M, Yato Y, Ueda S, Aoyama R, Yamane J, et al. New techniques for exposure of posterior cervical spine through intermuscular planes and their surgical application. Spine (Phila Pa 1976). 37:E286–E296. 2012.
Article26. Theuer CP, Bongard FS, Klein SR. Are blood cultures effective in the evaluation of fever in perioperative patients? Am J Surg. 162:615–618. discussion 618-619. 1991.
Article27. Varthi AG, Basques BA, Bohl DD, Golinvaux NS, Grauer JN. Perioperative outcomes after cervical laminoplasty versus posterior decompression and fusion: analysis of 779 patients in the ACS-NSQIP database. Clin Spine Surg. 29:E226–E232. 2016.
Article28. Xu R, Bydon M, Sciubba DM, Witham TF, Wolinsky JP, Gokaslan ZL, et al. Safety and efficacy of rhBMP2 in posterior cervical spinal fusion for subaxial degenerative spine disease: Analysis of outcomes in 204 patients. Surg Neurol Int. 2:109. 2011.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Laminoplasty Versus Laminectomy and Fusion for Multilevel Cervical Spondylosis
- Posterior Surgery for Cervical Myelopathy: Laminectomy, Laminectomy with Fusion, and Laminoplasty
- Radiographic and Clinical Results of C1 Laminoplasty for the Treatment of Compressive Myelopathy
- Cervical spondylotic myelopathy and radiculopathy: a stepwise approach and comparative analysis of surgical outcomes: a narrative review of recent literature
- Expansive Laminoplasty for Cervical Compression Myelopathy