Korean J Gastroenterol.
2020 May;75(5):296-299. 10.4166/kjg.2020.75.5.296.
Endoscopic Treatment of a Twisted Small Bowel Obstruction after Laparoscopic Proximal Gastrectomy with Double Tract Reconstruction
- Affiliations
-
- 1Departments of Surgery, School of Medicine, Kyungpook National University, Daegu, Korea
- 2Departments of Internal Medicine, School of Medicine, Kyungpook National University, Daegu, Korea
- KMID: 2504249
- DOI: http://doi.org/10.4166/kjg.2020.75.5.296
Abstract
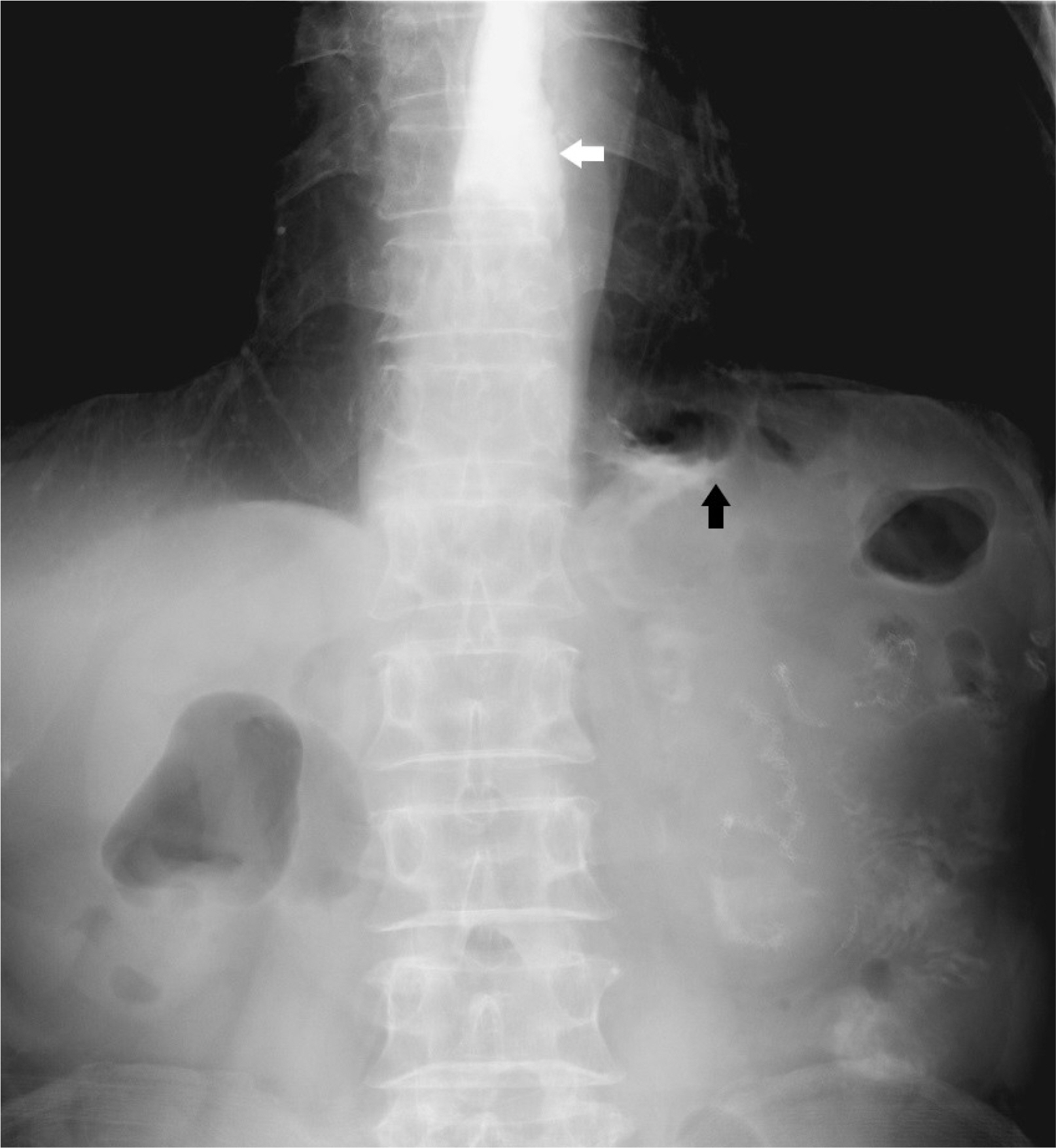
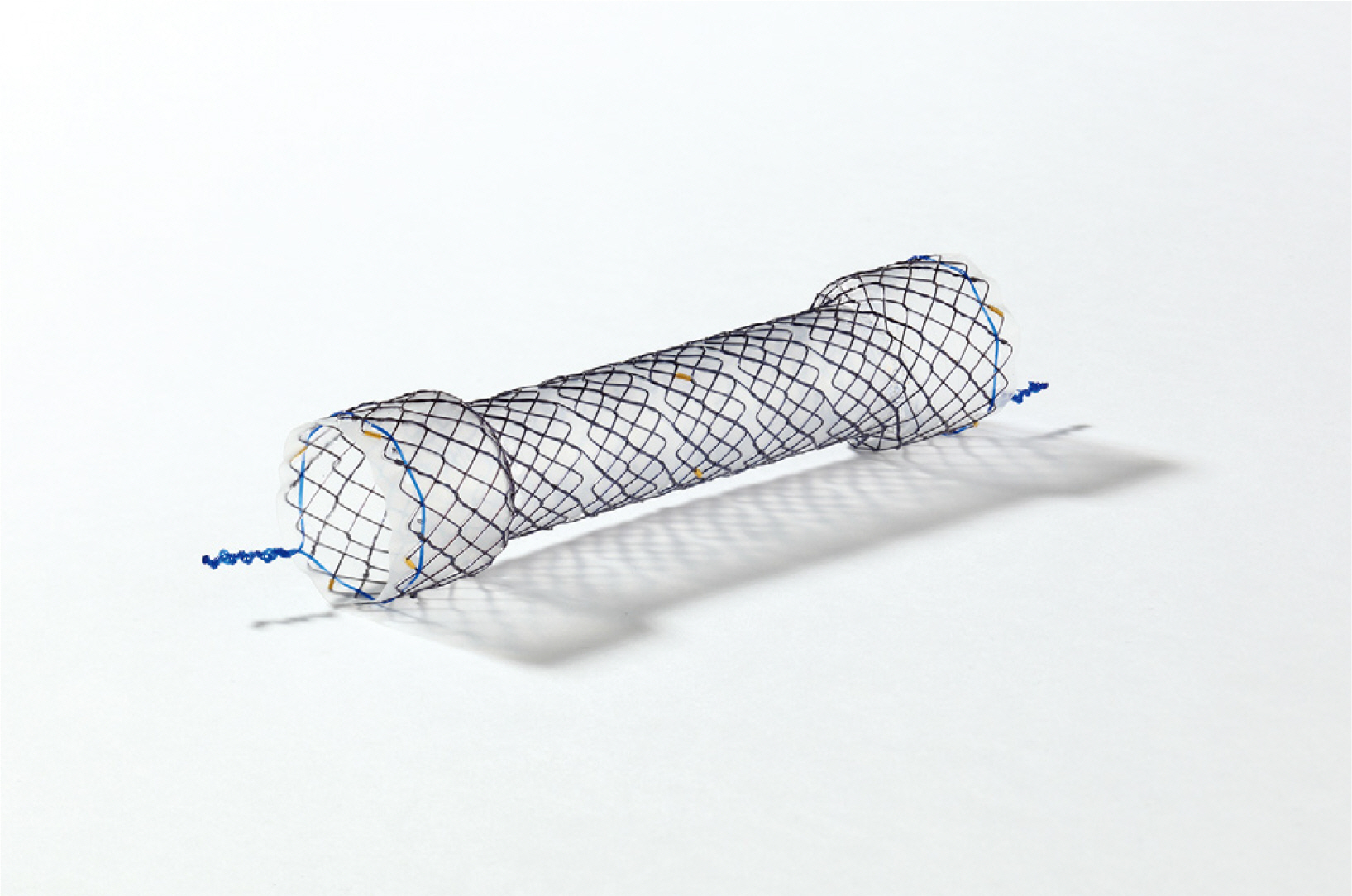
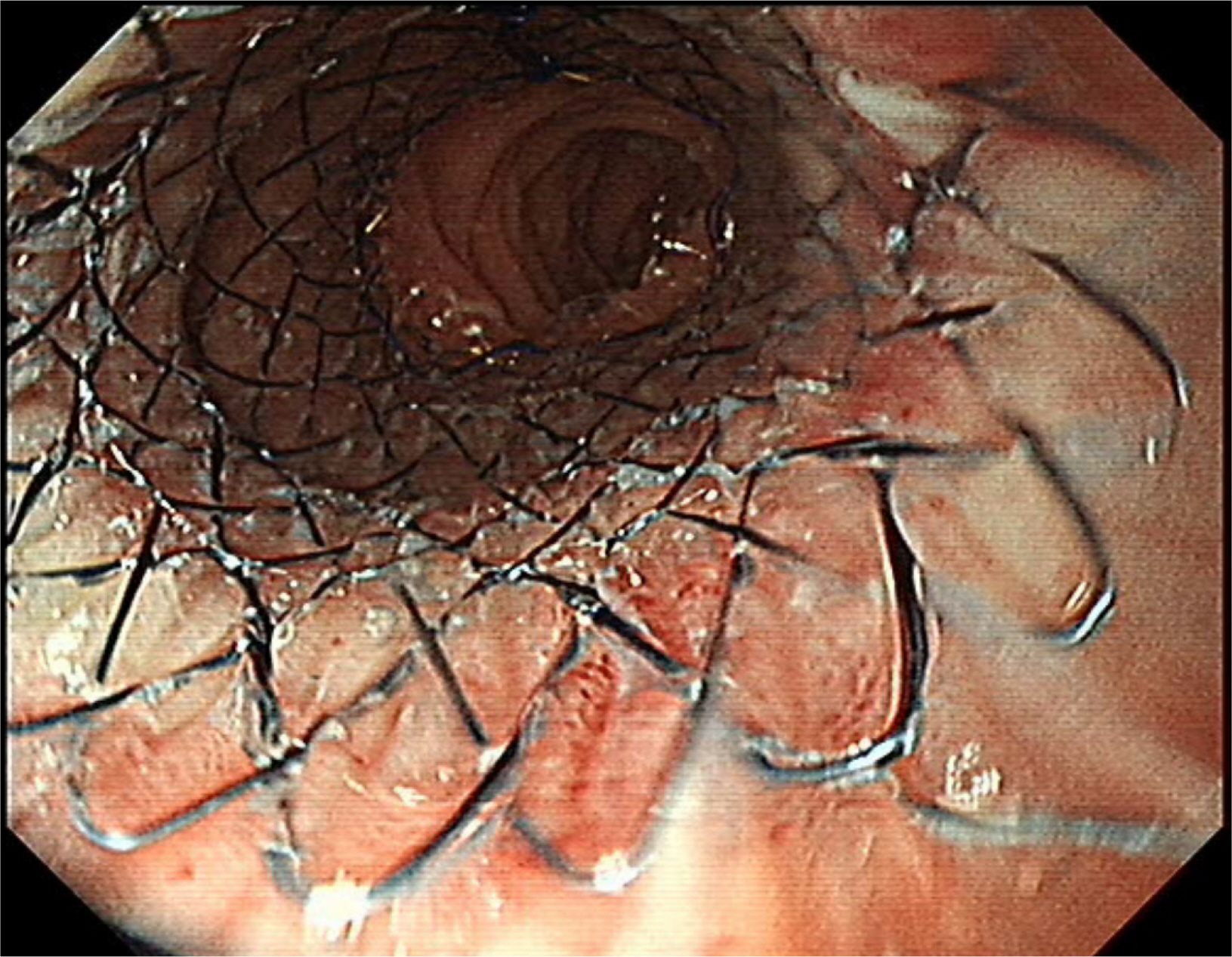
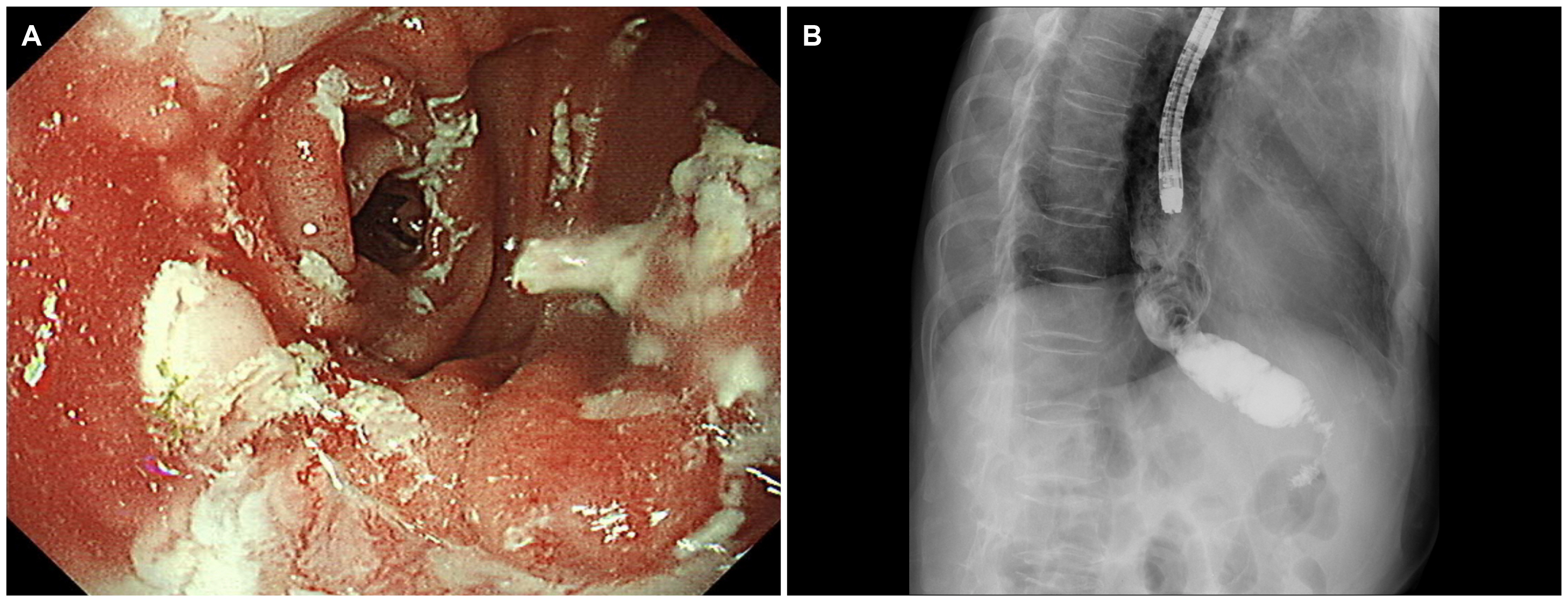
- This paper reports a case of a twisted small bowel obstruction in a 74-year-old man that occurred after a double tract reconstruction (DTR) in a laparoscopic proximal gastrectomy (PG) for early gastric cancer. The patient had inadequate oral intake and reflux symptoms for 10 days after discharge. Imaging analysis revealed a narrowed small bowel with twists between the esophagojejunostomy and gastrojejunostomy sites. A fully covered stent was placed in the narrowed small bowel for 2 weeks. The patient was then discharged after stent removal without any dietary problems. The authors’ experience shows that twisted small bowel after a DTR in PG can be treated by endoscopy.
Keyword
Figure
Reference
-
1. Japanese Gastric Cancer Association. 2017; Japanese gastric cancer treatment guidelines 2014 (ver. 4). Gastric Cancer. 20:1–19. DOI: 10.1007/s10120-016-0622-4. PMID: 27342689. PMCID: PMC5215069.2. Jung DH, Lee Y, Kim DW, et al. 2017; Laparoscopic proximal gastrectomy with double tract reconstruction is superior to laparoscopic total gastrectomy for proximal early gastric cancer. Surg Endosc. 31:3961–3969. DOI: 10.1007/s00464-017-5429-9. PMID: 28342130.
Article3. Park JY, Park KB, Kwon OK, Yu W. 2018; Comparison of laparoscopic proximal gastrectomy with double-tract reconstruction and laparoscopic total gastrectomy in terms of nutritional status or quality of life in early gastric cancer patients. Eur J Surg Oncol. 44:1963–1970. DOI: 10.1016/j.ejso.2018.08.014. PMID: 30197164.
Article4. Information Committee of Korean Gastric Cancer Association. 2016; Korean Gastric Cancer Association nationwide survey on gastric cancer in 2014. J Gastric Cancer. 16:131–140. DOI: 10.5230/jgc.2016.16.3.131. PMID: 27752390. PMCID: PMC5065942.5. Moris D, Chakedis J, Rahnemai-Azar AA, et al. 2017; Postoperative abdominal adhesions: clinical significance and advances in prevention and management. J Gastrointest Surg. 21:1713–1722. DOI: 10.1007/s11605-017-3488-9. PMID: 28685387.
Article6. Jee SR, Cho JY, Kim KH, Kim SG, Cho JH. Stent Study Group of the Korean Society of Gastrointestinal Endoscopy. 2013; Evidence-based recommendations on upper gastrointestinal tract stenting: a report from the stent study group of the korean society of gastrointestinal endoscopy. Clin Endosc. 46:342–354. DOI: 10.5946/ce.2013.46.4.342. PMID: 23964331. PMCID: PMC3746139.
Article7. Kang HW, Kim SG. 2015; Upper gastrointestinal stent insertion in malignant and benign disorders. Clin Endosc. 48:187–193. DOI: 10.5946/ce.2015.48.3.187. PMID: 26064817. PMCID: PMC4461661.
Article8. Kim SG, Yang CH. 2012; Upper gastrointestinal stent. Clin Endosc. 45:386–391. DOI: 10.5946/ce.2012.45.4.386. PMID: 23251886. PMCID: PMC3521940.
Article9. Madruga Neto AC, Brunaldi VO, Okazaki O, et al. 2018; Stent migration requiring surgical removal: a serious adverse event after bariatric megastent placement. Endoscopy. 50:E344–E345. DOI: 10.1055/a-0725-7718. PMID: 30332690.
Article10. Karagul S, Yagci MA, Ara C, et al. 2015; Small bowel perforation due to a migrated esophageal stent: report of a rare case and review of the literature. Int J Surg Case Rep. 11:113–116. DOI: 10.1016/j.ijscr.2015.04.030. PMID: 25967554. PMCID: PMC4446686.
Article11. Bae JS, Kim SH, Shin CI, et al. 2015; Efficacy of gastric balloon dilatation and/or retrievable stent insertion for pyloric spasms after pylorus-preserving gastrectomy: retrospective analysis. PLoS One. 10:e0144470. DOI: 10.1371/journal.pone.0144470. PMID: 26657405. PMCID: PMC4675538.
Article12. Shim CS, Cho YD, Moon JH, et al. 2001; Fixation of a modified covered esophageal stent: its clinical usefulness for preventing stent migration. Endoscopy. 33:843–848. DOI: 10.1055/s-2001-17326. PMID: 11571679.
Article13. Martins BC, Retes FA, Medrado BF, et al. 2014; Endoscopic management and prevention of migrated esophageal stents. World J Gastrointest Endosc. 6:49–54. DOI: 10.4253/wjge.v6.i2.49. PMID: 24567792. PMCID: PMC3930890.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Case Report: Gastrobronchial Fistula after Sleeve Gastrectomy: Treated by Laparoscopic Proximal Gastrectomy with Double Tract Reconstruction
- Single-Port Laparoscopic Proximal Gastrectomy with Double Tract Reconstruction for Early Gastric Cancer: Report of a Case
- Laparoscopic Proximal Gastrectomy as a Surgical Treatment for Upper Third Early Gastric Cancer
- Laparoscopic Adhesiolysis for Small Bowel Obstruction: Effective Alternatives or Immoderate Challenge?
- Postoperative mechanical small bowel obstruction induced by V-Loc barbed absorbable suture after laparoscopic distal gastrectomy